Melanoma David A . Jansen Chief Division Plastic Surgery Tulane University
advertisement

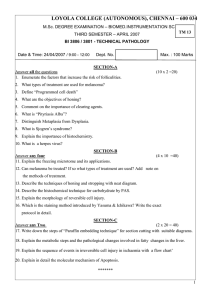
Melanoma David A . Jansen Chief Division Plastic Surgery Tulane University CC: “I have a lesion on my leg” • HPI: 25 yo Irish male who presented to clinic with a lesion on his leg. Pt stated he wasn’t sure how long it has been there “probably a couple of months.” He reported it getting bigger and changing color since he first noticed it. It also had developed an ulcer associated with it. History • PMH: multiple blistering sunburns as a teenager • PSH: RIH repair as child • Allergies: PCN • Meds: none • Social: Lifeguard, EtOH occasional, Tobacco denies, illicit +THC • FH: mother: melanoma, HTN PE • • • • • • Gen: A & O x3, NAD HEENT: PERRL, EOMI, MMM NECK: no lymphadenopathy Lungs: CTAB CV: S1S2 no mrg, no edema ABD: +BS, soft, NT, ND, no rebound, no guarding • Ext: warm, dry, 2+radial pulses • Neuro: CN II-XII intact • Skin: PE Labs • • • • • • • • • • WBC: 8.6 HBG: 14.5 HCT: 43.2 PLT: 285 Na: 140 K+: 4.3 Cl: 102 CO2: 25 BUN: 16 Cr: 0.7 Differential Diagnosis? What to do next? Biopsy Results • Superficial spreading melanoma • Breslow Depth: 2.5mm • Ulceration present Now What? Surgery • WLE with 2 cm margins and SLNB • Results: negative margins, SLNB neg Melanoma Facts • Most commonly diagnosed malignant tumors in US are cutaneous neoplasms • Most common skin cancers Basal CellCancer, Squamous Cell Cancer, and Melanoma • Melanoma accounts for 4% of skin cancer diagnosis • 75% of skin cancer deaths • 48,000 melanoma related deaths occur worldwide per year • Incidence of melanoma in Caucasians has tripled between 1980 and 2003 • 5th most common cancer in males, 7th in females • Most common on women on their legs; and males on their back Epidemiology • Life time risk: 1 in 39 Caucasian males, 1 in 58 Caucasian females • Incidence rates increasing most rapidly in older people • Overall trend is increased diagnosis at earlier stage • Mortality has declined for those 20 to 44 and increased in men over age 65 Risk Factors • UV light: strongest association for intermittent exposure and sunburn in adolescence and childhood – an analysis of more than 20 epidemiological studies indicates that people who begin using tanning devices before age 30 are 75% more likely to develop melanoma. • Phenotypic traits: fair complexion, inability to tan, blue/green eyes, blonde/red hair, freckling • Familial: 10%, multiple genes involved, ex: xeroderma pigmentosa (AR), Familial atypical multiple-mole melanoma syndrome (CDKN2) • Atypical nevi: 3 to 20 fold increase risk, ex: giant congenital nevus, greater than 100 nevi • Immunosuppression Classification • Superficial spreading: is the most common of the melanomas (70%). It usually occurs in middle age, but may occur in younger people. It can assume many shapes, and have a variety of colors, though there is usually a reddish hue • Lentigo maligna (10-15%): usually occurs in older people (>6th decade) and occurs in chronically sun exposed areas, most commonly on the face. Hutchinson Freckle This type carries the best prognosis Classification • Acral-lentiginous melanoma (5%) is most frequent in blacks and Asians. The most common site is the plantar surface of the foot; may be subungual • Nodular melanoma (15%)most often occurs in middle age and is more frequent in males. It is usually dome shaped and may ulcerate. Typically carries the worst prognosis Classification • Desmoplastic: frequently mistaken for a scar; pale and fleshy • In-transit metastases: lesions in the skin greater than 2 cm from primary lesion, arise from cells in lymphatics; poor prognosis Growth Phases Horizontal (radial): more indolent, typically cured by surgical incision alone Vertical: have increased metastatic potential; vertical growth phase melanomas may arise from radial growth phase or de novo, nodular melanoma have most vertical phase Pathophysiology Five stages of tumor progression have been suggested: – – – – – Benign melanocytic nevi Melanocytic nevi with architectural and cytologic atypia (dysplastic nevi) Primary malignant melanoma, radial growth phase Primary malignant melanoma, vertical growth phase Metastatic malignant melanoma Clinical Diagnosis • A: asymmetry- one half of lesion doesn’t match the other • B: border irregularity-ragged, notched, fuzzy • C: color-not uniform • D: diameter- greater than 6 mm • E: enlargement/evolution • Nodular – Elevated – Firm – growing Diagnosis • Histopathology necessary for diagnosis – Melanoma markers: S-100, Melan-A, HMB-45 • Initial biopsy: excisional biopsy preferred with 12 mm of normal appearing skin, orient the incision along langer’s line of stress, or parallel to long axis of extremity • Larger lesions: punch or incisional biopsy, not as accurate because the thickest part of the lesion may not be the part sampled. Breslow Depth • Total vertical height of lesion • Used to predict prognosis and determines excisional margins Breslow Thickness Approximate 5 year survival <1 mm95-100% 1 - 2 mm80-96% 2.1 - 4 mm60-75% >4 mm50% Excisional Margins In situ <1.0mm 1.1-2mm >2.0 0.5-1 cm 1 cm 1-2 cm 2 cm Clark’s Level • • • • • • • describes the level of anatomical invasion of the melanoma in the skin Five anatomical levels, and higher levels have worsening prognostic implications 1. Melanoma confined to the epidermis 2. Invasion into the papillary dermis 3. Invasion to the junction of the papillary and reticular dermis 4. Invasion into the reticular dermis 5. Invasion into the subcutaneous fat Prognosis • • • • • • • • Tumor thickness in millimeters depth related to skin structures (Clark level) type of melanoma presence of ulceration presence of lymphatic/perineural invasion presence of tumor-infiltrating lymphocytes presence of satellite lesions presence of regional or distant metastasis Surgery • Wide local excision based on Breslow depth • Sentinel lymph node biopsy should be preformed on all patients with a Breslow depth of 1mm or greater • A Breslow depth of 0.75-1.0mm may be considered for SNLB based on presence of ulceration, high mitotic rate • Use both isosulfan blue and radiolabeled colloid for SLNB • If the sentinel lymph node is negative there is a 96% chance that the rest of the nodes are negative • If positive, a regional lymphadenectomy is indicated, and consider additional metastasis Adjuvant Therapy • Interferon-alpha2b: improve disease free and overall survival rates in pts with stage IIb or III disease • IL-2 for stage IV disease • Ipilimumab: increase in median survival from 6.4 to 10 months in patients with advanced melanomas treated with the monoclonal antibody, versus an experimental vaccine • Vaccine trials for local 1.5-4mm • Radiation: typically used for palliation of bone pain or brain metastasis, may reduce rate of local reoccurance but not survival • Chemotherapy: not very useful, reports of isolated hyperthermic limb perfusion to treat in transit metastasis of extremities using TNF Staging Work-Up • Potential to metastasize to any organ: skin, subcutaneous tissue, lung, liver, brain, bone • All stages typically get LDH and CXR • LDH tests are often used to screen for metastases, although many patients with metastases (even end-stage) have a normal LDH; extraordinarily high LDH often indicates metastatic spread of the disease to the liver • Typically preformed for stage III and IV – CT – PET – MRI brain Staging Stage 0: Melanoma in Situ (Clark Level I), 99.9% Survival Stage I/II: Invasive Melanoma, 85-99% Survival -T1a: Less than 1.00 mm primary tumor thickness, w/o Ulceration and mitosis < 1/mm2 -T1b: Less than 1.00 mm primary tumor thickness, w/Ulceration or mitoses ≥ 1/mm2 -T2a: 1.00-2.00 mm primary tumor thickness, w/o Ulceration Stage II: High Risk Melanoma, 40-85% Survival -T2b: 1.00-2.00 mm primary tumor thickness, w/ Ulceration -T3a: 2.00-4.00 mm primary tumor thickness, w/o Ulceration -T3b: 2.00-4.00 mm primary tumor thickness, w/ Ulceration -T4a: 4.00 mm or greater primary tumor thickness w/o Ulceration -T4b: 4.00 mm or greater primary tumor thickness w/ Ulceration Stage III: Regional Metastasis, 25-60% Survival -N1: Single Positive Lymph Node -N2: 2-3 Positive Lymph Nodes OR Regional Skin/In-Transit Metastasis -N3: 4 Positive Lymph Nodes OR Lymph Node and Regional Skin/In Transit Metastases Stage IV: Distant Metastasis, 9-15% Survival -M1a: Distant Skin Metastasis, Normal LDH -M1b: Lung Metastasis, Normal LDH -M1c: Other Distant Metastasis OR Any Distant Metastasis with Elevated LDH Surveillance • Primary objective to identify potentially curable locoregional recurrences and second primary cancers • Stage I and II: most locoregional reoccurrences • Stage III: systemic recurrences more common • Most reoccurrences caught by PE • Stage IA recommend detailed medical history and PE every 6 to 12 months • Stage IB to III history and PE every 3 to 6 months for 3 years, every 4 to 12 mo for 2 years • Order additional studies based on symptoms Resources • Greenfield’s Surgery • The Washington Manuel of Surgery