PALLIATIVE CARE: WHAT IT IS, WHAT IT IS NOT &
advertisement

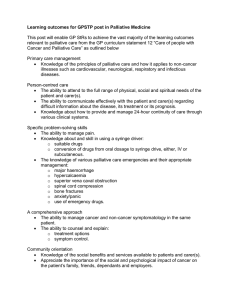
PALLIATIVE CARE: WHAT IT IS, WHAT IT IS NOT & HOW TO MAKE A DIFFERENCE Jennifer Reynolds RN, BSN, DNP-C March 12, 2015 Objectives • To define Palliative Care and its components • To differentiate Palliative Care from Hospice Care • To explain the affects of Palliative Care on health care outcomes • To recognize the stages, as well as the signs and symptoms, of approaching death • To describe the importance of spirituality in health care • To perform a spiritual assessment • To demonstrate therapeutic conversation skills surrounding EOL What is Palliative Care? • Patient and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. • Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and to facilitate patient autonomy, access to information and choice (National Quality Forum, 2013). Palliative Care Emphasizes… • Management of TOTAL pain: physical, emotional, spiritual, and social. • Symptom management: breathing, nausea, constipation, anxiety. • Spiritual and psychosocial counseling for patients and families. • Support for patients making decisions about their treatment, goals of care, and care coordination. Palliative Care vs. Hospice Palliative Care Hospice Both focus on: Quality of life Emotional, Physical, & Spiritual Support Unlike Hospice, Palliative care allows for: • Simultaneous treatment of underlying disease • Acute hospitalization, including intensive care, if needed • Palliation along side the most aggressive disease treatment Hospice vs. Palliative Care Hospice • Life expectancy of 6 months or less • Pain mgmt. to allow patients to die with dignity • Many hospice programs covered under Medicare Palliative Care • No life expectancy limit • More aggressive tx of symptoms without compromising QOL • Each item administered is typically covered through hospital; ACP and other services not yet covered Bruera, E., & Hui, D. (2010). Integrating Supportive and Palliative Care in the Trajectory of Cancer: Establishing Goals and Models of Care. Journal of Clinical Oncology, 28(25), 4013-4017. doi: 10.1200/jco.2010.29.5618 DID YOU KNOW THAT… 70 % of people say they prefer to die at home HOWEVER… 70% die in a hospital, nursing home, or long-term-care facility DID YOU KNOW… 82% of people say it’s important to put their wishes in writing HOWEVER… 23% actually do it Public Awareness About Palliative Care Very Knowledgeable 5% Knowledgeable 3% Somewhat Knowledgeable 14% N=800 Don't Know 8% Perceptions of patients’ wishes aren’t accurate Not At All Knowledgeable 70% Center to Advance Palliative Care, “2011 Public Opinion Research on Palliative Care,” https://www.capc.org/media/filer_public/18/ab/18ab708cf835-4380-921d-fbf729702e36/2011-public-opinion-research-on-palliative-care.pdf Once Informed about Palliative Care… Likelihood of Considering Palliative Care Use After Learning Its Definition n=800 70% Once informed, earlier referrals can be facilitated, as patients recognize the maximum benefit palliative care services have to offer. 63% 60% 50% 40% 29% 30% 20% 10% 6% 0% Very Likely Somewhat Likely Not too/Not at All Likely The Public’s Opinion… It is important that patients with serious illness and their families be educated about palliative care options available to them together with curative treatment. 78% Strongly Agree 95% either Agree or Strongly Agree The Public’s Opinion… Palliative care is appropriate at any age and at any stage in a serious illness, and can be provided together with curative treatment. 73% Strongly Agree 94% Either Agree or Strongly Agree Benefits of Palliative Care 1. IMPROVES QUALITY OF CARE: • Reduces symptom burden and unwanted aggressive end of life care • Lengthens end of life survival time • Improves patient care experience 2. REDUCES INPATIENT COST • Decreases LOS • Reduces cost-of-care • Frees up bed capacity 3. LOWERS TOTAL COST OF CARE • Reduces unnecessary hospitalizations and ED visits • Lowers readmission rates SUPPORTIVE STUDY: Early Palliative Care • Study done in Boston, Mass General Hospital • Background: Effect of introducing palliative medicine early after diagnosis with metastatic non-small-cell lung cancer on patient-reported outcomes and end-of-life care among ambulatory patients with newly diagnosed disease • Non-blinded, randomized controlled trial of 151 patients assigned to early palliative care integrated with standard oncologic care or standard oncologic care alone • Early palliative care group met with palliative care within 3 weeks of enrollment and at least monthly until death. • Standard care met with palliative care only if requested by the patient, family, or oncologist. Temel, J. S., Greer, J. A., Muzikansky, A., Gallagher, E. R., Admane, S., Jackson, V. A., . . . Lynch, T. J. (2010). Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine, 363(8), 733-742. doi: 10.1056/NEJMoa1000678 Early Palliative Care Study Results 120% 100% FACT-L Symptom Mgmt Scores P=0.03; n= 47, n=60 Percentage of patients with s/s of depression P= 0.01; n=47, n=57 98% Higher scores indicate fewer symptoms, better QOL 92% 80% 60% 38% 40% 16% 20% 0% Symptom Burden Symptoms of Depression Usual Care Palliative Care Early Palliative Care Study Results Patients receiving more aggressive EOL care P=0.05; n=56, n=49 Aggressive care= chemotherapy within 14 days of death, no hospice care, or admission to hospice 3 or few days prior to death Palliative Care, 33% Palliative care patients also had resuscitation preferences documented in their outpatient medical record more often than in usual care group (53% vs. 28%) Usual Care, 54% Early Palliative Care Study Results Patients’ Median Survival (Months) p=0.02; n=56, n=49 Palliative Care 11.6 Usual Care 0 2 4 Patients who received palliative care lived an average of 2.7 months longer 8.9 6 8 10 12 14 SUPPORTIVE STUDY: Outpatient Palliative Care • Study conducted at Kaiser Permanente Colorado and Kaiser Permanente Hawaii from 2002 and 2004 • Study included 297 homebound, late-stage COPD, CHF, or cancer patients with a prognosis of approximately one year or less who were randomly assigned to usual care or usual care plus an inhome palliative medicine program. • In-Home Palliative Medicine Lowers Utilization, Increases Patient Satisfaction SUPPORTIVE STUDY: Outpatient Palliative Care • In-Home Palliative Care Services Offered: • Patients are offered palliative care in 12 months rather than the 6 month prognosis with Hospice Care • Symptom management is the focus, similar to Hospice, however they do not have to forgo curative care. • Patients are assigned to Palliative Care Physicians who coordinates care from a variety of providers (specialists to PCP). They received home visits from Palliative Care physicians while maintain their regular relationship with PCP. • Interdisciplinary team approach utilizing a physician, nurse, and social worker with expertise in symptom management and biopsychosocial intervention. • Comprehensive education and discussions focus on identifying goals of care and the expected course of the disease and expected outcomes. SUPPORTIVE STUDY: Outpatient Palliative Care • Usual Care • Medicare guidelines for home health care criteria which also include acute care, primary care services, and hospice care (when indicated). • Patients were treated for their symptoms when they presented them to their attending physicians Study Results: Outpatient Palliative Care Brumley, R., Enguidanos, S., Jamison, P., Seitz, R., Morgenstern, N., Saito, S., & ... Gonzalez, J. (2007). Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. Journal Of The American Geriatrics Society, 55(7), 993-1000. doi:10.1111/j.1532-5415.2007.01234.x CONCLUSION • In-home palliative care program, may lead to significant total reduction in both ED utilization and hospitalizations for terminally ill patients. • Significant cost savings • Total cost of care per patient was nearly $8000 lower for those in the palliative care group. • Moreover pts receiving outpatient palliative care were more satisfied than usual care group. • In addition to keeping patients out of ED and hospital, outpatient palliative care can also transition care home and stay there comfortably. Quality Caring Rounds at HF Wyandotte: Project Design • To implement interdisciplinary “quality caring” rounds Monday through Friday for a one month pilot on the ICU. • To assess the impact of interdisciplinary rounds on patients’ goals of care. • To analyze whether palliative care triggers and advance care planning triggers, implemented on admission to the ICU, affect the palliative care consult rate, as well as quality of care. • MDRs included intensivist, charge nurse, CM, SW, nutritionist, Respiratory Therapist, Pharmacist, palliative care NP, infection control specialist, and pastoral care (depending on the day) Pastoral Care Consults 30 24 25 20 • In April, 2/9 were direct referrals from rounds. 15 10 8 10 9 • In May, 16/24 (67%) were established from rounds 5 0 ICU referrals Feb March April • There is a strong correlation between spiritual care and patient-family satisfaction in the ICU May Hospital Indicators With a 15 day and a 26 day outlier PROGRAM GROWTH • Over the past 10 years, growth in palliative care programs have been rapid. • Since 2000, the number of hospitals with inpatient palliative care team has increased by nearly 150%. • Right now, 66% of all hospitals with greater than 50 beds have palliative care teams in place. Source: “Growth of Palliative Care in U.S. Hospitals, 2012 Snapshot,” Center to Advance Palliative Care Traditional Model of Palliative Care This is when Palliative and/or Hospice services are introduced Conceptual Shift for Palliative Care--A Continuum of Care D I A G N O S I S Source: Snyder S, et al., “Physician Knowledge, Attitude, and Experience with Advance Care Planning, Palliative Care, and Hospice,” Am J Hosp Palliat Care, 30, no. 5 (2013): 419-424; Physician Executive Council interviews and analysis A Fundamental Shift Usual Care Goals of Care Palliative Care Delayed until EOL is near Established early in the disease trajectory Treatment Strategy Includes primarily curative treatments Includes a combination of curative and symptom-focused tx Service Utilization Pursues curative tx even when lowyield, high-cost, and burdensome for patient Pursues treatments that align with patient goals Signs & Symptoms of the Actively Dying Patient Early Stages— Months • Less communicative • Less active • Sleep or doze more • Eat and drink less • Withdraw from people and activities previously found pleasurable • Relive memories, especially childhood memories One to Two Weeks Prior to Death • Temperature fluctuations that may leave the skin cool, warm, moist, or pale • Increased pain • Changes in sleep-wake patterns, constant fatigue • Decreased intake of food and liquids • Decline in bowel and bladder output • Inability to heal or recover from wounds or infections • Increased swelling (edema) of either the extremities or the entire body • Congested breathing One to Two Weeks (cont’d) • Increased restlessness, confusion, agitation, inability to stay content in one position and insisting on changing positions frequently (exhausting family and caregivers) • Patient reports seeing persons who had already died • Patient states that he or she is dying • Patient requests family visit to settle "unfinished business" and tie up "loose ends" Imminent Death—Days or Hours • Coma: If not already unconscious, patient may drift in and out of consciousness • There may be little or no bladder or bowel activity. • The patient will stop eating and drinking • Pain may be more difficult recognize at this time Grimacing, scowls, groans. Need to be assessed frequently and managed. • Eyes may tear or become glazed over. Imminent death (cont’d) • Pulse may become irregular, thready, weak (difficult to detect) • Body temperature will drop and the skin of the lower extremities and hands will become mottled, a bluish-purple color. Death usually comes within 24 hours. • “Death rattle” • Breathing patterns will become irregular by gasping starts and stops and will become slow until it eventually stops. “Death Rattle” • Noisy breathing associated with wet secretions retained in the respiratory tract in actively dying patients. • Salivary secretions d/t impaired swallowing reflexes (Type I); or • Bronchial secretions that accumulate over days d/t inability to cough (Type II) • Occurs in approximately 44%-56% of dying patients in the last 24-48 hours of life. • Standard treatment: Antimuscarinic medications (anti-cholinergics) • Scopalimine, hyoscyamine, Robinol, and atropine. • Increased risk of side effects: sedation, confusion, delirium, hallucinations. • Are they really effective?? Cochrane review found no evidence that any intervention for death rattle is superior to a placebo Wee, B., & Hillier, R. (2008). Interventions for noisy breathing in patients near to death. Cochrane Database of Systematic Reviews(1). “Death Rattle” (cont.) • Expert opinions have concluded that the death rattle does not distress patients • Causes high rates of distress in medical professionals which inadvertently affect families perceptions • Staff find it difficult to not respond when there is treatment available • Focusing on treatment with meds results in poor outcomes because symptoms typically remain and if there are delays in meds, families may become upset. • Organizations are looking at refocusing education at reassuring families that this type of breathing is harmless. Heisler, M., Hamilton, G., Abbott, A., Chengalaram, A., Koceja, T., & Gerkin, R. (2013). Randomized Double- Blind Trial of Sublingual Atropine vs. Placebo for the Management of Death Rattle. Journal of Pain and Symptom Management, 45(1), 14-22. Spirituality • Spirituality is defined as, “the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and/or to the significant or sacred.” • Spirituality and religion are not congruent although they do overlap. • Spirituality is about the individual and finding one’s path whereas religion is an organized system of beliefs, rituals, or rules. • You can be spiritual, depending on religion to find your path. • You may be religious, identified as part of a particular religion, but not necessarily spiritual. Spiritual Care in Health Care • Integral to any patient-centered health care system • Based on honoring dignity • Spiritual distress treated the same as any other medical problem • Spirituality should be considered a “vital sign” • Improved Quality • In a survey given to patients with advanced illnesses to determine what was important to them at EOL, being at peace with God was ranked highest, along with pain control (Steinhauser et al., 2000) • Spiritual support is correlated to improved quality of life as well as decreased use of aggressive care at EOL (Balboni, Paulk, & Balboni, 2010) Role of Spirituality in Health Care • Manages interactions to support patient and family expression of spiritual needs and strengths and cultural practices • Creates environment that allows integration of dialogue about spiritual issues within care experience • May use questions such as: What is the meaning of this illness to you and for your life? What lessons would you want to share? What strength have you called upon as you go through this illness Do you have any spiritually specific care parameters you wish us to observe? • What do you worry about most? • • • • Spiritual Assessment: FICA • Do you consider yourself spiritual or religious? • Do you have beliefs that help you cope with stress? • Are you part of a spiritual/ religious community? • Is this of support to you? • Is there a group of people you really love or who are important? F: Faith, Belief, Meaning I: Importance and Influence C: Community A: Address/ Action in Care • What importance does your faith/belief have in your life? • Have your beliefs influenced you in how you handle stress? • How should the healthcare provider address these issues in your healthcare? Source: Hospice and Palliative Nurses Association (HPNA) Spiritual Distress • What is Spiritual Distress? • Spiritual distress is a disruption in one’s beliefs or value system. It affects a person’s entire being. It shakes the basic beliefs of one’s life • What are the Signs/Symptoms of Spiritual Distress? • • • • • • • • • Questioning the meaning of life Afraid to fall asleep at night or other fears Anger at God/higher power Questions own belief system Feels a sense of emptiness; loss of direction Talks about feelings of being left by God/higher power Seeking spiritual help Questions the meaning of suffering Pain and other physical symptoms can be expressions of spiritual distress as well Source: Hospice and Palliative Nurses Association (HPNA) Addressing Spiritual Distress • Symptoms to Report • Any symptoms of spiritual distress • Side effects of medications • Report behaviors that are out of character for the patient at distressing times • Talk about suicide • Known history of spiritual distress • Not caring for self or life in general • Sudden rejection or neglect of previous practices or beliefs • CONSULT PASTORAL CARE if not already consulted Spiritual Distress and the Practitioner’s Role • Encourage open discussions • Presence and listening to the patient’s story and concerns are the most important responses to spiritual distress • Provide ways to honor rituals and ways of life (utilize your pastoral care!) • Do not say, “I know how you feel” because you don’t Improving the Quality of Spiritual Care as a Dimension of Palliative Care: Journal of Palliative Medicine, October 2009 Formulation of a Spiritual Treatment Plan • Spiritual care coordinator • Documentation of spiritual support resources • Follow up evaluations • Discharge plans of care • Bereavement care Examples of Intervention of a Spiritual Treatment Plan • Compassionate presence • Reflective listening/query about important life events • Support patient sources of spiritual strength • Open ended questions • Inquiry about spiritual beliefs, values and practices • Life review, listening to the patient’s story • Targeted spiritual intervention • Continued presence and follow up Advance Directives/Advance Care Planning Conversations Starters Who do you want — or not want — to be involved in your care? Who would you like to make decisions on your behalf if you're not able to? When you think about the last phase of your life, what's most important to you? Are there important milestones you'd like to meet if possible? (birth of your grandchild or your 80th birthday.) Would you prefer to be actively involved in decisions about your care? Or would you rather have your doctors do what they think is best? Do you have any particular concerns about your health? About the last phase of your life? Are there circumstances that you would consider worse than death? (longterm need of a breathing machine or feeding tube, or not being able to recognize your loved ones.) Empathetic Statements • Acknowledge the difficulty of having a critically ill loved one • Acknowledge the difficulty of surrogate decision making • Show empathy to the impending loss of a loved one Curtis, J. R., & White, D. B. (2008). Practical Guidance for Evidence-Based ICU Family Conferences. Chest, 134(4), 835–843. doi:10.1378/chest.08-0235 Identify Commonly Missed Opportunities • Listen and respond to family members • Acknowledge and address family emotions • Explore and focus on patient values and treatment preferences • Explain the principle of surrogate decision making to the family • Affirm non-abandonment of patient and family Curtis, J. R., & White, D. B. (2008). Practical Guidance for Evidence-Based ICU Family Conferences. Chest, 134(4), 835–843. doi:10.1378/chest.08-0235 Where Do We Go From Here? Everyone serves a purpose in providing care for patients, however the actions each person performs are different Pastoral Care Palliative Care Team Administrator Patient Ancillary Services Nurse Physician