FINAL CHARACTERIZATION OF 3-DIMENSIONAL MICROWAVE HYPERTHERMIA PLANNING SYSTEM Sateesh Nallamilli
advertisement

FINAL CHARACTERIZATION OF 3-DIMENSIONAL MICROWAVE
HYPERTHERMIA PLANNING SYSTEM
Sateesh Nallamilli
B.Tech, JNT University, Hyderabad, 2006
Shaik Mehtab
B.E, Osmania University, Hyderabad, 2007
PROJECT
Submitted in partial satisfaction of
the requirements for the degree of
MASTER OF SCIENCE
in
ELECTRICAL AND ELECTRONIC ENGINEERING
at
CALIFORNIA STATE UNIVERSITY, SACRAMENTO
SUMMER
2010
FINAL CHARACTERIZATION OF 3-DIMENTIONAL MICROWAVE
HYPERTHERMIA PLANNING SYSTEM
A Project
by
Sateesh Nallamilli
Shaik Mehtab
Approved by:
________________________________, Committee Chair
SureshVadhva, Ph.D.
________________________________, Second Reader
Russell Tatro, M.S.
_________________________
Date
ii
Students:
Sateesh Nallamilli
Shaik Mehtab
I certify that these students have met the requirements for format contained in the
University format manual, and that this project is suitable for shelving in the Library and
credit is to be awarded for the project.
______________________, Department Chair
Suresh Vadhva, Ph.D.
Department of Electrical and Electronic Engineering
iii
________________
Date
Abstract
of
FINAL CHARACTERIZATION OF 3-DIMENSIONAL MICROWAVE
HYPERTHERMIA PLANNING SYSTEM
by
Sateesh Nallamilli
Shaik Mehtab
This project will focus on the final tuning and debugging of 3-dimensional
electromagnetic software that was initially developed in the Microwave laboratory at
CSUS. The application of the software in clinical hyperthermia, which involves the
treatment of tumors in the human or animal body by focused microwave radiation. The
software prepares the treatment planning for each individual patient by taking the patient
data, in this case, the CT scan data. This data in turn is used to plan the precise focusing
of the microwave beam. The software has been essentially developed however, there are
some key features still lacking such as the facility to access a multi-patient database, and
transfer of multi-file CT scan files to the main MATLAB program. This project has
focused on making the multi-patient database functional, and testing of the software to
validate its practicality. Final testing was performed on the software, and it is in a ready
shape for use in hospital therapy systems.
, Committee Chair
Suresh Vadhva, Ph.D.
iv
ACKNOWLEDGMENT
Firstly, we would like to express our sincere thanks and gratitude to the respected major
advisor of this project and distinguished faculty member of the Electrical and electronic
engineering department, Dr. Preetham Kumar for making this project available. His
continuous support was the main thing which helped us develop immense interest on the
project. Dr. Preetham Kumar helped us by providing many sources of information which
we needed from beginning of the project till the end. He was always there to meet, talk
and answer the questions which we came across during the project.
We also express our sincere thanks and gratitude to our second reader Dr. Russ Tatro for
being a reader of this project. We greatly appreciate his willingness to be a co-advisor
and committee member for this project. Dr. Russ Tatro spared his valuable office hours
every week to discuss our progress with the project work and report.
Finally, we also thank all our friends and Electrical engineering department who helped
us to complete our project work successfully. Without any of the above mentioned people
the project would not have come out the way it did. Thank you all.
v
TABLE OF CONTENTS
Page
Acknowledgments……………………………………………………………………….v
List of Figures…………………………………………………………………………...viii
Chapter
1. INTRODUCTION …………………………………….……………………….…… 1
2. HYPERTHERMIA PLANNING SYSTEM……………………………………...…. 4
2.1 Input Section…………………………………………………………............ 5
2.2 Specific Absorption Rate Model (SAR)....…….…………..…………….…. .5
2.3 Temperature and its Distribution ………………………………………..…...6
2.4 Treatment Planning ………..……………………………..…………………..7
2.5 Multi-patient database access …………………………………….……….....8
2.6 Evaluation tools………………………………………………….……….......8
3. Graphical User Interface (GUI) design for multi-patient database access………..…10
3.1 Introduction to GUI in MATLAB……………………………………..…..…10
3.2 GUI Elements……………………………………………………….…….…10
4. Simulation Results of Hyperthermia Planning System...............................................18
4.1 Simulation Data Set…………………………………………………..……...19
4.2 Simulation errors in initial project implementation and corrective steps …...19
4.3 Successive treatment planning of multiple patient data………………..……20
4.3.1 Treatment Planning based on Patient1 data set……………………..……..21
4.3.2 Treatment Planning based on Patient2 data set……………………..……..24
vi
4.3.3 Treatment Planning based on Patient3 data set………………………….......27
4.4
Code Implementation…………………………………………………...…...29
5. CONCLUSION …………………………………………………………………......32
Appendix A……………………………………………………………………………...33
Bibliography…………………………………………………………...………………..62
vii
LIST OF FIGURES
Page
Figure 2.1 Basic Hyperthermia Treatment Planning System [1]………………...….….4
Figure 2.2 DICOM File Set and File Format [10]……………………………..……….9
Figure 3.1 Property Inspector…………………………………...……………………..13
Figure 3.2 List box displaying patient names …………………………...…………….15
Figure 4.1 Source patients Model Geometry……...…………………………………...18
Figure 4.2 Temperature Distribution of Patient1 CT scan Data...…………………......21
Figure 4.3 Electric Field Distribution of Patient1 CT scan Data…...…………….........22
Figure 4.4 Zoomed view of Electric field after clicking on Image.…………………....23
Figure 4.5 Temperature Distribution of Patient2 CT scan Data...……………………..24
Figure 4.6 Electric Field Distribution of Patient2 CT scan Data…...……………….....25
Figure 4.7 Zoomed view of Electric field after clicking on Image……...……………..26
Figure 4.8 Temperature Distribution of Patient3 CT scan Data…...…………………..27
Figure 4.9 Electric Field Distribution of Patient3 CT scan Data………………………28
Figure 4.10 Zoomed view of Electric field after clicking on Image……...…………....29
viii
1
Chapter 1
INTRODUCTION
Hyperthermia is a type of treatment in which body tissue is exposed to high temperatures
from 104ºF to 111ºF, to damage and kill cancer cells. The rationale behind hyperthermia
treatment is that primary malignant tumors have a bad blood circulation, which makes
them more sensitive to changes in temperature [1, 2]. Though earlier clinical studies
involved the use of hyperthermia, this negative aspect was one of the reasons behind the
slow progress in hyperthermia research and application.
Eventually, researchers discovered that hyperthermia is more effective as an
adjuvant or added treatment to conventional forms of cancer therapy such as radiation or
chemotherapy [2, 3]. Hence, currently hyperthermia is administered prior to radiation or
chemotherapy, and several clinical studies have shown that the combined modality of
radiation plus hyperthermia or chemotherapy plus hyperthermia significantly improves
the response rate in patients, as compared to just radiation or chemotherapy alone [4, 5].
The hardware design of microwave applicators for thermo-therapeutic
applications is essential in hyperthermia, for the actual application of the RF or
microwave energy on the tumor surface.
However, in order to precisely tune the
applicator power and orientation, accurate simulation tools are required to prepare the
treatment individually for each patient. However, the question now arises that how to
simulate the thermal effect of the device on applied tissue? What is the shape and size of
the effective aperture area? A variety of electromagnetic simulators of electromagnetic
2
fields have been developed, utilizing methods such as Finite Difference Time Domain
and Finite element methods. These simulators provide advanced visualization of the
computed results.
The Microwave Communication Laboratory in our department has been working
on a 3-dimensional hyperthermia planning software, which utilizes the CT scan data of
each individual patient to plan the treatment profile. This planning software uses
MATLAB with the image processing toolbox to display output images showing the
radiated power and temperature distribution over the patient treatment area.
Additionally, the software also has a dynamic capability to allow adjustment of the
applicator position by the system operator, and view the changes in electric field and
temperature profile.
The unique feature of the complete software package is that it is patient specific. This is
achieved by using the CT scan data of the each individual patient to model the electrical
propagation of the various, biological tissues in the human body. Hence this package will
provide a very useful tool for the hyperthermia system operator to plan the treatment
individually for each patient. The operator can effectively use the modeling to adjust the
orientation and pores of the hyperthermia system aperture to focus of the hyperthermia
system applicator to focus the beam onto the tumor surface, while delivering minimal
energy to neighboring healthy tissue.
Specifically, the aim of the current project is to develop and grant operator access
to a multi-patient database, and transfer of multi-file CT scan files to the main MATLAB
3
program. The studies performed for the project are organized in the various chapters of
the report as follows. Chapter 1 is a brief introduction to the work. Chapter 2 gives a
background on the Hyperthermia planning system and a description of the various
components that make up the system. Chapter 3 describes the graphical user interface
implementation software, and multi-patient database access. Chapter 4 lists the
simulation studies performed in the work, and finally, Chapter 5 draws conclusions from
our work.
4
Chapter 2
HYPERTHERMIA PLANNING SYSTEM
The treatment planning for hyperthermia may be resolved into six parts which are
introduced below.
Figure 2.1 Basic Hyperthermia Treatment Planning System [1]
Input section
Specific Absorption Rate Model
Temperature and its Distribution
Treatment Planning
5
Multi-patient database
Evaluation Tools
2.1 Input section
The input section is used to determine the distribution of dielectric parameters like
conductivity and permittivity of both the applicators and the patient. For each patient a 40
cm CT scan is made and segmented into fat, muscle and bone. The tissues are given
dielectric properties in accordance with the SAR distribution on the dielectric parameters.
This part of the algorithm also calculates the grid parameters of the lattice which defines
the outer boundary of the computational lattice. The time index, field array initialization
and the material parameter setup are defined and the boundary conditions are calculated
from the temporal data that is stored by the time index. [3]
2.2 Specific Absorption Rate Model (SAR Model)
Specific Absorption Rate (SAR) and its Distribution is the determination of the rate of
energy absorption per unit mass, wkg-1, in three dimensions under specified conditions in
standard phantoms or in a patient from a given treatment machine. The data accumulated
during this procedure characterize the heating technique under the specific conditions
employed and permit general identification of those sites and target volumes which are
likely to prove amenable to treatment with a particular technique. In addition, the
distribution of Specific Absorption Rate [SAR] forms one group of input parameters
which is essential for the calculation of the temperature distribution in vivo. [4]
6
It is an important factor in hyperthermia planning system because it
controls the amount of power delivered to the tumor area while keeping the power
delivered to the neighboring healthy tissues minimal. Heating from microwave and RF
radiation best relates to Specific Absorption Rate (SAR) rather than the incident power
density. The total SAR is related to the internal E- fields as
SAR= 1/ρ ωε0εrnΕ2loc
Where ρ is the mass density of the object in kg/m3
And SAR is the specific absorption rate in W/kg
2.3 Temperature and its Distribution
It is the determination of the distribution of temperature in three dimensions in a patient
throughout the course of a clinical treatment.
The temperature data accumulated during the clinical treatment form the most
valuable record of that treatment and is the ultimate source of data characterizing the
heating session. In practice, and with currently available invasive thermometry, complete
temperature distributions in vivo cannot be determined. The state of the art technology is
presently limited to recommending minimum procedures which could probably indicate
when an appropriate hyperthermia treatment had been delivered.
The general factors to consider the transfer of heat in tissue are thermo physical
properties of tissue such as heat capacity, thermal conductivity, geometry of irradiated
7
organism, heat absorption due to applicator, heat production due to metabolic processes,
heat flow due to perfusion of blood and thermoregulatory mechanism. By delivering
thermal energy, the tissue is stimulated to increase the blood flow by thermoregulation in
order to remove the excess heat. [4]
2.4 Treatment Planning
Treatment Planning is the selection of the optimal treatment technique and the
geometrical configuration of that technique based on knowledge of the performance of
available treatment machines and on the computation of the expected three dimensional
temperature distributions in a patient.
This definition describes closely the decision making process known as treatment
planning in radiotherapy. The difference in practice between the two is that, in the case of
hyperthermia, the computational aspects are less advanced and are subject to far greater
uncertainty. In the sections that follow each of the three areas defined above is discussed
in some detail. After a brief review of the relevant recent literature on these topics
suggestions are offered as to how the current knowledge may best be applied in the
clinical environment taking into account the wide variation in the equipment available
and its degree of sophistication. From the ensuing discussion, areas requiring further
study can be identified.
8
2.5 Multi-patient database access
In a typical cancer treatment center, there are expected to be a large number of patients,
and it is essential that the system operator should have access to each patient’s CT scan
database, to develop the individual treatment profile for that patient. In this project, the
effort has been to modify the main GUI software to generate a patient identification
window, which requires the patient’s name or identification number. Once the operator
selects a specific patient’s name or identification number, then the patient’s CT scan files,
which are stored in DICOM format, as a set of *.dcm files, are uploaded to the main
software, and the FDTD routine is executed to generate the electric field and temperature
profile over the patient treatment area. If the temperature focus is observed in an area
shifted from the tumor area, then the operator can use the cross-hair GUI function to
adjust the applicator position, and re-check the field/temperature distribution.
This
procedure can be repeated until optimal focus at the tumor is achieved.
2.6 Evaluation Tools
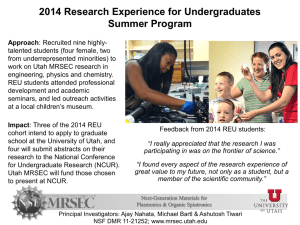
The code reads a section of human body CT scan image stored in DICOM format.
The DICOM standard facilitates the interpretability of medical image imaging equipment
by specifying set of protocols for network communications; syntax and semantics of
commands and associated information which can be exchanged using these protocols a
file format and a medical directory structure to facilitates access to the images and related
9
information stored on interchangeable media. The standard pertains to the field of
Medical Informatics. Within that field, it addresses the exchange of digital information
between medical imaging equipment and the other systems. Such equipment may
interoperate with other medical devices, the scope of this standard needs to overlap with
other areas of Medical Informatics. A DICOM file format provides a mean to encapsulate
in a file the data set representing a SOP instance related to a DICOM IOD. As shown in
the figure, the byte stream of the Data set is placed into the file after the DICOM file
meta information. Each file contains a single SOP instance. [10]
Figure 2.2 DICOM File-set and File Format [10]
10
Chapter 3
GRAPHICAL USER INTERFACE (GUI) DESIGN FOR MULTI-PATIENT
DATABASE ACCESS
3.1 Introduction to GUI in Matlab
A graphical user interface (GUI) is a user interface built with graphical objects, such as
buttons, text fields, sliders, and menus. In general, these objects already have meanings to
most computer users. For example, when we move a slider, a value changes; when we
press an OK button, our settings are applied and the dialog box is dismissed. Of course,
to leverage this built-in familiarity, we must be consistent in how you use the various
GUI-building components [11].
Applications that provide GUIs are generally easier to learn and use. The action that
results from a particular user action can be made clear by the design of the interface. The
sections that follow describe how to create GUIs with MATLAB. This includes laying
out the components, programming them to do specific things in response to user actions,
and saving and launching the GUI; in other words, the mechanics of creating GUIs.
3.2 GUI Elements
Push button
A push button is typically used when you want an immediate action to occur when the
user presses the button. It is used to trigger a callback when clicked with a mouse. An
example might a button to start the application.
11
Check box
Check boxes generate an action when clicked and indicate their state as checked or not
checked. Check boxes are useful when providing the user with a number of independent
choices that set a mode (e.g., display a toolbar or generate callback function
prototypes).The Value property indicates the state of the check box by taking on the
value of the Max or Min property (1 and 0 respectively by default):
•Value = Max, box is checked.
•Value = Min, box is not checked.
You can determine the current state of a check box from within its callback by querying
the state of its Value property, as illustrated in the following example:
function checkbox1_Callback(h,eventdata,handles,varargin)
if (get(h,'Value') == get(h,'Max'))
% then checkbox is checked-take appropriate action
else
% checkbox is not checked-take appropriate action
12
Radio Button
It is a type of toggle button with a small circular dot in the middle when it is on and no
dot when it is off. It is typically used when you need to group several buttons together so
that the groups of buttons have mutually exclusive settings.
For Example
Set (handles.option1,’Value’, 1);
Set (handles.option2,’Value’, 0);
Set (handles.option3,’Value’, 0);
Edit Text
Edit text controls are fields that enable users to enter or modify text strings. Use edit text
when you want text as input. The String property contains the text entered by the user. To
obtain the string typed by the user, get the String property in the callback.
function edittext1_Callback (h, event data, handles, varargin)
user_string = get (h, 'string');
Static Text
Static text controls displays lines of text. Static text is typically used to label other
controls, provide directions to the user, or indicate values associated with a slider. Users
cannot change static text interactively and there is no way to invoke the callback routine
associated with it.
13
Slider function
Sliders accept numeric input within a specific range by enabling the user to move a
sliding bar. Users move the bar by pressing the mouse button and dragging the slide, by
clicking in the trough, or by clicking an arrow. The location of the bar indicates a
numeric value.
We can orient the slider either horizontally or vertically by setting the relative width and
height of the Position property:
•Horizontal slider – width is greater than height.
•Vertical slider – height is greater than width.
For example, these settings create a horizontal slider.
Figure 3.1 Property Inspector
Slider1=uicontrol(gcf,…’style’,’slider’,….’callback’,…
[‘slvalue=get(slider1,’’value’’);’,….’disp (num2str(slvalue));’…]);
14
List box
List boxes display a list of items and enable users to select one or more items. The String
property contains the list of strings displayed in the list box. The first item in the list has
an index of 1. The Value property contains the index into the list of strings that
correspond to the selected item. If the user selects multiple items, then Value is a vector
of indices. By default, the first item in the list is highlighted when the list box is first
displayed. If we do not want any item highlighted then set the Value property to empty.
The List box Top property defines which string in the list displays as the top most items
when the list box is not large enough to display all list entries. List box Top is an index
into the array of strings defined by the String property and must have a value between 1
and the number of strings. Non integer values are fixed to the next lowest integer.
The following is a sample load_listbox function, which is called by the opening function
of the GUI M-file as well as by the list box callback. [7]
function load_listbox(dir_path, handles)
cd (dir_path)
dir_struct = dir(dir_path);
[sorted_names,sorted_index] = sortrows({dir_struct.name}');
handles.file_names = sorted_names;
handles.is_dir = [dir_struct.isdir];
15
handles.sorted_index = [sorted_index];
guidata(handles.figure1,handles)
set(handles.listbox1,'String',handles.file_names,...
'Value',1)
set(handles.text1,'String',pwd)
Figure 3.2: List Box displaying patient names.
16
Frame
It is a decorative rectangular box with in a figure. It is used for the visual grouping of
other controls. It makes the user interface easier to understand by visually grouping
related controls. Frames do not have any callback routine associated with them and only
ui-controls can appear with in them.
Popup Menu
Popup menus open to display a list of choices when users press the arrow. The String
property contains the list of string displayed in the popup menu. The Value property
contains the index into the list of strings that correspond to the selected item. User
Interface Controls. When not open, a popup menu displays the current choice, which is
determined by the index contained in the Value property. The first item in the list has an
index of 1. Popup menus are useful when you want to provide users with a number of
mutually exclusive choices, but do not want to take up the amount of space that a series
of radio buttons requires.[7]
Programming the Popup Menu
You can program the popup menu callback to work by checking only the index of the
item selected (contained in the Value property) or you can obtain the actual string
contained in the selected item. This callback checks the index of the selected item and
uses a switch statement to take action based on the value. If the contents of the popup
menu are fixed, then you can use this approach.
17
function varargout = popupmenu1_Callback(h,eventdata,handles,varargin)
val = get(h,'Value');
switch val
case 1
% The user selected the first item
case 2
% The user selected the second item.
This callback obtains the actual string selected in the popup menu. It uses the value to
index into the list of strings. This approach may be useful if your program dynamically
loads the contents of the popup menu based on user action and you need to obtain the
selected string. Note that it is necessary to convert the value returned by the String
property from a cell array to a string.
function varargout = popupmenu1_Callback(h,eventdata,handles,varargin)
val = get(h,'Value');
string_list = get(h,'String');
selected_string = string_list{val}; % convert from cell array to string %
18
Chapter 4
SIMULATION RESULTS OF HYPERTHERMIA PLANNING SYSTEM
This chapter discusses the several simulations done on the hyperthermia planning system
software. The software package contains three sections: patient model, source model and
FDTD field calculations. The complete geometry is shown in Fig 4.1
FDTD Field calculation over entire simulation space
P(x, y, z)
Z
(X)
r
S(x0, y0, z0)
Patient Model
Source Model
Y
X
Figure 4.1 Source-Patient Model Geometry
The patient model is created from the CT scan data: this is achieved by the first part of
the treatment planning software which converts the CT distribution into an electrical
permittivity/magnetic permeability/electrical conductivity (//) distribution. The
source model is created by assuming a circular area with a specified current distribution,
to replicate the hyperthermia applicator system.
19
4.1 Simulation Data Set
In this simulation work we used four different patient data sets. The spatial resolution
along x-y-z directions for the simulation software is:
∆z=0.002 m
∆y=0.002 m
∆x=0.002 m
However, due to a limitation in maximum memory size that the software can handle, we
have use the interpolation along all 3 axes of the data set. This constraint can be avoided
by using a Student version of Matlab with higher disk storage area.
4.2 Simulation errors in initial project implementation and corrective steps
The simulation of the entire program is carried out at the hyperthermia application
frequency of 27MHz. When the program is initialized it shows the list box with different
patient names.
The software package was being tested on different sets of CT scan data. One aspect of
the work covered under this project is to test the software package to efficiently run and
simulate the data of different patients CT scan. This is the major step in testing, as the
ultimate purpose of the software is to make it applicable to hyperthermia treatment
planning in an actual cancer center which is treating a large number of patients daily.
20
During the first phase of the development of this treatment planning software, the CT
scan section set of just one patient was used to extract the data. Now it is developed to
use for multiple patients: however, there was a problem with list box not closing at the
start of the program and we implemented a function called close to close the list box after
selecting the patient. The major change done in the program is to use multiple CT scan
data along all three axes. After these modifications, successful generation of 3-D images
was achieved. In the modified version, the code increase the period of interpolation and,
instead of talking consecutive image sections, it uses 8, 16 and 32 image sections along
the Z-axis. However, even after these interpolation modifications, the SARs of the
temperature output results were satisfactory.
A further problem that the previous project partners faced was the inability of the
software to access multiple patient data: after the first patient selection, the routine
generated an error signal, if prompted to select the next patient. This problem in the
software was rectified after considerable adjustment of the software code, and proper
sequencing of the initial list box, and successive image displays.
4.3 Successive treatment planning of multiple patient data
The following simulation study was successfully able to access three patient data sets,
and generate the required image files for effective treatment planning.
21
4.3.1 Treatment planning based on Patient 1 data set
The figure 4.2 shows all the interpolation sections of patient1, each section depicting the
temperature in ºC. These show the simulated temperature rise in each section in response
to the 27 MHz diathermy source. This is the first stage of the treatment planning, which
assumes the default setting of the applicator.
Figure 4.2: Temperature Distribution of Patient1 CT scan Data
22
Figure 4.3 shows the electric field distribution over all interpolated sections, and also the
position of diathermy source antenna. This graphical layout is used to position the X-Y
position of the diathermy applicator source near the tumor area. The dynamic adjustment
of the applicator is achieved by means of a cross-hair function, which allows the operator
to focus on the tumor area.
Figure 4.3: Electrical Field Distribution of Patient1 CT scan Data
23
Figure 4.4 shows the electric field of the section selected in figure and is used to focus the
Z-axis of the antenna position to an optimal position near the tumor.
Figure 4.4: Zoomed view of Electric field after clicking on image
The cross hairs shown in the figure are used to fix the position of the antenna. Now the
simulation package takes in the new X-Y-Z co-ordinates of the source antenna and
recalculates the temperature distribution over the entire scan area. This process is
repeated by the system operator until an optimal antenna position is reached.
24
4.3.2 Treatment planning based on Patient 2 data set
The figure 4.5 shows all the interpolation sections of patient2, each section depicting the
temperature in ºC. These show the simulated temperature rise in each section in response
to the diathermia source.
Figure 4.5: Temperature Distribution of Patient2 CT Scan Data
25
Figure 4.6 shows the electric field distribution over all interpolated sections, and also the
position of diathermy source antenna. This graphical layout is used to position the X-Y
position of the antenna source near the tumor area.
Figure 4.6: Electrical Field Distribution of Patient2 CT Scan Data
26
Figure 4.7 shows the electric field of the section selected in figure and is used to focus the
Z-axis of the antenna position to an optimal position near the tumor.
Figure 4.7: Zoomed view of Electric field after clicking on any image
27
4.3.3 Treatment planning based on Patient 3 data set
The figure 4.8 shows all the interpolation sections of patient3, each section depicting the
temperature in ºC. These show the simulated temperature rise in each section in response
to the diathermia source.
Figure 4.8: Temperature Distribution of Pateint 3 CT Scan Data
28
Figure 4.9 shows the electric field distribution over all interpolated sections, and also the
position of diathermy source antenna. This graphical layout is used to position the X-Y
position of the antenna source near the tumor area.
Figure 4.9: Electric Field Distribution of Patient 3 CT Scan Data
29
Figure 4.10 shows the electric field of the section selected in figure and is used to focus
the Z-axis of the antenna position to an optimal position near the tumor.
Figure 4.10: Zoomed View of Electric Field after clicking on any image
4.4 Code Implementation
For the program used for simulating the above results, the following information is
required as input:
30
The name of the patient, in order to extract the corresponding CT file set
The size in the X-dimension of the CT scan data
The value of the time steps in the Y, Z-dimensions of the CT scan data
The program calculates the computational lattice from the following information:
Frequency of operation [in this case 27 MHz is chosen]
Number of cells per wavelength [to define the X-Y-Z resolution]
Total number of time steps
The spatial increment is calculated based on the input provided, which is one-tenth of a
wavelength, in order to obtain good resolution for the fields. The value of the grid used
throughout the program, defines the outer boundaries for the computational lattice.
The next step is to define the time index, initialize the field arrays and setup the material
parameters. The time index holds the temporal data, which is used in computing the
boundary conditions and field updating equations. The temporal data is a circular link list
that rotates with every time index, this is necessary for the field to propagate. Grid
parameters are computed in which scattered properties are defined and the values of the
updating coefficients are computed for the entire lattice. [8]
Lattice boundary conditions are applied in order to minimize the effects of reflections at
the boundary of the solution space. These boundary conditions minimize the reflection of
any outgoing waves by simulating the propagation of the wave from the lattice plane
31
adjacent to the lattice truncation plane in a number of time steps corresponding to the
propagation delay. The averaging process is used to take into account all possible local
angels of the incidence of the outgoing wave at the lattice boundary and possible multiple
incidences. [8]
The software program calculates the 3-dimentional electric field distribution throughout
the simulation pace, which includes the patient treatment area. The electric filed
components Ex, Ey, Ez are calculated in the 3-dimentional spaces. The Specific
Absorption Rate (SAR) is determined. The SAR measures the amount of energy
absorption in the time and is defined by:
SAR (x,y,z)=[|E(x,y,z)|² X σ(x,y,z)]/[2ρ(x,y,z)]
Where, |E(x,y,z)|²=|Ex(x,y,z)|²+ |Ey(x,y,z)|²+ |Ez(x,y,z)|²
σ(x,y,z)= Electrical conductivity at part (x,y,z)
ρ(x,y,z)= Volume density at part (x,y,z)
The unit of SAR is W/kg. Once the SAR is calculated, the 3-dimentional-temperature
distribution is calculated using the bio-heat transfer equation. And the Matlab program
used to generate the simulations results is included in the Appendix A.
32
Chapter 5
CONCLUSION
The main goal of this project is a facility to access a multi-patient database, and transfer of
multi-file CT scan files to the main hyperthermia treatment planning MATLAB program. A few
modifications in the program, including the list box implementation, made it possible to use the
program effectively with a multiple patient’s database. The GUI was developed in MATLAB
programming language and the access to various patient files from the database was presented.
This software was successfully tested for executing various patient CT scan files in the graphical
window.
The main advantage of this software is that, it is patient-specific and hence more accurate than a
process which uses a generic patient model. The actual CT scan files for the patient are obtained
in a MATLAB data file. This helps in treatment planning of incident antenna power, antenna
position and configuration, to focus the beam at the desired tumor location, and cause minimum
damage to the healthy tissues around the tumor spot. The better visualization from the 3
dimensional images helps the doctors for precisely applying hyperthermia techniques to patient
tumors.
The software was designed to be ultimately used in an actual cancer center, which
provides hyperthermia treatment as an additional cancer-fighting tool. Hence the remaining task
is to carry out an experimental trial of the software in a typical cancer center, treating hundreds of
patients. The trial will bring out the efficiency and reliability of the software, and provide
valuable feedback to correct any shortcomings in the operational efficiency.
33
APPENDIX A
Matlab code
function varargout = original(varargin)
gui_Singleton = 1;
gui_State = struct('gui_Name',
mfilename, ...
'gui_Singleton', gui_Singleton, ...
'gui_OpeningFcn', @original_OpeningFcn, ...
'gui_OutputFcn', @original_OutputFcn, ...
'gui_LayoutFcn', [], ...
'gui_Callback',
[]);
if nargin & isstr(varargin{1})
gui_State.gui_Callback = str2func(varargin{1});
end
if nargout
varargout{1:nargout} = gui_mainfcn(gui_State, varargin{:});
else
gui_mainfcn(gui_State, varargin{:});
end
function original_OpeningFcn(hObject, eventdata, handles, varargin)
handles.output = hObject;
guidata(hObject, handles);
if nargin == 3,
initial_dir = pwd;
elseif nargin > 4
if strcmpi(varargin{1},'dir')
if exist(varargin{2},'dir')
initial_dir = varargin{2};
else
errordlg('Input argument must be a valid directory','Input Argument Error!')
return
end
else
errordlg('Unrecognized input argument','Input Argument Error!');
return;
34
end
end
% Populate the listbox
load_listbox(initial_dir,handles)
function varargout = original_OutputFcn(hObject, eventdata, handles)
% Get default command line output from handles structure
varargout{1} = handles.output;
function varargout = listbox1_Callback(h, eventdata, handles)
get(handles.figure1,'SelectionType');
if strcmp(get(handles.figure1,'SelectionType'),'open')
index_selected = get(handles.listbox1,'Value');
file_list = get(handles.listbox1,'String');
patientname = file_list{index_selected};
if handles.is_dir(handles.sorted_index(index_selected))
cd (patientname)
else
[path,name,ext,ver] = fileparts(patientname);
switch ext
case '.fig'
guide (patientname)
otherwise
try
open(patientname)
catch
errordlg(lasterr,'File Type Error','modal')
end
end
end
close
fprintf(1,'Patient selected:%s\n',patientname);
p=1;
file1=[num2str(patientname),'_000',num2str(p),'.dcm'];
[X,map]=dicomread(char(file1));
35
[ix,iy]=size(X);
iz = 20;
ctnumber=zeros(ix,iy,iz);
intp=4;
xmax=0.2;
ymax=0.2;
zmax=0.2;
dx=xmax/ix;
dy=ymax/iy;
dz=zmax/iz;
for p=1:iz
file=[num2str(patientname),'_000',num2str(p),'.dcm'];
if p > 9 file=[num2str(patientname),'_00',num2str(p),'.dcm'];
end;
[X,map]=dicomread(char(file));
ctnumber(:,:,p)=X;
end;
ctmax=max(max(max(ctnumber)));
ctnumber=ctnumber*2000/ctmax-1000;
ct11=ctnumber;
%image(ct11);
i1=1;
for i=1:intp:ix;
j1=1;
for j=1:intp:iy;
for k=1:iz;
x1(i1,j1,k)=(i-1)*dx;
y1(i1,j1,k)=(j-1)*dy;
z1(i1,j1,k)=(k-1)*dz;
ct13(i1,j1,k)=ct11(i,j,k);
end;
j1=j1+1;
end;
i1=i1+1;
end;
[ix,iy,iz]=size(ct13);
dx=dx*intp;
36
dy=dy*intp;
dz=dz;
ix1=ix*1.5/4;
xii=ix1*dx;
ix2=0.1*ix;
dx2=ix2*dx;
iy1=iy*1.5/4;
yii=iy1*dy;
iy2=iy/2+0.1*iy;
iz1=iz/2;
zii=iz1*dz;
iz2=iz/2+0.1*iz;
for i=1:ix;
xx=i*dx;
for j=1:iy;
yy=j*dy;
for k=1:iz;
zz=k*dz;
if (xx-xii)^2 + (yy-yii)^2 + (zz-zii)^2 <= dx2^2
ct13(i,j,k)=300;
end;
end;
end;
end;
inx=ix*iy*iz;
ct1x(1:inx)=ct13;
x(1:inx)=x1(:,:,:);
y(1:inx)=y1(:,:,:);
z(1:inx)=z1(:,:,:);
G=ones(ix,iy,iz)*0.001;
Roe=1.29*ones(ix,iy,iz);
37
Er=ones(ix,iy,iz);
sph=ones(ix,iy,iz)*1006;
perf=ones(ix,iy,iz)*0;
met=ones(ix,iy,iz)*0;
therm=ones(ix,iy,iz)*0.026;
%electrical/density parameters for different human tissues at 2.45GHz
%layer air
G1=0.001;
Er1=1;
Roe1=1.29;
sph1=1006;
perf1=0;
met1=0;
therm1=0.026;
%layer blood
G2=2.5448;
Er2=58.264;
Roe2=1000;
sph2=3600;
perf2=1000;
met2=0;
therm2=0.51;
%layer bone
G3=0.32;
Er3=16.1;
Roe3=1080;
sph3=2238;
perf3=3;
met3=0;
therm3=0.36;
%layer brain
G4=1.08;
Er4=42.8;
38
Roe4=1040;
sph4=3640;
perf4=56;
met4=331;
therm4=0.534;
%brain(grey matter)
G5=1.8077;
Er5=48.911;
Roe5=1000;
sph5=3680;
perf5=67.1;
met5=5370;
therm5=0.565;
%brain(white matter)
G6=1.215;
Er6=36.167;
Roe6=1000;
sph6=3600;
perf6=23.7;
met6=5370;
therm6=0.503;
%cartilage
G7=1.7559;
Er7=38.77;
Roe7=1000;
%cerebro-spinal fluid
G8=3.4578;
Er8=66.243;
Roe8=1000;
sph8=4200;
perf8=0;
met8=0;
therm8=0.6;
%layer fat
39
G9=0.1045;
Er9=5.28;
Roe9=920;
sph9=2300;
perf9=2.8;
met9=302;
therm9=0.23;
%layer heart
G10=2.2561;
Er10=54.814;
Roe10=1000;
%layer kidney
G11=2.4295;
Er11=52.742;
Roe11=1000;
%layer lens
G12=1.504;
Er12=44.625;
Roe12=1000;
%layer liver
G13=1.6864;
Er13=43.035;
Roe13=1000;
%inflated lung
G14=0.8084;
Er14=20.5909;
Roe14=1000;
%inflated lymph
G15=1.9679;
Er15=57.201;
Roe15=1000;
%layer muscle
40
G16=1.7388;
Er16=52.729;
Roe16=1040;
sph16=3500;
perf16=5;
met16=756;
therm16=0.498;
%layer ovary
G17=2.2641;
Er17=44.7;
Roe17=1000;
%layer pancreas
G18=1.9679;
Er18=57.201;
Roe18=1000;
%layer skin
G19=0.86;
Er19=39.1;
Roe19=1010;
sph19=3150;
perf19=12;
met19=1125;
therm19=0.343;
%layer spleen
G20=2.238;
Er20=52.449;
Roe20=1000;
%layer testis
G21=2.1676;
Er21=57.551;
Roe21=1000;
%layer thyroid
G22=1.9679;
41
Er22=57.201;
Roe22=1000;
%layer eyeball
G23=2.21;
Er23=73.9;
Roe23=1010;
sph23=4200;
perf23=0;
met23=0;
therm23=0.586;
%breast fat
G24=0.1378;
Er24=5.1750;
Roe24=1000;
sph24=2300;
perf24=2.8;
met24=302;
therm24=0.23;
%layer cerebellum
G25=2.1125;
Er25=45.0552;
Roe25=1000;
sph25=3640;
perf25=56;
met25=331;
therm25=0.534;
%cornea
G26=2.3075;
Er26=51.9018;
Roe26=1000;
sph26=3000;
perf26=3.8;
met26=0;
therm26=0.4;
%dura
42
G27=1.6776;
Er27=42.2677;
Roe27=1000;
%layer tongue
G28=1.8121;
Er28=52.9196;
Roe28=1000;
Gtumor=1.5;
Ertumor=40;
Roetumor=1000;
for i=1:ix;
for j=1:iy;
for k=1:iz;
%this portion of the code detects the tissue from the image acquired for the
corresponding ct number
%layer air boundary
if ctnumber(i,j,k) >= -1050 & ctnumber(i,j,k) <= -950
G(i,j,k)=G1;
Er(i,j,k)=Er1;
Roe(i,j,k)=Roe1;
sph(i,j,k)=sph1;
perf(i,j,k)=perf1;
met(i,j,k)=met1;
therm(i,j,k)=therm1;
%layer blood boundary
elseif ctnumber(i,j,k) >= 23 & ctnumber(i,j,k) <= 27
G(i,j,k)=G2;
Er(i,j,k)=Er2;
Roe(i,j,k)=Roe2;
sph(i,j,k)=sph2;
perf(i,j,k)=perf2;
met(i,j,k)=met2;
therm(i,j,k)=therm2;
43
%layer bone boundary
elseif ctnumber(i,j,k) >= 900 & ctnumber(i,j,k) <= 1100
G(i,j,k)=G3;
Er(i,j,k)=Er3;
Roe(i,j,k)=Roe3;
sph(i,j,k)=sph3;
perf(i,j,k)=perf3;
met(i,j,k)=met3;
therm(i,j,k)=therm3;
%layer brain boundary
elseif ctnumber(i,j,k) >= 33 & ctnumber(i,j,k) <= 41
G(i,j,k)=G4;
Er(i,j,k)=Er4;
Roe(i,j,k)=Roe4;
sph(i,j,k)=sph4;
perf(i,j,k)=perf4;
met(i,j,k)=met4;
therm(i,j,k)=therm4;
%layer brain_grey matter boundary
elseif ctnumber(i,j,k) >= 32 & ctnumber(i,j,k) <= 44
G(i,j,k)=G5;
Er(i,j,k)=Er5;
Roe(i,j,k)=Roe5;
sph(i,j,k)=sph5;
perf(i,j,k)=perf5;
met(i,j,k)=met5;
therm(i,j,k)=therm5;
%layer brain_white matter boundary
elseif ctnumber(i,j,k) >= 24 & ctnumber(i,j,k) <= 36
G(i,j,k)=G6;
Er(i,j,k)=Er6;
Roe(i,j,k)=Roe6;
44
sph(i,j,k)=sph6;
perf(i,j,k)=perf6;
met(i,j,k)=met6;
therm(i,j,k)=therm6;
%layer cartilage boundary
elseif ctnumber(i,j,k) >= 93 & ctnumber(i,j,k) <= 103
G(i,j,k)=G7;
Er(i,j,k)=Er7;
Roe(i,j,k)=Roe7;
%layer csf boundary
elseif ctnumber(i,j,k) >= 0 & ctnumber(i,j,k) <= 22
G(i,j,k)=G8;
Er(i,j,k)=Er8;
Roe(i,j,k)=Roe8;
sph(i,j,k)=sph8;
perf(i,j,k)=perf8;
met(i,j,k)=met8;
%layer Fat boundry
elseif ctnumber(i,j,k) >= -55 & ctnumber(i,j,k) <= -45
G(i,j,k)=G9;
Er(i,j,k)=Er9;
Roe(i,j,k)=Roe9;
sph(i,j,k)=sph9;
perf(i,j,k)=perf9;
met(i,j,k)=met9;
therm(i,j,k)=therm9;
%layer heartboundry
elseif ctnumber(i,j,k) >= 52 & ctnumber(i,j,k) <= 58
G(i,j,k)=G10;
Er(i,j,k)=Er10;
Roe(i,j,k)=Roe10;
%layer kidney boundary
elseif ctnumber(i,j,k) >= 40 & ctnumber(i,j,k) <= 46
G(i,j,k)=G11;
45
Er(i,j,k)=Er11;
Roe(i,j,k)=Roe11;
%layer lens boundry
elseif ctnumber(i,j,k) >= 47 & ctnumber(i,j,k) <= 53
G(i,j,k)=G12;
Er(i,j,k)=Er12;
Roe(i,j,k)=Roe12;
%layer liver boundray
elseif ctnumber(i,j,k) >= 50 & ctnumber(i,j,k) <= 56
G(i,j,k)=G13;
Er(i,j,k)=Er13;
Roe(i,j,k)=Roe13;
%layer lung boundary
elseif ctnumber(i,j,k) >= -815 & ctnumber(i,j,k) <= 667
G(i,j,k)=G14;
Er(i,j,k)=Er14;
Roe(i,j,k)=Roe14;
%layer lymph boundary
elseif ctnumber(i,j,k) >= 26 & ctnumber(i,j,k) <= 330
G(i,j,k)=G15;
Er(i,j,k)=Er15;
Roe(i,j,k)=Roe15;
%layer Muscle boundary
elseif ctnumber(i,j,k) >= 38 & ctnumber(i,j,k) <= 46
G(i,j,k)=G16 ;
Er(i,j,k)=Er16;
Roe(i,j,k)=Roe16;
sph(i,j,k)=sph16;
perf(i,j,k)=perf16;
met(i,j,k)=met16;
therm(i,j,k)=therm16;
%layer ovary boundary
elseif ctnumber(i,j,k) >= 42& ctnumber(i,j,k) <= 48
46
G(i,j,k)=G17 ;
Er(i,j,k)=Er17;
Roe(i,j,k)=Roe17;
%layer pancreas boundary
elseif ctnumber(i,j,k) >= 29& ctnumber(i,j,k) <= 35
G(i,j,k)=G18;
Er(i,j,k)=Er18;
Roe(i,j,k)=Roe18;
%layer Skin boundary
elseif ctnumber(i,j,k) >= 70 & ctnumber(i,j,k) <= 85
G(i,j,k)=G19;
Er(i,j,k)=Er19;
Roe(i,j,k)=Roe19;
sph(i,j,k)=sph19;
perf(i,j,k)=perf19;
met(i,j,k)=met19;
therm(i,j,k)=therm19;
%layer spleen boundary
elseif ctnumber(i,j,k) >= 51& ctnumber(i,j,k) <= 57
G(i,j,k)=G20 ;
Er(i,j,k)=Er20;
Roe(i,j,k)=Roe20;
%layer testis boundary
elseif ctnumber(i,j,k) >= 30& ctnumber(i,j,k) <= 34
G(i,j,k)=G21;
Er(i,j,k)=Er21;
Roe(i,j,k)=Roe21;
%layer thyroid boundary
elseif ctnumber(i,j,k) >= 38 & ctnumber(i,j,k) <= 42
G(i,j,k)=G22;
Er(i,j,k)=Er22;
Roe(i,j,k)=Roe22;
47
%layer eyeball
elseif ctnumber(i,j,k) >=47 & ctnumber(i,j,k) <= 53
G(i,j,k)=G23;
Er(i,j,k)=Er23;
Roe(i,j,k)=Roe23;
sph(i,j,k)=sph23;
perf(i,j,k)=perf23;
met(i,j,k)=met23;
end;
end;
end;
end;
GG=G;
EEr=Er;
RRoe=Roe;
ssph=sph;
pperf=perf;
mmet=met;
ttherm=therm;
freq1=27e6;
;
cells_per_wavelength=5;
%**********************************************************************
*
% Fundamental constants
%**********************************************************************
*
cc = 2.99792458e8;
muz = 4.0*pi*1.0e-7;
%speed of light in free space
%permeability of free space
48
epsz = 1.0/(cc*cc*muz);
%permittivity of free space
aimp1 = 1;
aimp2 = 1; % sqrt (muz/epsz);
%**********************************************************************
*
% Initial calculations
%**********************************************************************
*
lambda = cc/freq1;
D=dx;
dt = dx/(2.0*cc); %dx = 0.002 time step
%
xp=0.01;
yp=0.01;
zp=0.01;
antx=xp;
anty=yp;
antz=zp;
ant_objx=0.1;
ant_objy=0.1;
ant_objz=0.1;
obj_sizex = xmax;
obj_sizey = ymax;
obj_sizez = zmax;
objpx=antx+ant_objx;
objpy=anty+ant_objy;
objpz=antz+ant_objz;
for norient=1:10;
antx=xp;
anty=yp;
antz=zp;
49
ant_objx=objpx-antx;
ant_objy=objpy-anty;
ant_objz=objpz-antz;
Dmaxx = obj_sizex + ant_objx + antx ;
Dmaxy = obj_sizey + ant_objy + anty ;
Dmaxz = obj_sizez + ant_objz + antz ;
Dmax = max (Dmaxx, Dmaxy)
Dmax= max (Dmax, Dmaxz);
%**********************************************************************
*
% Inputs
%**********************************************************************
xinput = Dmaxx*1.1; %input('Enter the x dimensions of the space lattice: ');
yinput = Dmaxy*1.1;
zinput = Dmaxz*1.1;
%**********************************************************************
*
% Grid parameters
%**********************************************************************
*
tcon = 3;
ie = round(xinput/dx);
%number of grid cells in x-direction
je = round(yinput/dy);
%number of grid cells in y-direction
ke = round(zinput/dz);
%number of grid cells in z-direction
ib = ie+1;
jb = je+1;
kb = ke+1;
is = 2; %location of y-directed current source
js = round(je/2); % side view y plane location
%kobs = 5;
kobs = round(ke/2); % top view z plane location
ex = zeros (ib, jb, kb, tcon);
50
ey = zeros (ib, jb, kb, tcon);
ez = zeros (ib, jb, kb, tcon);
hx = zeros (ib, jb, kb, tcon);
hy = zeros (ib, jb, kb, tcon);
hz = zeros (ib, jb, kb, tcon);
ct = zeros (ib, jb, kb);
tt=ones(ib,jb,kb,tcon)*25;
G=ones(ib,jb,kb)*0.001;
Roe=ones(ib,jb,kb)*1.29;
Er=ones(ib,jb,kb);
sph=ones(ib,jb,kb)*1006;
perf=ones(ib,jb,kb)*0;
met=ones(ib,jb,kb)*0;
therm=ones(ib,jb,kb)*0.026;
tt1=ones(ib,jb,kb)*0;
tt2=ones(ib,jb,kb)*0;
tt3=ones(ib,jb,kb)*0;
sar=zeros(ib,jb,kb);
ez_source = zeros (ib, jb, kb);
ey_source = zeros (ib, jb, kb);
e_source = zeros (ib, jb, kb);
ees = zeros (ib, jb, kb);
ees1 = zeros (ib, jb);
ees2 = zeros (ib,kb);
%**********************************************************************
% Time index setup
%**********************************************************************
ncur = 3;
npr1 = 2;
npr2 = 1;
%**********************************************************************
*
% Material parameters
%**********************************************************************
*
freq1=27e6;
51
%cells_per_wavelength = input ('Enter Cells per wavelength: ');
cells_per_wavelength=5;
%eps = [1.0 47]; %e1=47 a=2.17
%sig = [0 2.17];
cc = 2.99792458e8;
%speed of light in free space
muz = 4.0*pi*1.0e-7;
%permeability of free space
epsz = 1.0/(cc*cc*muz);
%permittivity of free space
aimp1 = 1;
aimp2 = 1; % sqrt (muz/epsz);
%**********************************************************************
*
% Initial calculations
%**********************************************************************
*
lambda = cc/freq1;
%D = lambda/cells_per_wavelength;
%dx = 0.002;
D=dx;
dt = dx/(2.0*cc); %dx = 0.002 time step
da = 1.0; %((cc*dt)/(dx))^2;
db = dt/ muz/ dx;
ca = zeros (ib, jb ,kb , 1);
cb = zeros (ib, jb, kb, 1);
%Shift Object to fit source model
i111=round((antx+ant_objx)/dx);
j111=round((anty+ ant_objy)/dy);
k111=round((antz+ ant_objz)/dz);
for i=1:ix;
i11 = i+i111;
for j=1:iy;
j11 = j + j111;
for k=1:iz;
%i11 = i+3;
%k11 = k+3;
k11 = k+k111;
Er(i11, j11, k11)= EEr(i,j,k);
G(i11, j11, k11) = GG(i,j,k);
Roe(i11, j11, k11) = RRoe(i,j,k);
therm(i11, j11, k11) = ttherm(i,j,k);
sph(i11, j11, k11) = ssph(i,j,k);
52
met(i11, j11, k11) = mmet(i,j,k);
perf(i11, j11, k11) = pperf(i,j,k);
ct(i11,j11,k11)=ct13(i,j,k);
end;
end;
end;
%**********************************************************************
*
% Updating coefficients
%**********************************************************************
*
ca(:,:,:,1)=(1.0-(dt*G)./(2.0*epsz*Er))./(1.0+(dt*G)./(2.0*epsz*Er));
cb(:,:,:,1)=(dt/epsz/Er/dx)./(1.0+(dt*G)./(2.0*epsz*Er));
%**********************************************************************
*
% Create Sources: cosine distribution on a face of horn antenna
%*********************************************************************
a = 0.1;
c = 25.546*a;
yy11 = (yinput -2* a)/2;
yy12 = yy11 + 2*a;
zz11 = (zinput - 2*a)/2;
zz12 = zz11 + 2*a;
source1_y1 = fix(yy11/dy)+1;
source1_y2 = fix(yy12/dy)+1;
source1_z1 = fix(zz11/dz)+1;
source1_z2 = fix(zz12/dz)+1;
kc=1.841/a;
for j = source1_y1:source1_y2;
y=(j-1)*dy;
y1=y-anty;
53
for k = source1_z1:source1_z2;
z=(k-1)*dz;
z1=z-antz;
b = kc*sqrt(y1^2+z1^2);
ph=atan2(z1,y1);
d = besselj(1,b);
d1=besselj(0,b);
dd = -d/b+d1;
e = sqrt(y1^2+z1^2);
f = sin(ph);
g = cos(ph);
if y1^2 + z1^2 <= a^2;
ey_source(is,j,k) = -g^2*d/(kc*b)-f^2*dd/kc;
end;
if y1^2 + z1^2 <= a^2;
ez_source(is,j,k) = -f*g*d/(kc*b) + g*f*dd/kc;
end;
end;
end;
e_source=ez_source.^2+ey_source.^2;
e_source=sqrt(e_source);
eesm=max(max(max(e_source)));
e_source=(e_source)/eesm;
ctm=max(max(max(ct)));
ees=e_source+ct/ctm;
%**********************************************************************
*
% BEGIN TIME-STEPPING LOOP
%**********************************************************************
*
nmax=100;
for n=1:nmax
% if mod(n,10) == 0
%
time = n
% end
%display time progress
54
%**********************************************************************
*
%
Update time container index
%**********************************************************************
npr2 = npr1;
npr1 = ncur;
ncur = mod(ncur+1,3);
if ncur == 0
ncur = 3;
else
ncur = ncur;
end
%**********************************************************************
%
Apply soft lattice Truncation Conditions at the boundaries
%**********************************************************************
%i = 0 case (index =1)
%case where index excludes the boundaries
hy (1, 1:jb, 2:ke-1, ncur) = (hy (2 , 1:jb , 1:ke-2 , npr2)+...
hy (2 , 1:jb , 2:ke-1, npr2)+hy(2 ,1:jb ,3:ke , npr2))/3;
hz (1, 1:je, 2:ke, ncur) = (hz(2, 1:je, 1:ke-1, npr2)+...
hz (2, 1:je, 2:ke, npr2) + hz (2, 1:je, 3:kb, npr2))/3;
%case where k = ke, kb index fails (at max k index for hy, hz)
hy (1, 1:jb ,ke, ncur) = (hy (2, 1:jb, ke-1, npr2)+...
hy (2, 1:jb, ke, npr2))/2;
hz (1, 1:je, kb, ncur) = (hz (2, 1:je, kb-1, npr2)+...
hz (2, 1:je, kb, npr2))/2;
%for k = 1 where index fails (at min k index for hy, hz)
hy (1, 1:jb, 1, ncur) = (hy (2, 1:jb, 1, npr2)+...
hy (2, 1:jb, 2, npr2))/2;
hz (1, 1:je, 1, npr2) = (hz (2, 1:je, 1, npr2)+...
hz (2, 1:je, 2, npr2))/2;
%i = imax case
%case where index excludes the boundaries
hy (ie, 1:jb, 2:ke-1, ncur) = (hy (ie-1, 1:jb, 1:ke-2, npr2)+...
hy (ie-1, 1:jb, 2:ke-1, npr2) + hy (ie-1, 1:jb, 3:ke, npr2))/3;
hz (ie, 1:je, 2:ke, ncur) = (hz (ie-1, 1:je, 1:ke-1, npr2)+...
hz (ie-1, 1:je, 2:ke, npr2) + hz (ie-1, 1:je, 3:ke+1, npr2))/3;
55
%for k = ke, kb where index fails (at max k index for hy, hz)
hy (ie, 1:jb, ke, ncur) = (hy (ie-1, 1:jb, ke-1, npr2)+...
hy (ie-1, 1:jb, ke, npr2))/2;
hz (ie, 1:je, kb, ncur) = (hz (ie-1, 1:je, kb-1, npr2)+...
hz (ie-1, 1:je, kb, npr2))/2;
%for k=1 where index fails (at min k index for hy, hz)
hy (ie, 1:jb, 1, ncur) = (hy (ie-1, 1:jb, 1, npr2)+...
hy (ie-1, 1:jb, 2, npr2))/2;
hz (ie, 1:je, 1, ncur) = (hz (ie-1, 1:je, 1, npr2)+...
hz (ie-1, 1:je, 2, npr2))/2;
%j=0 case (index=1)
ex (1:ie, 1, 1:kb, ncur) = ex (1:ie, 2, 1:kb, npr2);
ez (1:ib, 1, 1:ke, ncur) = ez (1:ib, 2, 1:ke, npr2);
%j=jmax case (index=1)
ex (1:ie, jb, 1:kb, ncur) = ex (1:ie, jb-1, 1:kb, npr2);
ez (1:ib, jb, 1:ke, ncur) = ez (1:ib, jb-1, 1:ke, npr2);
%k=0 case (index k=1)
%case where index excludes the boundaries
ex (2:ie-1, 1:jb, 1, ncur) = (ex (1:ie-2,1:jb,2,npr2)+...
ex (2:ie-1,1:jb,2,npr2) + ex (3:ie,1:jb,2,npr2))/3;
ey (2:ie, 1:je, 1, ncur) = (ey (1:ie-1, 1:je, 2, npr2)+...
ey (2:ie, 1:je, 2, npr2) + ey (3:ie+1, 1:je, 2, npr2))/3;
%for i = ie, ib case where index fails (at max i index for ex, ey)
ex (ie,1:jb,1,ncur) = (ex(ie-1,1:jb,2,npr2)+...
ex (ie,1:jb,2,npr2))/2;
ey (ib,1:je,1,ncur) = (ey(ib-1,1:je,2,npr2)+...
ey (ib,1:je,2,npr2))/2;
%for i=1 case where index fails (at min i index for ex, ey)
ex (1,1:jb,1,ncur) = (ex(1,1:jb,1,npr2)+...
ex(2,1:jb,1,npr2))/2;
ey (1,1:je,1,ncur) = (ey (1,1:je,1,npr2)+...
ey (2,1:je,1,npr2))/2;
ex(2:ie-1,1:jb,kb,ncur) = (ex(1:ie-2,1:jb,kb-1,npr2)+...
56
ex(2:ie-1,1:jb,kb-1,npr2)+ex(3:ie,1:jb,kb-1))/3;
ey(2:ie,1:je,kb,ncur) = (ey(1:ie-1,1:je,kb-1,npr2)+...
ey(2:ie,1:je,kb-1,npr2) + ey(3:ie+1,1:je,kb-1,npr2))/3;
%for i=ie,ib case where index fails (at max i index for ex, ey)
ex(ie,1:jb,kb,ncur) = (ex(ie-1,1:jb,kb-1,npr2)+...
ex(ie,1:jb,kb-1,npr2))/2;
ey(ib,1:je,kb,ncur) = (ey(ib-1,1:je,kb-1,npr2)+...
ey(ib,1:je,kb-1,npr2))/2;
ex(1,1:jb,kb,ncur) = (ex(1,1:jb,kb-1,npr2)+...
ex(2,1:jb,kb-1))/2;
ey(1,1:je,kb,ncur) = (ey(1,1:je,kb-1,npr2)+...
ey(2,1:je,kb-1,npr2))/2;
%**********************************************************************
*
% Update electric fields
%**********************************************************************
*
ex(1:ie,2:je,2:ke,ncur) = ca(1:ie,2:je,2:ke,1).*ex(1:ie,2:je,2:ke,npr1)+...
cb(1:ie,2:je,2:ke,1).*(hz(1:ie,2:je,2:ke,npr1)-hz(1:ie,1:je-1,2:ke,npr1)+...
hy(1:ie,2:je,1:ke-1,npr1)-hy(1:ie,2:je,2:ke,npr1));
ey(2:ie,1:je,2:ke,ncur) = ca(2:ie,1:je,2:ke,1).*ey(2:ie,1:je,2:ke,npr1)+...
cb(2:ie,1:je,2:ke,1).*(hx(2:ie,1:je,2:ke,npr1)-hx(2:ie,1:je,1:ke-1,npr1)+...
hz(1:ie-1,1:je,2:ke,npr1)-hz(2:ie,1:je,2:ke,npr1));
ez(2:ie,2:je,1:ke,ncur) = ca(2:ie,2:je,1:ke,1).*ez(2:ie,2:je,1:ke,npr1)+...
cb(2:ie,2:je,1:ke,1).*(hx(2:ie,1:je-1,1:ke,npr1)-hx(2:ie,2:je,1:ke,npr1)+...
hy(2:ie,2:je,1:ke,npr1)-hy(1:ie-1,2:je,1:ke,npr1));
sar1=abs(ex(:,:,:,ncur)).^2+abs(ey(:,:,:,ncur)).^2+abs(ez(:,:,:,ncur)).^2;
%sar= G.*sar1./(2*Roe);
%**********************************************************************
**
% Source update
%**********************************************************************
**
57
ez(is,source1_y1:source1_y2,source1_z1:source1_z2,ncur) = ...
ez_source(is,source1_y1:source1_y2,source1_z1:source1_z2,1)*...
aimp1 * sin(2*pi*freq1*n*dt);
ey(is,source1_y1:source1_y2,source1_z1:source1_z2,ncur) = ...
ey_source(is,source1_y1:source1_y2,source1_z1:source1_z2,1)*...
aimp1 * sin(2*pi*freq1*n*dt);
%**********************************************************************
*
% Update magnetic fields
%**********************************************************************
*
hx(2:ie,1:je,1:ke,ncur) = da*hx(2:ie,1:je,1:ke,npr1)+...
db*(ey(2:ie,1:je,2:kb,ncur)-ey(2:ie,1:je,1:ke,ncur)+...
ez(2:ie,1:je,1:ke,ncur)-ez(2:ie,2:jb,1:ke,ncur));
hy(1:ie,2:je,1:ke,ncur) = da*hy(1:ie,2:je,1:ke,npr1) + ...
db*(ex(1:ie,2:je,1:ke,ncur)-ex(1:ie,2:je,2:kb,ncur) + ...
ez(2:ib,2:je,1:ke,ncur) - ez(1:ie,2:je,1:ke,ncur));
hz(1:ie,1:je,2:ke,ncur) = da*hz(1:ie,1:je,2:ke,npr1) +...
db*(ex(1:ie,2:jb,2:ke,ncur) - ex(1:ie,1:je,2:ke,ncur) +...
ey(1:ie,1:je,2:ke,ncur) - ey(2:ib,1:je,2:ke,ncur));
%**********************************************************************
*
% END TIME-STEPPING LOOP
%**********************************************************************
*
end;
sar1=abs(ex(:,:,:,ncur)).^2+abs(ey(:,:,:,ncur)).^2+abs(ez(:,:,:,ncur)).^2;
sar= G.*sar1./(2*Roe);
58
%**********************************************************************
*
% Update temperature
%**********************************************************************
*
ncur = 2;
npr1 = 1;
nmax=100;
dtt=0.05;
for n=1:nmax
%**********************************************************************
*
%
Update time container index
%**********************************************************************
npr2 = npr1;
npr1 = ncur;
ncur = mod(ncur+1,3);
if ncur == 0
ncur = 3;
else
ncur = ncur;
end
tt1(2:ie-1,:,:)=(therm(3:ie,:,:).*tt(3:ie,:,:,npr1)-therm(3:ie,:,:).*tt(1:ie-2,:,:,npr1)-...
therm(1:ie-2,:,:).*tt(3:ie,:,:,npr1)+therm(1:ie-2,:,:).*tt(1:ie-2,:,:,npr1))/4 +...
therm(2:ie-1,:,:).*(tt(3:ie,:,:,npr1)-2*tt(2:ie-1,:,:,npr1)+tt(1:ie-2,:,:,npr1));
tt1=tt1/dx/dx;
tt2(:,2:je-1,:)=(therm(:,3:je,:).*tt(:,3:je,:,npr1)-therm(:,3:je,:).*tt(:,1:je-2,:,npr1)-...
therm(:,1:je-2,:).*tt(:,3:je,:,npr1)+therm(:,1:je-2,:).*tt(:,1:je-2,:,npr1))/4 +...
therm(:,2:je-1,:).*(tt(:,3:je,:,npr1)-2*tt(:,2:je-1,:,npr1)+tt(:,1:je-2,:,npr1));
tt2=tt2/dy/dy;
tt3(:,:,2:ke-1)=(therm(:,:,3:ke).*tt(:,:,3:ke,npr1)-therm(:,:,3:ke).*tt(:,:,1:ke-2,npr1)...
therm(:,:,1:ke-2).*tt(:,:,3:ke,npr1)+therm(:,:,1:ke-2).*tt(:,:,1:ke-2,npr1))/4 +...
therm(:,:,2:ke-1).*(tt(:,:,3:ke,npr1)-2*tt(:,:,2:ke-1,npr1)+tt(:,:,1:ke-2,npr1));
tt3=tt3/dz/dz;
59
tt(:,:,:,ncur) = tt(:,:,:,npr1)+ dtt*(tt1+tt2+tt3+sar.*Roe-(3600*1057*perf.*(tt(:,:,:,npr1)37)/6000)+met)./Roe./sph;
end;
is=2;
%**********************************************************************
*
% Visualize fields
%**********************************************************************
*
tmax=nmax*dtt/60;
ee=tt(:,:,:,ncur);
[ix1,iy1,iz1]=size(ee);
i=1:ix1;
x1=(i-1)*dx;
i=1:iy1;
y1=(i-1)*dy;
i=1:iz1;
z1=(i-1)*dz;
iz2=round(iz1/6)+1;
inx=ix1*iy1*iz1;
figure(1);
for isub=1:iz1;
subplot(iz2,6,isub);
ees1=ee(:,:,isub);
pcolor(x1,y1,ees1');
colorbar;
shading flat;
axis off;
end;
xlabel('x,m');
ylabel('y,m');
title(['Temperature, degress C after ',num2str(tmax),' minutes']);
ees=abs(ees);
figure(2)
for isub=1:iz1;
60
subplot(iz2,6,isub);
ees1=ees(:,:,isub);
pcolor(x1,y1,ees1');
colorbar;
shading flat;
axis off;
end;
title('Electric field, Volts/meter');
xlabel('x,m');
ylabel('y,m');
[xp,yp]=ginput(1);
figure(3)
iz2=round(iy1/6)+1;
np1=round(yp/dy)+1;
ees2(:,:)=ees(:,np1,:);
pcolor(x1,z1,ees2');
colorbar;
shading flat;
axis off;
title('Electric field, Volts/meter');
xlabel('x,m');
ylabel('z,m');
[xpp,ypp]=ginput(1);
zp=ypp;
end;
end;
close(1);
% -----------------------------------------------------------% Read the current directory and sort the names
% -----------------------------------------------------------function load_listbox(dir_path,handles)
cd (dir_path)
dir_struct = dir(dir_path);
[sorted_names,sorted_index] = sortrows({dir_struct.name}');
handles.file_names = sorted_names;
61
handles.is_dir = [dir_struct.isdir];
handles.sorted_index = [sorted_index];
guidata(handles.figure1,handles)
set(handles.listbox1,'String',handles.file_names,...
'Value',1)
set(handles.text1,'String',pwd)
% --- Executes during object creation, after setting all properties.
function listbox1_CreateFcn(hObject, eventdata, handles)
usewhitebg = 1;
if usewhitebg
set(hObject,'BackgroundColor','white');
else
set(hObject,'BackgroundColor',get(0,'defaultUicontrolBackgroundColor'));
end
62
BIBLIOGRAPHY
1.
American Cancer Society, “Progress Report on Reducing the Global Cancer
Burden”, presented at the 20th World Cancer Congress. August 2008.
2.
R. Bansal, “Battling cancer: the latest on microwave hyperthermia”, IEEE
Microwave Magazine, Volume 6, Issue 3, Sept. 2005 Page(s):32 – 34.
3.
E.L. Jones, J.R. Oleson, L.R. Prosnitz, T.V. Samulski, Z. Vujaskovic, D.Yu, L.L.
Sanders, and M.W. Dewhirst, ‘Randomized trial of hyperthermia and radiation for
superficial tumors’, J Clin. Oncol. 2005 May 1;23(13):3079-85.
4.
R. Knoechel, ‘Capabilities of Multiapplicator systems for focused hyperthermia’,
IEEE Trans. Microw. Theory Tech., Vol.31, pp. 70-73, Jan. 1983.
5.
M. Popovic and L. Duong, “Phased array for microwave hyperthermia: a
preliminary study in a computational muscle phantom”, 2005 IEEE International
Symposium on Antennas and Propagation, Volume 2B, 3-8 July 2005 Page(s):788 – 791.
6.
Sabariego, R.V.; Landesa, L.; Obelleiro, F., “Synthesis of an array antenna for
hyperthermia applications”, IEEE Transactions on Magnetics, Volume 36, Issue 4, Part
1, July 2000 Page(s):1696 – 1699.
7.
B.P. Kumar, N. Karnik & G.R. Branner, ‘Near-field beam-forming for
hyperthermia applications using waveguide aperture arrays’, (invited paper), Proceedings
of the 2002 Progress in Electromagnetics Research (PIERS) Conference, Boston, p. 345
(abstract), July 2002.
63
8.
C.Y. Huang, Design And Optimization Of Nine Element Array Antenna For Deep
Focused Hyperthermia Applications, M.S. Thesis, California State University, Sacramento,
2002.
9.
C.A. Balanis, ‘Antenna Theory: Analysis and Design’, John Wiley & Sons, New
York, 1997.
10.
DICOM File Format. Retrieved on April 21st, 2010 from World Wide Web:
http://download.oracle.com/docs/cd/B28359_01/appdev.111/b28416/img/dicom004.gif
11.
The Mathworks Inc., Graphical User Interface Applications. Retrieved on March
13th, 2010 from World Wide Web:
http://www.mathworks.com/access/helpdesk/help/pdf_doc/matlab/buildgui.pdf