REPORT ON ORGANIZATION AND IMPLEMENTATION OF PHASE-I CLINICAL
advertisement

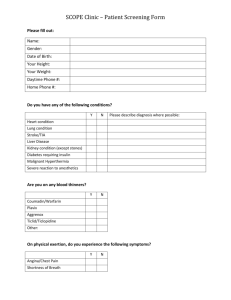
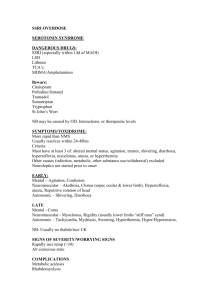
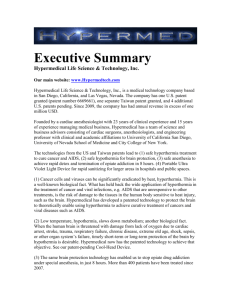
REPORT ON ORGANIZATION AND IMPLEMENTATION OF PHASE-I CLINICAL TRIAL OF HYPERTHERMIA AND RADIATION CANCER TREATMENTS IN INDIA Krishna Ramya Cherukuri BTech, Jawaharlal Nehru Technology University, India, 2007 Vijaya Chandra Yadav BTech, Jawaharlal Nehru Technology University, India, 2005 PROJECT Submitted in partial satisfaction of the requirements for the degree of MASTER OF SCIENCE in ELECTRICAL AND ELECTRONIC ENGINEERING at CALIFORNIA STATE UNIVERSITY, SACRAMENTO SPRING 2010 REPORT ON ORGANIZATION AND IMPLEMENTATION OF PHASE-I CLINICAL TRIAL OF HYPERTHERMIA AND RADIATION CANCER TREATMENTS IN INDIA A Project by Krishna Ramya Cherukuri Vijaya Chandra Yadav Approved by: __________________________________, Committee Chair Preetham B. Kumar, Ph.D. __________________________________, Second Reader Warren D. Smith, Ph.D. ____________________________ Date ii Students: Krishna Ramya Cherukuri Vijaya Chandra Yadav I certify that these students have met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the project. ______________________, Graduate Coordinator ________________ Preetham B. Kumar, Ph.D. Date Department of Electrical & Electronics Engineering iii Abstract of REPORT ON ORGANIZATION AND IMPLEMENTATION OF PHASE-I CLINICAL TRIAL OF HYPERTHERMIA AND RADIATION CANCER TREATMENTS IN INDIA by Krishna Ramya Cherukuri Vijaya Chandra Yadav This report details the different stages of the recently initiated Phase I clinical trial of a new modality of cancer treatment in India. The clinical trial involves the addition of hyperthermia or heat treatment to existing treatment techniques such as radiation or chemotherapy, with the aim to improving patient response. Earlier studies have showed that the combined protocols can double the patient response. The current trial involved 14 patients in a palliative mode of treatment, and the report covers the planning, organization, and carrying out of the clinical trials. Currently, the trial has been initiated at one cancer center in India, but will be extended to another center shortly. This report can be used as a base on how the hyperthermia treatment is conducted practically and also includes details about the procedure and protocol followed for hyperthermia treatment together with radiation and chemotherapy treatment. In this collaborative project, Krishna Ramya Cherukuri and Vijaya Chandra Yadav, individually contributed to the background research on hyperthermia treatment and its practical application in the clinical trial. iv Krishna Ramya Cherukuri did background research on hyperthermia treatment and its usage and in the selection of different kinds of equipment used in the treatment. Vijaya Chandra Yadav did research on practical clinical trials involving combined hyperthermia and radiation or chemotherapy protocols and developed recommendations regarding how the hyperthermia treatment should be implemented in India, taking into account the demographics and cancer spread in that country. _______________________, Committee Chair Preetham B. Kumar, Ph.D. _______________________ Date v ACKNOWLEDGMENTS Behind every achievement lies an unfathomable sea of gratitude to those who actuated it, without whom it would never come into existence. It is with a deep sense of gratitude and honor that we convey our thanks to our advisor, committee chair, and graduate coordinator, Dr. Preetham Kumar, for his exemplary guidance, monitoring, and constant encouragement throughout the course of this project. We are very indebted to Dr. Warren D. Smith for patiently reviewing our work as our second reader. We would also like to take this opportunity to thank the considerate faculty and staff of Electrical and Electronic Engineering Department who have encouraged us throughout our curriculum. Last but not the least, we thank our parents and all those friends who implicitly or explicitly helped in the success of our project with their constructive criticism and encouragement. vi TABLE OF CONTENTS Page Acknowledgements ............................................................................................................ vi List of Tables ..................................................................................................................... ix List of Figures ..................................................................................................................... x Chapter 1. INTRODUCTION ....................................................................................................... 1 2. BACKGROUND ON HYPERTHERMIA TREATMENT OF CANCER ................... 4 2.1 Description of Hyperthermia .................................................................................. 4 2.2 Microwave Hyperthermia ....................................................................................... 4 2.3 Methods of Hyperthermia ....................................................................................... 5 2.4 Effects of Hyperthermia........................................................................................ 11 2.5 Advantages of Hyperthermia ................................................................................ 12 2.6 Health Factors that Increase Risk of Hypterthermia ............................................ 14 2.7 Disadvantages of Hyperthermia ........................................................................... 14 3. PLANNING OF HYPERTHERMIA TRIAL IN INDIA ........................................... 16 4. EQUIPMENT DEVELOPMENT AND DELIVERY ................................................ 20 4.1 Initial Installation of Equipment ........................................................................... 20 4.2 Initial Tests on Equipment .................................................................................... 23 4.3 Experimental Goals............................................................................................... 27 5. TREATMENT PROTOCOL AND PROCEDURE .................................................... 28 5.1 Patient Screening and Pre-treatment Guidelines ................................................. 28 vii 5.2 Radiation and Localized Hyperthermia Protocol .................................................. 29 5.3 Patient Follow-up Procedure ............................................................................... 33 6. PATIENT DATA COLLECTION AND PRECAUTIONS………………………...37 6.1 Guidelines for Collection and Organization of Patient Response ....................... 37 6.2 Study Stage 1: Patient Screening ........................................................................ 38 6.3 Study Stage 2: Treatment Ethics and Patient Consent Form .............................. 41 7. HYPERTHERMIA CLINICAL TRIAL SCHEDULE AND DETAILS ................... 49 7.1 Initial Feasibility Study ........................................................................................ 49 7.2 Grant Funding ...................................................................................................... 50 7.3 Schedule of the Clinical Trials ............................................................................. 50 8. CONCLUSIONS…...………………………………………………………………..52 References ......................................................................................................................... 54 viii LIST OF TABLES Page 1. Table 1. Readings for Different Temperatures…………...……………...............26 2. Table 2. Radiation and Hyperthermia (RT + HT) Protocol………………….......35 3. Table 3. Chemotherapy and Hyperthermia (CT + HT) Protocol ………………..36 4. Table 4. Patient Profile and Responses…………………………………….…….37 5. Table 5. Patient Side Effects...…………………………………………………...38 ix LIST OF FIGURES Page 1. Figure 2.1. Scheme of Local Hyperthermia……………......……………………...7 2. Figure 2.2. Applicator Types of Local Hyperthermia……..…………….………..8 3. Figure 2.3. Schematic for Aquatherm System……………...…...……………… 11 4. Figure 3.1. News Report in the Hindustan Times, Dated September 18, 2007… 18 5. Figure 3.2. News Report in the Hindustan Times, Dated January 4, 2010…..…..19 6. Figure 4.1. Diathermy Unit…………………...………………………………… 20 7. Figure 4.2. Thermometry Unit…………...……………………………………... 21 8. Figure 4.3. Experimental Setup……………...…...……………………………...25 9. Figure 5.1. Integrated Microwave Hyperthermia System………………………..31 x 1 Chapter 1 INTRODUCTION In this report, the goal is to present the details of the recently conducted clinical trial in India involving the combination of hyperthermia or heat treatment with conventional radiation or chemotherapy for cancer treatment. It provides the details of the different stages of the clinical trial, including the planning, organization of funding for the project, acquisition of the hyperthermia therapy equipment, and finally, the actual small-scale trial. The existing treatments for cancer are radiation and chemotherapy, and the present trial includes hyperthermia or heat treatment before the conventional treatment. Previous studies indicate that hyperthermia together with radiation or chemotherapy can double the patient’s response [1]. The type of clinical trial was a phase-I clinical trial conducted on 14 patients in a palliative mode of treatment in one of the cancer treatment centers in India. Palliative trials usually are conducted for new forms of treatment, such as hyperthermia, and patients selected for this kind of trial are those who have not responded satisfactorily to conventional forms of treatment. Generally, hyperthermia is the heat process that raises the temperature of the cancerous area, and this rise of the body temperature weakens or kills the cancer [2]. Additionally, the heating makes the tumors more sensitive to subsequent radiation or chemotherapy. There are different varieties of hyperthermia or heat treatment available to increase the temperature of the affected area of the body [2]. 2 In the Department of Electrical and Electronic Engineering microwave laboratory at California State University, Sacramento (CSUS), much research has been conducted previously on hyperthermia, and many experiments have been conducted by students to model the heating process using clay, as clay closely resembles human tissues [1]. Additionally, students developed efficient treatment-planning software which utilizes the computed tomography (CT) scan of the patient to precisely plan the focusing of the microwave beam on the tumor area. This report is organized into eight chapters. Chapter I introduces the report, and Chapter II explains the background of the hyperthermia treatment. Chapters III and IV describe the planning of the clinical trial in India and development of the equipment. Chapter V explains the treatment protocol and procedure, and Chapter VI details the patient data collection and precautions. Chapter VII details the clinical trial schedule, and Chapter VIII presents the conclusions. In this collaborative project, Krishna Ramya Cherukuri carried out the background research on hyperthermia treatment and different types of equipment available for cancer treatment using the hyperthermia modality. Additionally, she researched hyperthermia treatment combined with radiation and chemotherapy treatment for effective increase in patient response. For example, it is often debated if hyperthermia should be given before or after conventional radiation treatment or at the same time. We concluded from earlier clinical trials in Europe and U.S. that it is more effective to give hyperthermia first, followed by radiation or chemotherapy. 3 Vijaya Chandra Yadav researched how hyperthermia treatment should be implemented in India by taking into account the economic and human demographics in that country. Additionally, he also researched the existing cancer centers in India and helped to narrow down the list of hospitals which could be candidate centers. Ultimately, five centers were identified. From these, two centers were selected on the basis of budget and logistics. Currently, the hyperthermia trial is underway at one cancer center in Northern India, and a second trial will start at a cancer center in Southern India during the summer of 2010. 4 Chapter 2 BACKGROUND ON HYPERTHERMIA TREATMENT OF CANCER 2.1 Description of Hyperthermia Hyperthermia is the general term that originates from Greek and means overheating [3]. Specifically, “hyperthermia” refers to raising the temperature of a cancer tumor for a limited period of time. It is a procedure for treating cancer in which the tissue temperatures in the tumor are raised above normal temperature (98.6 °F), usually in the range of 103-108 °F. The main challenge in hyperthermia is accurate and precisely targeted heating of the tumor area, and this is primarily achieved by the following two engineering tools [4]: Hardware, such as microwave antenna systems which can provide narrow focused beams for tumor heating [4]. Software to accurately plan the tumor heating based on patient scan data [4]. 2.2 Microwave Hyperthermia Microwave hyperthermia is rapidly evolving as a fourth modality in the fight against cancer, along with surgery, radiation, and chemotherapy. This form of cancer treatment utilizes a narrow microwave beam to heat the tumor volume to a temperature of approximately 42 °C with minimal energy delivery to neighboring healthy tissue, which is one of the main challenges in hyperthermia technology. Potentially, this application 5 can be achieved by using a phased array of apertures or dipoles to generate and control the beam focus within the near-field treatment region [5]. Microwave hyperthermia has been used generally in combination with chemotherapy and/or radiation, because hyperthermia enhances the tumor's response to radio/chemotherapy [6]. 2.3 Methods of Hyperthermia Several methods of hyperthermia are currently under study, including local, regional, and whole-body hyperthermia. 2.3.1 Local Hyperthermia Local hyperthermia treatment (heat applied to a very small area, such as a tumor) is a well-established cancer treatment method with a simple basic principle: If a rise in temperature to 106 ºF can be obtained for one hour within a cancer tumor, the cancer cells will be destroyed [7]. 2.3.1.1 Methodology of Local Hyperthermia In this method, heat is applied to a small area, such as a tumor, using various techniques that deliver energy to heat the tumor. To achieve internal heating, one of several types of sterile probes may be used, including thin, heated wires or hollow tubes filled with warm water; implanted microwave antennae; and radiofrequency electrodes [7]. Heating rods and ultrasound also are used for this process [6]. Depending on the tumor location, there are several approaches to local hyperthermia: 6 “External approaches are used to treat tumors that are in or just below the skin. External applicators are positioned around or near the appropriate region, and energy is focused on the tumor to raise its temperature” [6]. Intraluminal or endocavitary methods may be used to treat tumors within or near body cavities, such as the esophagus or rectum. Probes are placed inside the cavity and inserted into the tumor to deliver energy and heat the area directly [6]. Ultrasound is used to administer local hyperthermia to solid tumor cancers. This technique uses ultra-high frequency sound waves to produce heat within the tumor. Ultrasound is more easily focused than other energy modalities and can be applied to tumors located from the skin to 8 cm within your body. This technique allows the treatment of tumors unreachable by other external modalities. Ultrasound does not require the use of radio wave shielding devices to protect medical personnel during treatment [7]. Interstitial techniques are used to treat tumors deep within the body, such as brain tumors. Radiofrequency ablation (RFA) is a type of interstitial hyperthermia that uses radio waves to heat and kill cancer cells [6]. 7 2.3.1.2 Components Used in Hyperthermia Various applicators used for local hyperthermia treatment are spiral, waveguide, horn, current sheet, and compact applicators. Figure 2.1 shows the components used in hyperthermia. Figure 2.1. Scheme for Local Hyperthermia [1] 8 Figure 2.2 shows the applicator types for local hyperthermia, such as waveguide applicator, spiral applicator and current sheet applicator. Figure 2.2. Applicator Types for Local Hyperthermia, such as (a) Waveguide Applicator; (b) Spiral Applicator; and (c) Current Sheet Applicator [1] 2.3.2 Regional Hyperthermia Regional hyperthermia for cancer uses focused electromagnetic energy to warm the tissue in and around the tumor to between 40 and 43 °C [8]. Heat is focused directly on the organ or area affected by the tumor, unlike whole-body hyperthermia, in which the entire body is heated [9]. The affected area is positioned between two applicators. Radio waves 9 directed by computer are concentrated on the tumor, and the temperature is raised to 107 to 111 °F. This temperature is maintained in the tumor tissue for approximately 60 to 90 min. A temperature check is carried out either directly within the tumor, or externally by means of a radiometer which, unlike invasive temperature monitoring, carries no risk of infection or of spreading cancer cells [9]. Various approaches may be used to heat large areas of tissue, such as a body cavity, organ, or limb [6]. These approaches are described below. Deep tissue approaches may be used to treat cancers within the body, such as cervical or bladder cancer. External applicators are positioned around the body cavity or organ to be treated, and microwave or radiofrequency energy is focused on the area to raise its temperature [6]. Regional perfusion techniques can be used to treat cancers in the arms and legs, such as melanoma, or cancer in some organs, such as the liver or lung [6]. A warmed solution containing anticancer drugs is used to bathe, or is passed through the blood vessels of, the tissue or organ containing the tumor. Some of the patient’s blood is removed, heated, and then pumped (perfused) into the region that is to be heated internally [7]. Continuous Hyperthermic Peritoneal Perfusion (CHPP) is a procedure in which the abdominal cavity is bathed in warm fluid that contains anticancer drugs [9]. It is used to treat cancers within the peritoneal cavity (the space within the abdomen that contains the 10 intestines, stomach, and liver), including primary peritoneal mesothelioma and stomach cancer. During surgery, heated anticancer drugs flow from a warming device through the peritoneal cavity. The peritoneal cavity temperature reaches 106–108 °F [6]. 2.3.3 Whole-Body Hyperthermia Whole-body hyperthermia is used to treat metastatic cancer that has spread throughout the body. This treatment can be accomplished by several techniques, such as extracorporeal technologies that raise the body temperature to 107–108 °F, including the use of thermal chambers (similar to large incubators) or hot water blankets [6]. The patient lies in a special, insulated chamber that is gradually heated by means of a special infrared radiation reflector system until the desired body temperature is reached [9]. The patient reaches target temperature within approximately 1.3 hr, is maintained at 107.2 °F for 1 hr, and then cools for 1 hr [1]. Small probes may be inserted into the tumor under a local anesthetic to monitor the temperature of the affected tissue and surrounding tissue [1]. Depending on the patient and the temperature obtained, the whole procedure takes 3 to 5 hr, including the recovery phase. Many patients have an intravenous drip running during the treatment session, which allows the addition of whatever medications may be necessary. During the whole period, the patient is continuously and intensively monitored to check if pulse frequency, heart rate, blood pressure, ECG, respiratory rate, body core temperature, and various blood tests are normal [9]. 11 The aquatherm system (Figure 2.3) is used for whole body hyperthermia. It is an isolated moisture-saturated chamber which has steamed tubes (122 – 140 °F) on its inner sides in which the patient is positioned. The whole body is exposed to long-wavelength infrared wave emission. The cabin where the patient is kept contains hot water tubes and a temperature of (140 °F) is maintained inside. After a systemic temperature of 107.2 °F is achieved, the patient is thermally isolated with blankets [1]. Figure 2.3. Schematic for Aquatherm System [1] 2.4 Effects of Hyperthermia Hyperthermia has both pros and cons, but beneficial effects overcome the cons of it. Hyperthermia effectiveness is related to: 12 Temperature: Temperature monitoring is a must throughout the treatment. Doctors use local anesthesia and insert small needles or tubes with tiny thermometers into the treatment area to monitor the temperature. Imaging techniques, such as CT is used to make sure that probes are positioned properly [6]. Length of Treatment: Length of treatment is very important during the treatment, because if it exceeds the desired time, it may result in damaging the unaffected areas and kill the good cells [6]. Cell and Tissue Characteristics: Success of treatment depends on how well cells and tissues react to high temperature. If cells and tissues do not react, then applying more and more temperature may result in destroying good cells [6]. Studies reveal that the combination of hyperthermia and radiation therapy results in effective and better treatment. The response rate for radiation without heat is 35%, and the response rate of hyperthermia combined with radiation is 75%. As the research gains momentum, more reasons for the use of hyperthermia are continuously being identified [1]. 2.5 Advantages of Hyperthermia Direct destruction of malignant cells: The temperature can be increased enough to kill the unwanted bacteria, viruses, and cancer cells without the need for surgery [6]. 13 Hyperthermia is used for general activation of the immune system and better recognition of tumor cells by the immune system [3]. An increase in body temperature above normal levels consistently for a period of time helps draw toxins out of the body, kill harmful bacteria and viruses, clean clogged pores, increase circulation and enhance immune system [6]. Hyperthermia is used for improving the effectiveness of radiation. The local hyperthermia with radiation is better than radiation alone for breast cancer reoccurrence, melonoma metastases, relapsed and lymph node metastases from head and neck cancer, and glioblastomas [3]. Hyperthermia is useful in treatments such as healing muscle aches, pains, and injuries after accidents [6]. Hyperthermia combined with radiation is more useful to treat deep seated tumors than radiation alone. It is used in the treatment of upper and lower respiratory tract infections, bladder problems, bronchitis, pneumonia, urinary tract infections such as cystitis, sinusitis, and other conditions of the lungs and body cavities. It is also helpful in controlling bleeding and treating prostatic hypertrophy and psoriasis [6]. Hyperthermia is used for improving the effectiveness of chemotherapy [3]. Hyperthermia is synergistic with chemotherapeutic drugs and with ionizing radiation, is easy to control, and has low host toxicity [10]. Hyperthermia is used in drug delivery. Several studies have shown that the delivery of monoclonal antibodies is enhanced by a factor of 12 using hyperthermia, with resultant 14 improvement in anti-tumor effects. The spread of carried chemotherapy drugs into the tissues of liposome is increased considerably with higher temperature when compared to that under normal temperature [6]. Hyperthermia improves the therapeutic index of TBI (total body irradiation), not only by increased neoplastic cell kill, but also by inhibiting the expression of radiationinduced damage to the normal cell population [6]. 2.6 Health Factors that Increase Risk of Hyperthermia Health factors which may increase risk include: Poor circulation of blood may result in cancer. Inefficient sweat glands and changes in the skin caused by the normal aging process, heart, lung and kidney diseases, as well as any illness that causes general weakness or fever, high blood pressure, or other conditions that require changes in diet [11]. Overweight or underweight and drinking alcoholic beverages [11]. 2.7 Disadvantages of Hyperthermia Hyperthermia may result in various hot spots due to regional differences in tissue characteristics, which in turn may result in burns, blisters, discomfort, or pain [6]. 15 Perfusion techniques can cause tissue swelling, blood clots, bleeding, and other damage to the normal tissues in the perfused area; however, most of these side effects are temporary [6]. During loco-regional hyperthermia, a local heating or hot sensation may occur. Local redness, tiredness, and mild fevers may occur [3]. Whole-body hyperthermia can cause more serious side effects, including cardiac and vascular disorders, but these effects are uncommon. Neuropathies, diarrhea, nausea, vomiting, abnormal or lethal blood coagulation, damages to liver tissues and kidneys, and brain hemorrhaging and some seizures are commonly observed after whole-body hyperthermia [6]. Extracorporeal systemic hyperthermia can give side effects such as frequent persistent neurophites, damages to liver or kidneys, abnormal blood coagulation, and brain hemorrhaging and seizures [1]. In spite of the above disadvantages, hyperthermia is popular and successful, as these side effects are temporary, and uncommon. They can be avoided by being careful and precise during treatment and by controlled clinical procedures. 16 Chapter 3 PLANNING OF HYPERTHERMIA TRIAL IN INDIA Cancer is one of the deadliest diseases, and it is projected to be the leading cause of death in 2010. It is also projected that by 2030, there will be 20 to 26 million new diagnoses and 13 to 17 million deaths all over the world [4]. Any means of treatment is welcomed in reducing the number of cancer deaths and treating the suffering patients. Microwave hyperthermia is a promising tool against cancer. It involves the use of microwave or RF (radiofrequency) antennas to heat the tumor area, which increases the sensitivity of the treatment volume to subsequent radiation or chemotherapy [4]. Research conducted on microwave hyperthermia at CSUS, which resulted in improved antenna hardware design and efficient treatment planning software which helps to target the tumors precisely [4] [1]. This research finally led to the planning of two new clinical trials for hyperthermia with the help of a CSUS Research and Creative Activity (RCA) grant and another grant from the International Union Against Cancer (UICC), based in Switzerland [1]. The clinical trial effort is underway at one cancer center in India, which has one of the highest numbers of cancer patients in the world. The clinical trial at one of the centers, Mahavir Cancer Sansthan (MCS), Patna, India, was started in January, 2010, with an 17 initial number of 14 patients, and the other trial at Christian Medical College Hospital, Vellore, India, will start in July, 2010. The first clinical trial, which was initiated in January, 2010, included 14 patients on palliative treatment, with 11 patients receiving radiation and hyperthermia, while the remaining three patients received radiation and chemotherapy. Media reports appeared in the press during the course of the planning and course of the clinical hyperthermia trials in India. Figures 3.1 and 3.2 show two media reports appeared in the Hindustan Times, which is the second largest English newspaper in India, with a circulation of 6.3 million readers [1]. 18 News report in the Hindustan Times, dated September 18, 2007 Figure 3.1. News Report in the Hindustan Times, dated September 18, 2007 19 News report in the Hindustan Times, dated January 4, 2010 Reproduced from Hindustan Times Online: From right: Dr. Jitendra Singh, Director, Dr. Vineeta Jain, Radiation Chief, Dr. Preetham Kumar Figure 3.2. News report in the Hindustan Times, dated January 4, 2010 20 Chapter 4 EQUIPMENT DEVELOPMENT AND DELIVERY 4.1 Initial Installation of Equipment 4.1.1 Equipment List Two important pieces of equipment are used in the hyperthermia treatment in the clinical trials in India: the diathermy unit, which generates the RF power, and the thermometry unit, which monitors the temperature in the patient treatment area. 27 MHz short wave diathermy unit (shown in Figure 4.1) Figure 4.1. Diathermy Unit 21 Infrared/Probe thermometry unit (shown in Figure 4.2) Figure 4.2. Thermometry Unit The infrared thermometer can measure the temperature on the treatment area from a distance, in order to avoid interference between the RF source and the thermometer infrared radiation. 4.1.2 Choosing a Location for the Equipment The diathermy and thermometry units are not very large and will not occupy much space. The diathermy unit is about the size of a small refrigerator and can stand on its own; however, it requires a 500-W power outlet. The thermometry unit is the size of a calculator and can be placed on a table close to the patient [12]. 22 There are two options for placing these two units: Option 1: Place diathermy equipment and thermometry unit in the same room as radiation equipment In this option, the patient can remain in the same room when hyperthermia is given, followed by radiation. This option provides less discomfort to the patient and also maximizes the effect of the hyperthermia [12]. Option 2: Place diathermy equipment and thermometry unit in a different room than radiation equipment In this option, the patient can receive hyperthermia in a separate room called “Hyperthermia room,” and then be taken very quickly to the radiation room. The advantage of this method is that a separate room also can accommodate the equipment for whole body hyperthermia, and also a computer for records [12]. 4.1.3 Powering Up the Equipment Power up the diathermy equipment, and check if the working light comes on. If the disc electrodes are not attached to the unit, screw on the electrodes. These two electrodes are shown in Figure 4.1. Switch on the thermometry system (check if batteries are installed), and check if it displays room temperature. 23 4.2 Initial Tests on Equipment Before starting with the clinical trials, ensure that the following items have been completed: 4.2.1 Permission from Review Board Ensure that the necessary permissions have been obtained from the Institutional Review Board (IRB). This protocol has been already approved by the CSUS Human subjects Committee, but it should also be approved by the MCS review board [12]. 4.2.2 Selection of Patients for the Hyperthermia and Radiation Trial Select an appropriate number of patients for the radiation and hyperthermia clinical trial and also a similar number of patients for the control arm that will receive radiation alone. 4.2.3 Patient Consent Forms Ensure that patients have been advised, and patient consent forms have been signed according to the center guidelines. A sample consent form is provided in the main radiation and hyperthermia protocol document [12]. 24 4.2.4 Initial Tests on Equipment The equipment must be calibrated before it can be used on the patient. The calibration setup is shown in Figure 4.3. The sample material for testing can be foam or thermocol material. Initially, keep the material dry, and turn on the diathermy power. It will take some time to start the heating process. Set the power level at half the maximum power by using the power control knob. Set the timer for 30 min., and record the temperature rise every 5 min. The temperature can be recorded by the infrared thermometer or by putting a needle probe in the material. It is recommended to compare the readings by both infrared and needle probe mechanisms. 25 Thermocol (dry and wet) Power Temperature measurement Figure 4.3. Experimental Setup Tabulate the readings as shown in Table 1. If there is no significant temperature change after 30 min., then set the timer for another 30 min., and record for a maximum of 60 min. [12]. 26 Table 1. Readings for Different Temperatures Time (min.) Temperature material), °C (Dry Temperature (Wet Material), °C 0 5 10 15 20 25 30 35 40 45 50 60 Repeat the same experiment by adding water on the upper surface of the thermocol or foam material. 4.3 Experimental Goals 27 You should observe a higher temperature rise in the wet material than in the dry material. The target temperature to aim for is 42 °C or 107 °F. However, in the experiment, if you reach a temperature of 98-100 °F, it is satisfactory, since the human body is lossier, and will heat to a higher temperature [12]. 28 Chapter 5 TREATMENT PROTOCOL AND PROCEDURE This chapter describes the protocol for hyperthermia treatment in the clinical trials in India. As discussed previously, hyperthermia is used along with radiation treatment (HT+RT) and chemotherapy treatment (HT+CT). First, the proposed localized hyperthermia (HT) treatment study is described. This study will involve HT, in conjunction with radiation (RT), since HT is expected to significantly enhance the effects of radiation on the patients. However, in order to accurately compare the effects of HT, as an adjuvant to radiation, a control study is performed on an equal number of patients with radiation treatment only. The complete procedure of the proposed study is given below. It has been derived from experiences of earlier clinical studies, specifically [1320]. 5.1 Patient Screening and Pre-Treatment Guidelines Initially, a pool of 50 patient volunteers will be selected at each clinical trial center who satisfy all the following conditions: The patients fit the health profile specified in the screening guidelines given in Section 6.2. The patients have responded poorly or not at all to previous radiation treatment. 29 The patients have been informed of the details of the RT + HT procedure and are willing to undergo the procedure. Patients participating in this study should have willingly signed a consent form provided in Section 6.6.3. Patients should not be allowed to receive prior chemotherapy within 4 weeks of study enrollment or radiation for 2 weeks prior to study enrolment. Patients are required to have pre-therapy baseline physical exams, computed tomography (CT) scans, and CA-125 levels. 5.2 Radiation and Localized Hyperthermia Protocol The combined radiation (RT) and localized hyperthermia (HT) treatment protocol is detailed below in four steps: Step 1: Pre-HT Treatment Guidelines Patients should have been screened and advised according to the guidelines given in Section 5.1. Patients should not be allowed to receive prior chemotherapy within 4 weeks of study enrollment or radiation for 2 weeks prior to study enrolment. Patients are required to have pre-therapy baseline physical exams, computed tomography (CT) scans, and CA-125 levels. 30 Step 2: HT-RT Treatment Cycle The localized hyperthermia (HT) treatment session is focused mainly on raising the patient’s application area temperature to the designated level of 42.0 °C, and maintains it for about 60 min., during one cycle of the study. The main guidelines for each cycle of HT-RT treatment are as follows: Apply the heat treatment (HT) using the integrated hyperthermia system shown in Figure 5.1. Maintain a temperature of 42.0 °C on the patient tumor area for a period of 30 min. Apply the radiation treatment (RT) of 1.5-2.0 Gy (or the normal dosage) to the patient tumor area. Temperature should be monitored in the tumor volume by using either temperature probes or infrared temperature equipment, shown in Figure 5.1. The temperature can be raised or lowered by controlling the power output of the diathermy equipment, whose maximum power is 500 W, and is equipped with digital timer, audio alarm and patient control switch. Step 3: HT- RT Treatment Schedule A total of 50 patients can be divided into two categories for the proposed phase I trials. The first category, which is the control arm, consists of patients that will receive radiation only, according to the existing schedule at the cancer center. The second 31 category, which is the trial arm, will receive the combined radiation and hyperthermia treatment according to the schedule shown below. 27 MHz DIATHERMY SYSTEM INFRARED THERMOMETER INFRARED/PROBE THERMOMETER POWER CONTROL MICROWAVE HEATING TREATMENT PLANNING SOFTWARE CT DATA TEMPERATURE MONITOR PATIENT CT SCAN FILES Figure 5.1. Integrated Microwave Hyperthermia System 32 CONTROL ARM (25 patients) Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Day 7 Day 8 Day 9 Day 10 Day 11 Day 12 Day 13 Day 14 Day 15 Day 16 Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation Radiation TRIAL ARM (25 patients) Radiation + Hyperthermia Radiation Radiation Radiation + Hyperthermia Radiation Radiation Radiation + Hyperthermia Radiation Radiation Radiation + Hyperthermia Radiation Radiation Radiation + Hyperthermia Radiation Radiation Radiation + Hyperthermia The hyperthermia is given for the trial arm only at 2-day intervals in order to prevent thermotolerance of the tissue. Thermotolerance means that the tissue becomes tolerant to the heat treatment. Step 4: Post-HT Treatment Guidelines Patients can be treated with normal saline 500 to 1000 ml as needed to maintain systolic blood pressures greater than 90 mm Hg. 33 Patients should be observed for 20-24 hr prior to being discharged. 5.3 Patient Follow-up Procedure After each patient has undergone the complete treatment, the following guidelines are recommended for the follow-up study: After the complete treatment, each patient should undergo a routine physical exam and CT scan to evaluate the status of the disease. The following categories are defined: Complete response (CR) is defined as the disappearance of all clinically detectable malignant disease, without the development of new malignant lesions for at least 4 weeks. Partial response (PR) is defined as a 50% or greater decrease in tumor size lasting for at least 4 weeks, without an increase in the size of any area of known malignant disease, or appearance of new areas of malignant disease. Stable disease (SD) is defined as no significant change in measurable disease for at least 8 weeks, no increase in the size of any area of known malignant disease, or appearance of new areas of malignant disease. Progressive disease (PD) is defined as a significant increase in the size of lesions present at the start of therapy, or the appearance of new metastatic lesions. 34 Each patient should have a routine physical exam once every month to check the status of his/her condition. At each exam, the status of disease should again be classified as CR, PR, SD or PD. This periodic exam should continue at least for one year, to determine the progress of disease and effectiveness of the combined hyperthermia and radiation treatments. 35 Protocol Tables for Radiation & Hyperthermia and Chemotherapy & Hyperthermia Protocols Table 2. Radiation and Hyperthermia (RT + HT) Protocol RADIATION AND HYPERTHERMIA (RT + HT) PROTOCOL Patient Name: __________ M/F _______ Id No.: ____________ Age ________ Treatment Date Cycle Time Started Time Ended HT + RT HT RT HT RT Maximum Maximum Temperature Power (for HT) or Setting Radiation Dose (RT) HT RT HT RT HT RT HT RT HT RT HT RT HT RT HT RT HT RT HT RT RT only RT only HT + RT RT only RT only HT + RT RT only RT only HT + RT RT only RT only Type of Cancer 36 Table 3. Chemotherapy and Hyperthermia (CT + HT) Protocol CHEMOTHERAPY AND HYPERTHERMIA (CT + HT) PROTOCOL Patient Name: ________ M/F _______ Id No.: ____________ Age ________ Treatment Date Cycle Time Started Time Ended HT + CT HT CT HT CT Maximum Maximum Temperature Power (for HT) or Setting Chemotherapy Dose (CT) HT CT HT CT HT CT HT CT HT CT HT CT HT CT HT CT HT CT HT CT CT only CT only HT + CT CT only CT only HT + CT CT only CT only HT + CT CT only CT only Type of Cancer 37 Chapter 6 PATIENT DATA COLLECTION AND PRECAUTIONS 6.1 Guidelines for Collection and Organization of Patient Response Data The suggested guidelines for collection of patient data for the clinical trials in India are shown in Table 4. It is also advisable to make a table listing the side-effects of the HT + RT, as suggested in Table 5. Table 4. Patient Profile and Responses Patient Age No. Prior (years) Therapies Number TTP of HT + (days) RT cycles Survival Response (days) (CR, PR, SD, PD) Note: CR – Complete Response, PR – Partial Response, SD – Stable Disease, PDPartial Disease, HT – Localized Hyperthermia, RT – Radiation, TTP – Time to Progression 38 Table 5. Patient Side Effects Name of side Percent side effect effect Grade 1 2 3 4 Discomfort Fat necrosis Blood pressure Skin blisters Ulcers Infection Bleeding 6.2 Study Stage 1: Patient Screening The patient screening guidelines are based on those used in earlier clinical studies [18 25]. The main factors are given below. 39 6.2.1 Disease Characteristics Histological confirmed localized carcinoma Measurable and evaluable disease 6.2.2 Patient Characteristics Age: 18 and over Sex: Both male and female Life expectancy: At least 3 months Cardiovascular: o Normal cardiovascular system o Resting ventricular ejection fraction greater than 40% o No prior myocardial infarction o No symptomatic coronary artery disease o No unstable blood pressure 40 o No thromboembolic disease Neurologic: o No seizures or other CNS disorders o Negative computerized tomographic scan of brain Pulmonary: o FEV_1 greater than 70% of predicted o Arterial pressure of oxygen greater than 60 mm Hg on room air with appropriate pressure of carbon dioxide and pH values o No history of cardiopulmonary or respiratory disease Other: o No other serious concurrent medical illness o No diabetes mellitus 6.2.3 Prior Concurrent Therapy Chemotherapy: Prior chemotherapy allowed 41 Radiotherapy: Prior radiotherapy allowed Surgery: Not specified 6.3. Study Stage 2: Treatment Ethics and Patient Consent Form The following guidelines must be observed to comply with regulations for the conduct and monitoring of the proposed hyperthermia clinical trial study; they also represent sound clinical and research practice: 6.3.1 Principles of Informed Consent In seeking informed consent, the following information shall be provided in a language understandable to the patient: o A statement that the hyperthermia clinical trial study involves research; an explanation of the purposes of the research and the expected duration of the participation o A description of the procedures to be followed; and identification of any procedures which are experimental. 42 o A description of any possible side effects that the patient could experience due to the proposed hyperthermia treatment. o A description of any benefits to the subject or to others which may reasonably be expected from the research. o A disclosure of appropriate alternative procedures or courses of treatment, if any, that may be advantageous to the patient. o A statement describing the extent, if any, to which confidentiality of records identifying the subject will be maintained and that notes the possibility that regulatory authority will inspect the records. o For this proposed research, which involves minimal risk, an assurance that medical treatment will be provided for any pain, discomfort, or other side effects listed in the treatment protocol. o An explanation of whom to contact for answers to pertinent questions about the research and research subject's rights, o A statement that participation is voluntary, that refusal to participate will involve no penalty or loss of benefits to which the subject is otherwise entitled, and that the subject may discontinue participation at any time without penalty or loss of benefits to which the subject is otherwise entitled. 43 o A statement that significant new findings developed during the course of the study which may relate to the subject's willingness to continued participation will be provided to the subject. o A patient or his legally authorized representative must give consent to participate in this study. The consent must be witnessed and dated, and retained by the investigator as part of the study records. A copy must be given to the patient. This form must also be prepared and signed by each subject and retained as part of the required study records. A copy must also be given to the patient. 6.3.2 Patient Care o Every effort will be taken by the clinical trial center staff and research supervisor to cause minimal pain or discomfort to the patient during the clinical trial study. o The clinical trial center will provide all necessary medical treatment for any possible side effects that might occur during the clinical trial study. o Patient condition and side effects will be monitored continuously during the clinical trial study, and a written record will be made for every patient. o Follow-up examination of the patient will be made for a specified period after the clinical trial study to assess the response of each patient to the hyperthermia treatment. Written record of follow-up progress will be made. 44 6.3.3 Patient Consent Form I, .......................................................................................................... state that I am..............years of age and I wish to participate in the following research clinical study being conducted by ………………………………………………(Hospital/Institution name). The supervisor of this research is Dr. …………………., and I understand that I may contact him/her if there are any questions. His/her contact details have been provided to me as below: Dr. …………………. Room No. ………….. Telephone: …………… E-mail: ……………….. The purpose of this clinical study is to investigate the effects of localized hyperthermia, or heat treatment as an addition to traditional radiation therapy, for cancer treatment. The primary aim is to evaluate the improvement in tumor response by application of the combined hyperthermia and radiation treatment, as compared to radiation treatment alone. The typical course of treatment is described at the end of this form. The investigational procedure is localized hyperthermia. My doctors have discussed the nature of this disease and the results of accepted treatment. It is hoped that I will benefit 45 from this treatment, but it is not guaranteed to be curative. My doctors have also discussed minor personal risks involved in this procedure, primarily pain or bruising at the site where heat is applied or temperature probes are inserted. I will have probes in muscle, close to the treatment area, to monitor temperature at 42 °C. During the procedure the temperature at the tumor site will be raised to 42 °C (108 °F) for 60 min., and this procedure will be accompanied or followed by radiation. I understand that I will return weekly, and then monthly for further examination, testing, and treatment. I understand I will receive accepted medical care if required, even if I do not participate in this study. I understand that all these procedures are not guaranteed cures for cancer, and that should I agree to participate, I will be foregoing the opportunity for these alternative treatments only while I participate in this study. I understand I am free to withdraw from this protocol at any time without prejudicing continuing medical care. I have a right to privacy and all information obtained in connection with this study and that can be identified with me will remain confidential. I understand that clinical and laboratory data collected on me will be used in analyzing the results of localized hyperthermia. 46 Information may be released to appropriate IRB and authorities. The results of this study may be published in scientific journals without identifying me by name. Every effort will be made to prevent injury that could result from this research. Compensation for injuries as a result of participating in this study is not available except as may be required by law. My signature below is to certify that I have read this document, have had a full opportunity to discuss it with my doctors, and consent to localized hyperthermia. I understand that I may ask further questions at any time and that I may have a copy of this document. Please initial each page of the consent form and sign below. Witness: Date: Volunteer: Date: I have explained the preceding to the patient. This consent form includes no exculpatory language through which the patient is made to waive any legal right or to release the investigator from liability for any negligence. 47 Research Supervisor: o Date: 6.3.4 Institutional Review Board (IRB) o A copy of the proposed consent form must be submitted to the local IRB together with the protocol for approval. o A copy of the IRB-approved consent form must be submitted to the study monitor prior to study entry. Each subject's signed consent form must be kept on file by the investigator for inspection at any time. o This study must be approved by an appropriate IRB. o Significant changes to the hyperthermia and radiation protocol, as well as a change of principal investigator, must also be approved by the IRB and documentation of this approval provided to the study monitor. o Records of the IRB review and approval must be kept on file by the investigator and are subject to inspection at any time. These records must be maintained for a minimum of 2 years following the completion date of the project. 48 o Periodic status reports must be submitted to the IRB at least yearly, as well as notification of study completion or termination. A copy of these reports must be sent to the study monitor. o The investigator must maintain an accurate and complete record of all submissions to the IRB. o A sponsor representative may conduct site visits to the investigation facilities for the purpose of monitoring the various aspects of the study. 6.3.5 Publications and Dissemination of Results The investigator is free to publish the results of the study at any time, in any language or paper, magazine, journal, etc., subject to the following guidelines: Published material should include results of clinical trial study only, without identifying any patient involved in the study. However, relevant information such as age, sex, and cancer history of the patient could be included in the publication. 49 Chapter 7 HYPERTHERMIA CLINICAL TRIAL SCHEDULE AND DETAILS 7.1 Initial Feasibility Study The hyperthermia clinical trials were initially planned at five cancer centers in India: 1. Tata Memorial Hospital, Mumbai, Maharashtra State, India (Dr. Purvish Parikh). 2. Mahavir Cancer Sansthan , Patna, Bihar State, India (Dr. Vineeta Goel). 3. Jawaharlal Nehru Cancer Hospital Research Centre, Bhopal, Madhya Pradesh State, India (Dr. R. K. Panday). 4. Dharamshila Cancer Hospital & Research Centre, Delhi, India (Dr. Dinesh Singh). Christian Medical College, Vellore, Tamil Nadu State, India (Dr. Joseph Chacko/Dr. SubhashiniJohn). The names of the doctors are given within parenthesis. All these centers are affiliated with the Indian Cooperative Oncology Network (ICON), which is a cancer network group that includes more than 100 cancer centers in India. However, due to funding and logistic reasons, two centers were chosen from among the five centers for an initial hyperthermia trial. If these were successful, then the treatment modality could be extended to other centers. 50 The two centers were: 1. Mahavir Cancer Sansthan, Patna, Bihar State, India 2. Christian Medical College, Vellore, Tamil Nadu State, India 7.2 Grant Funding As is the case for any project, funding is essential to provide equipment, personnel time, and also travel to coordinate the clinical trials. Initially, it was thought to try funding sources in India, such as the Indian Council of Medical Research (ICMR). However, a start-up grant from the RCA program at CSUS in 2008, gave the initial funding to obtain two diathermy units (which would provide the hyperthermia or heat treatment on the patient). These units were installed at the two cancer centers in Patna and Vellore in the summer of 2008. The equipment also included an infrared non-contact digital thermometer, which would make it possible to monitor patient temperature in the treatment area during the hyperthermia treat. The upper limit of temperature is 108 °F. 7.3 Schedule of the Clinical Trials The first clinical trial involving hyperthermia was started on December 25, 2009, at Patna. Fourteen patients were selected to undergo palliative treatment using a combination of radiation and hyperthermia. The protocol was as follows: the patient will initially undergo 30 min. of hyperthermia in the treatment area and then be immediately taken to the radiation room. Out of the 14 patients, 12 underwent radiation and hyperthermia, while the remaining two patients underwent radiation and chemotherapy. 51 The trials are continuing now, and results will be evaluated after a few months of hyperthermia treatment (along with the conventional radiation and chemotherapy). The second clinical trial is scheduled to start in July, 2010, at Vellore. 52 Chapter 8 CONCLUSIONS This project report has detailed the different stages of the recently initiated phase I clinical trial of a new modality of cancer treatment in India. Specifically, it has focused on the planning, technical details, and implementation of the medical trial involving the use of hyperthermia or heat treatment in cancer treatment, primarily as an added tool to boost the therapeutic effects of conventional treatment methods. The clinical trial involves the addition of hyperthermia or heat treatment to existing treatment techniques, such as radiation or chemotherapy, with the aim to improving patient response. Different methods of hyperthermia and the effects of hyperthermia, along with health factors that increase the risk of hyperthermia, are studied in detail. Additionally, the contribution of the CSUS research group to improved antenna hardware design, treatment planning software for hyperthermia (which was developed at CSUS), equipment development are discussed. Different treatment protocols, such as radiation and hyperthermia and chemotherapy and hyperthermia, and the procedures followed are discussed in detail. The background research on hyperthermia led to the planning of two new clinical trials in India. The first trial involved a total of 14 patients in a palliative mode of treatment with a combination of hyperthermia and radiation while two other patients were treated with 53 hyperthermia and chemotherapy. The trials are continuing now at the Mahavir Cancer Santhan in Patna, Northern India, and the results will be evaluated after a few months of hyperthermia treatment. The second clinical trial is scheduled to start in July, 2010, at the Christian Medical College Hospital in Vellore, a city in Southern India. Thus, this report covered all aspects of the planning, organization, and carrying out of the clinical trials at different centers. This report was the culminating part of the research to obtain insight on hyperthermia treatment protocol. Future work will focus on obtaining the treatment data from the two clinical trial centers and studying the beneficial effect of the hyperthermia modality. This effort will help in understanding the effectiveness of hyperthermia in the fight against the scourge of cancer. 54 REFERENCES 1. Abdul Muqeet Syed and Atif Ahmed Syed, “Thermometric Calibration of the heating effects by 27.12 MHz Mettler Diathermy system for use in Hyperthermia system for treatment of cancer,” M.S. project, Dept. Electrical and Electronic Engineering, California State University, Sacramento, CA, Fall 2009. 2. “Hyperthermia in cancer treatment,” Internet: http://www.cancer.gov/cancertopics/factsheet/Therapy/hyperthermia, Aug., 12, 2004 [Feb., 2010] 3. “Hyperthermia zentrum,” Internet: http://www.hyperthermiezentrum.com/index.php/en/hyperthermia/what-is- hyperthermia, Mar., 2010 [Mar., 2010]. 4. Preetham, K. B., “Microwave hyperthermia therapy in cancer treatment – CSUS efforts from research to clinical trial,” unpublished, May, 2010. 5. Karnik, N. S., Tulpule, R., Kumar, B. P., et al., “Design, simulation and experimental study of near-field beam forming techniques using conformal waveguide arrays,” 55 Internet: http://scitation.aip.org/getabs/servlet/GetabsServlet?prog=normal&id=IMAPCH0000040 00002000162000001&idtype=cvips&gifs=yes&ref=no” Feb., 2010 [ Feb., 2010]. 6. “Hyperthermia in cancer treatment,” Internet: http://www.cancer.gov/cancertopics/factsheet/Therapy/hyperthermia, Aug., 12, 2004 [Feb., 2010]. 7. “Cancer treatment centers of America,” Internet: http://www.cancercenter.com/conventional-cancer-treatment/local- hyperthermia.cfm, Jun. 15, 2009 [Feb., 2010]. 8. Kate Kelland “Regional hyperthermia helps in cancer treatment,” Internet: http://www.oncolink.upenn.edu/resources/article.cfm?c=3&s=8&ss=23&Year=2009&M onth=09&id=16465, Sep. 22, 2009 [Feb., 2010]. 9. Annie “Loco-regional hyperthermia,” Internet: http://www.annieappleseedproject.org/lochyp.html, [Mar., 2010]. 10. Kowal, C. D., Bertino, J. R., “Possible benefits of hyperthermia to chemotherapy,” Internet: http://cancerres.aacrjournals.org/cgi/reprint/39/6_Part_2/2285.pdf, Jun., 1979 [Mar., 2010]. 56 11. “USA Today,” Internet: http://www.healthscout.com/ency/68/271/main.html, Apr. 1, 2009 [Mar., 2010]. 12. 3. Preetham, K. B., “Instructions for radiothermy equipment,” unpublished, Jul., 2008. Emami, B., Scott, C., Perez, C. A., Asbell, S., Grigsby, P., Montesano, A., et al., “Phase III study of interstitial thermo radiotherapy compared with interstitial radiotherapy alone in the treatment of recurrent or persistent human tumors: A prospectively controlled randomized study by the radiation therapy oncology group,” International Journal of Radiation Oncology, Biology and Physics, Vol. 34, pp. 10971104, 1996. 14. Perez, C. A., Pajak, T., Emami, B., Hornback, N. B., Tupchong, L., and Rubin, P., “Randomized phase III study comparing irradiation and hyperthermia with irradiation alone in superficial measurable tumors,” American Journal of Clinical Oncology, Vol. 14, pp. 133-141, 1991. 15. Datta, N. R., Bose, A. K., Kapoor, H. K., and Gupta S., “Head and neck cancers: results of thermoradiotherapy versus radiotherapy,” International Journal of Hyperthermia, Vol. 6, pp. 479-486, 1990. 16. Valdagni, R., Amichetti, M., and Pani, G., “Radical radiation alone versus radical radiation plus microwave hyperthermia for N3 (TNM-UICC) neck nodes: a prospective 57 randomized clinical trial,” International Journal of Radiation Oncology, Biology and Physics, Vol. 15, pp. 13-24, 1998. 17. Overgaard, J., Gonzalez Gonzales, D., Hulshof, M. C. C.M., Arcangeli, G., Dahl, O., and Bentzen, S. M., “Randomized trial of hyperthermia as adjuvant to radiotherapy for recurrent or metastatic malignant melanoma,” The Lancet, Vol. 345, pp. 540-543, 1995. 18. Vernon, C. C., Hand, J. W., Field, S. B., Machin, D., Whaley, J. B., Van Der Zee, J., Van Putten, W. L. J., Van Rhoon, G. C., Van Dijk, J. D. P., Gonzalez Gonzalez, D., Liu, F.-F., Goodman, P., and Sherar, M., “Radiotherapy with or without hyperthermia in the treatment of superficial localized Breast cancer: results from five randomized controlled trials,” International Journal of Radiation Oncology, Biology and Physics, Vol. 35, pp. 731-744, 1996. 19. Van Der Zee, J., Gonzalez Gonzalez, D., Van Rhoon, G. C., Van Dijk, J. D., Van Putten, W. L., and Hart, A. A., “Comparison of radiotherapy alone with radiotherapy plus hyperthermia in locally advanced pelvic tumors: a prospective, randomized, multicentre trial. Dutch Deep Hyperthermia Group,” The Lancet, Vol. 355, pp. 1119-1125, 2000. 20. Jones, E. L., Oleson, J. R., Prosnitz, L. R., Samulski, T. V., Vujaskovic, Z., Yu D., Sanders, L. L., Dewhirst, M. W., “Randomized trial of hyperthermia and radiation for superficial tumors,” J Clin. Oncol, Vol. 23(13), pp. 3079-85, May 1 2005. 58 21. Green, I. Hyperthermia in Conjunction with Cancer Chemotherapy. Health Technology Assessment, No. 2. 1991. Rockville, MD; U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research. Accessed May 12, 2004. Available at URL address: http://www.hstat.nlm.nih.gov/hq/Hquest/db/124/screen/DocTitle/odas/1/s/38698. 22. Hegewisch-Becker, S., Gruber, Y., Corovic, A., Pichlmeier, U., Atanackovic, D., Nierhaus, A., Hossfeld, D., “Whole-body hyperthermia (41.8°C) combined with bimonthly oxaliplatin, high-dose leucovorin and 5-fluorouracil 48-hour continuous infusion in pretreated metastatic colorectal cancer: a phase II study,” Ann Oncol, Vol. 13(8), pp. 1197-1204, 2002 . 23. Hildebrandt, B., Wust, P., Ahlers, O., Dieing, A., Sreenivasa, G., Kerner, T., et al., “The cellular and molecular basis of hyperthermia,” Crit Rev Oncol Hematol, Vol. 43(1), pp. 33-56, 2002. 24. Katschinski, D. M., Wiedemann, G. J., Longo, W., d’Oleire, F. R., Spriggs, D., Robins, H. I., “Whole body hyperthermia cytokine induction: a review, and unifying hypothesis for myeloprotection in the setting of cytotoxic therapy,” Cytokine Growth Factor Rev, Vol. 10(2), pp. 93-97, 1999. 25. Kerner, T., Deja, M., Ahlers, O., Hildebrandt, B., Dieing, A., Riess, H., et al., “Monitoring arterial blood pressure during whole body hyperthermia,” Acta Anaesthesiol Scand, Vol. 46(5), pp. 561-566, 2002. 59