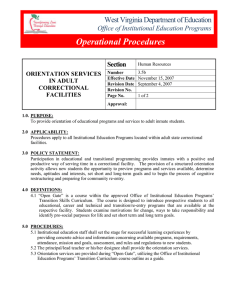
CORRECTIONAL FACILITY CLINICAL CURRICULUM James Avery
advertisement

CORRECTIONAL FACILITY CLINICAL CURRICULUM James Avery B. S. N., University of Phoenix, Sacramento, 2005 Ken Bowman B. S. N., California State University, Stanislaus, 2004 PROJECT Submitted in partial satisfaction of the requirements for the degree of MASTER OF SCIENCE in NURSING at CALIFORNIA STATE UNIVERSITY, SACRAMENTO SPRING 2010 CORRECTIONAL FACILITY CLINICAL CURRICULUM A Project by James Avery Kenneth Bowman Approved by: , Committee Chair Duane DeAmicis, F.N.P.-C., M.S.N. , Reader Ann Stoltz, Ph.D. R.N., Division of Nursing ______________________ Date ii Students: James Avery Ken Bowman I certify that these students have met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the Project. ______________ Date Ann D. Stoltz, PhD., R.N. Division of Nursing iii ABSTRACT Correctional healthcare training has little documented curriculum. The purpose of this project was to assess the need for curriculum development and present a working curriculum. The first component was accomplished by assessing the healthcare concerns associated in this patient population including infectious disease, behavioral treatment, palliative care, healthcare maintenance, and safety precautions. Assessment of current practices and learning strategies were discussed. After evaluating these needs and practices, a curriculum utilizing Leininger’s theory of culture care, was developed in collaboration with University of California, Davis and California Medical Facility, Vacaville. Course descriptions, expectations of the student, and objectives for a two week clinical rotation to be offered to University of California, Davis Family Nurse Practitioner/Physician Assistant students were outlined. , Committee Chair Duane DeAmicis, F.N.P.-C., M.S.N. ______________________ Date iv TABLE OF CONTENTS List of Figures………………………………………………………………...………….vii Chapter 1 INTRODUCTION ...........................................................................................................1 Rationale…………………………………………………………………………..1 Significance and Need…………………………………………………………….2 Summary…………………………………………………………………………..9 2 REVIEW OF LITERATURE .........................................................................................11 Introduction………………………………………………………………………11 Current Strategies………………………………………………………………...12 Pedagogical Strategies…………………………………………………………...22 Summary…………………………………………………………………………33 3 THEORETICAL FRAMEWORK ..................................................................................34 Introduction………………………………………………………………………34 Five Major Theory Assumptions………………………………………………...35 Summary…………………………………………………………………………38 4 PROJECT OVERVIEW .................................................................................................39 Intent of Project…………………………………………………………………..39 Progression of Project……………………………………………………………39 Methodology of Student Sampling………………………………………………41 v Discussion of Project Syllabus…………………………………………………...44 5 CONCLUSION ...............................................................................................................52 Introduction………………………………………………………………………52 Evaluation………………………………………………………………………..53 Limitations……………………………………………………………………….54 Literature Review Impact………………………………………………………..56 Implications for Nursing…………………………………………………………57 Summary…………………………………………………………………………58 Appendix A Budget ..........................................................................................................60 Appendix B Consent of Participation ...............................................................................61 Appendix C Study Questionnaire ....................................................................................63 Appendix D Syllabus ........................................................................................................65 References ........................................................................................................................130 vi LIST OF FIGURES 1. Figure 1. Proposed Content Areas for Correctional Health Care Curricula……16 2. Figure 2. Clinical Preventive Services – Health Promotion……………………31 vii 1 Chapter 1 INTRODUCTION Nursing has been thought of as a dynamic profession in which many individuals provide care for a variety of patients. As the nursing shortage remains, there is a small population that does not receive a great deal of press. Correctional facility nursing is a specialty field requiring the most dynamic of professionals that are capable of working with a wide variety of patients. This project will discuss the purpose and significance of developing a correctional facility clinical curriculum for health care providers. A summary of all the literature researched will be presented as well as the modalities that were used to obtain the information. Theoretical framework utilized in the project will be discussed. The project overview will be explained. A conclusion will summarize and express recommended changes as seen fit. Rationale Previously, the University of California, Davis (UCD) Family Nurse Practitioner/Physician Assistant program and California Medical Facility, Vacaville have operated in conjunction to allow practitioner students the unique opportunity to receive medical training in the prison system. The UCD Family Nurse Practitioner/Physician Assistant program has not adopted a specific curriculum for the experience. Students were expected to attend a two day orientation that discussed safety and security concerns within the medical facility. Currently the California Medical Facility, Vacaville site is the only prison hospital facility within the entire California Department of Corrections. More than 3,000 inmates are receiving medical care in the facility (California Department, 2 2009). These numbers are likely to increase as our population increases. A structured curriculum can assist students in obtaining an excellent educational experience while providing optimal care for inmates. Significance and Need The significance and need for a structured curriculum will be identified for two populations; the patient (inmates at the California Medical Facility, Vacaville) and the students (UCD Family Nurse Practitioner/Physician Assistant students). Current knowledge base and practice deficiencies for healthcare providers to justify curriculum development include infectious disease, chronic disease management, preventative management, defining professional role, behavioral health, transitional care, and palliative care. Inmate Needs. Infectious disease has always been considered a threat to prisoners and healthcare providers. Inmates sharing close quarters and not receiving regular healthcare are more at risk for obtaining and, more importantly, spreading communicable diseases. Allen, Spaulding, Osei, Taylor, Cabral, and Rich (2003) explained, “The challenge of evaluating and caring for as many as one third of all incarcerated individuals with hepatitis C is daunting and has been undertaken despite limited clinical experience relevant to this special population” (p. 187). Allen et al. (2003) go on to report that infection rates of Hepatitis C are 8.8 to 22.8 times greater in the state and federal correctional facility in proportion to the general public. There is a need to accurately diagnose Hepatitis C in a timely manner. Once the diagnosis is made, prompt medical intervention needs to be 3 initiated. Continuation of Hepatitis C treatment must remain a high priority. Most importantly, the authors report that practitioners need to be attentive in screening practices. Why are communicable diseases so communicable in prisons? Perceptions by inmates can prove to be deterrents of early diagnosis. Hepatitis C is one of several infectious diseases that hinders healthcare in the correctional facilities. Several authors have offered discussion for change in order to be preemptive. Khaw, Stobbart, and Murtagh (2007) suggested, “…optimizing testing pathways that support appropriate testing at appropriate times during a prisoner’s stay in prison, ensuring adequate pre- and post-test discussion, and by developing care pathways for HCV that enable seamless continuity of care” (p.5). Health care providers (or students) must be diligent when assessing this population for communicable diseases. Tuberculosis is another communicable disease that healthcare providers in the correctional healthcare system should focus on. Tuberculosis requires a great deal of intervention from healthcare providers in the correctional facilities of America. Discrepancies occur in tuberculosis treatment inside the correctional facilities versus the treatment provided in the general public. MacNeil, Lobato, and Moore (2005) clarified, “Tuberculosis case rates in prison systems remain higher than in the general population. Inmates with TB are less likely than non-inmates to complete treatment” (p. 1800). In some cases inmates are released before the course of treatment is scheduled to be completed. These inmates are then lost in the gray area of initiating a new life and maintaining healthcare needs. The consequences of correctional healthcare provisions 4 transitioning to general public healthcare become a great concern for the inmates as well as the general public. Essentially tuberculosis is more common in the correctional facility and treatment is not always successful (MacNeil et al., 2005). Human Immunodeficiency Virus (HIV) is also of great concern. Multiple factors contribute to HIV infection in the prison system. The variables include unprotected sex, drug use, high risk behavior, and delay in early diagnosis (Macher, Kibble, & Wheeler, 2006). Macher et al. (2006) explained that other factors included a prison population that is typically uneducated and that the turnover rate of health care providers tends to be high. All of the listed factors contribute to an increased vulnerability for becoming infected with HIV. Health care providers need to incorporate HIV into their educational experience. Macher et al. (2006) suggested, “Correctional staff and inmates should be educated about the consequences of unprotected sex and the signs and symptoms of acute retroviral syndrome” (p. 670). Smoking cessation is also of great concern for the prison population. One poll, in the Polish prison system, indicated that almost 81% of the inmates were smokers and another 12% were ex-smokers, with one of the biggest instigators of smoking being higher levels of stress (Sieminska, Jassem, and Konopa, 2006). Sieminiska et al. (2006) also revealed that almost 50% of smokers were aware of the health risks associated with smoking, and that 75% of smokers had attempted to quit at least once. The conclusions that could be obtained were that cigarette smoking is common among inmates and that intervention could possibly require more assistance from health care providers in comparison to the general public. Also of note, 40% of prisoners indicated that a reward 5 system would be beneficial in motivating prisoners to attempt smoking cessation (Sieminska et al., 2006). Smoking poses a significant need that needs to be addressed with curriculum development so that health care providers are better able to handle this intervention. Patient education in regards to risky health behavior is of great concern and contributes to chronic illness in the prison system (Conklin, Lincoln, & Tuthill, 2000). To obtain the information they were seeking, Conklin et al. (2000) conducted interviews with over 1,000 inmates within three days of their arrival to the facility. The resulting data collected showed a high rate of chronic health problems as well as risky health behaviors and habits. This data also showed the need to provide increased education, intervention, and preventive treatment within the correctional facility as the inmates’ transition back into the community or to a higher level of incarceration (Conklin et al., 2000). Mental illness has been associated with high risk behavior (Howerton, Byng, Campbell, Hess, Owens, & Aitken, 2007). Howerton et al. (2007) identified many inmates as high risks of being a harm to themselves. Research suggested that this area of health care concern had been of significant importance and was lacking in the care given by health care providers (Howerton et al., 2007). Data proposed from pre and post release interviews revealed that few inmates were likely to seek help for mental distress even though some had considerable emotional problems (Howerton et al., 2007). The greatest problem was lack of trust in providers and the fear of being stigmatized as having a mental illness and thus being labeled. Howerton et al. (2007) concluded: 6 Like most people, the respondents in this study wanted to feel listened to, acknowledged, and treated as individuals by health professionals. By ensuring that a positive precedent is set, particularly for sceptical [sic] groups such as exprisoners, general practitioners and prison doctors may be able to encourage future help seeking. Information specifically designed for prisoners is needed to help to de-stigmatise [sic] mental illness, and preparation for release should include provision of information about access to health and social services. Awareness training for health professionals is recommended: trust might be fostered in this population by seemingly trivial gestures that indicate respect. (p.303). It is important for health care providers to be trained to treat inmates with respect, as this might lead to an opportunity to build trust and provide better care for the often multiple needs of the inmate. Continuum of care, especially upon release from prison has also been considered a significant concern for inmates (Loeb, Steffensmeier, & Myco, 2007). Data collected by Loeb et al. (2007) indicated that older inmates were fairly optimistic in regards to their health care after release because of supposed family support and access to health care. This, in reality, may not be available to them at the level they suppose (Loeb et al., 2007). Another concern is that those inmates who did not qualify for health care aid, or did not identify themselves as high risk, may relapse into risky behavior. Loeb et al. suggested that more research needs to be conducted to provide ways to better prepare the older inmates for release into society and to the community’s health care system. 7 Prison health care involves the continuum of care provided to an individual during the course of a lifetime including the end of life. Linder and Meyers (2007) provided a case study of an inmate in his late 40’s in their article, Palliative care for Prison Inmates: 'don't let me die in Prison'. The case study involved an inmate serving a 10 year sentence for manslaughter. During the incarceration he developed terminal lung cancer. Eventually the inmate was referred to hospice care and for medical parole. This specific inmate had not been granted medical parole during the time of the article. Linder and Meyers interviewed the inmate, the prison physician, and a prison psychologist involved with the inmate’s care. The interviews focused on different aspects of providing care to a dying inmate. Throughout the interview process several deficiencies were noted. These deficiencies were not that uncommon (Linder & Meyers, 2007). Linder and Meyers (2007) explained that concerns for end-of-life care were noted to be site specific, as only 25 of 49 jurisdictions from a previous survey conducted in 2001 had hospice programs. The greatest worries were noted to be symptom relief and lack of family involvement (Linder & Meyers, 2007). Student Needs. In 2005, Constance Weiskopf, Director of Nursing at University of Connecticut Health Center, published an article entitled Nurses’ Experience of Caring for Inmate Patients, in which her main goal was to explore the everyday experiences of nurses delivering health care to inmate patients in a correctional setting. Weiskopf carried out indepth interviews with nine registered nurses who were employed in a correctional setting and were able to discuss that experience. The data collected was comprised of the 8 experiences and frustrations that these nurses had undergone while working in the correctional settings. Weiskopf uncovered five central themes in regards to these experiences. These themes include: 1) Negotiating Boundaries Between Custody and Caring, 2) Struggling to Create a Caring Environment, 3) Striving to Turn a Life Around, 4) A Risky Situation, and 5) Staying Vigilant. These five central themes were the categories that the nurses experiences fell into. In summary of her interviews and analysis, Weiskopf (2005) makes the following statements: Consideration needs to be given to the numerous frustrations and challenges these prison nurses faced in order to enhance therapeutic care while balancing the need for security. To address these complex issues, nurse administrators must model caring behaviors, such as soliciting honest feedback about patient care and/or custody issues, and maintaining consistent, direct interactions with staff. (p. 342). Unfortunately, despite the most sincere concerns of health care providers, patients in the correctional facilities may not always be appreciative of these efforts. The healthcare provider must always be aware of ones own safety first. Without taking care of oneself first and foremost the health care practitioner may not be able to return the next day to provide care. Safety first! Inmate-made Weapons in Prison Facilities: Assessing the Injury risk is a quantitative article written by Lincoln, Chen, Mair, Bierman, and Baker (2006) that looked into the harm that occurs to health care providers. Lincoln et al. (2006) reported, “The injury rate for staff was 1/ 1000 workers per year. The annual cost of injuries for time lost and medical care for staff was estimated at $1,125,000 in these 70 prisons” (p. 195). Attention to the most common types of weapons, and the materials to 9 make those weapons can alert the practitioner to potential harm. An increased knowledge base about these dangers can potentially save a life. Summary There is ample evidence that training specific to the needs of providing healthcare in correctional facilities warrants development. Several concerns have been shown in this introduction that present the discrepancies of care between incarcerated patients in comparison to the general public. Articles discussed in this introduction involved medical topics including infectious diseases, behavioral concerns, transitional health care concerns, and dying. Holistic approaches to the healthcare of inmates were also presented regarding current inmate and nursing concerns. Safety concerns were assessed. End of life topics specific to incarcerated health care provision were also addressed in this introduction. Every concern had a concept in common, the need for specialty training to obtain optimal outcomes. This knowledge deficit can be decreased by beginning to work with healthcare providers early in their education and developing tailored course curriculums. Every individual is entitled to optimal care. “In addition, the nurse supports initiatives to address barriers to health, such as poverty, homelessness, unsafe living conditions, abuse and violence, and lack of access to health services” (American Nurse’s Association, provision 8.2, 2008). Curriculum development has the potential for primarily benefiting healthcare providers in their educational journey. The intent of this project is to directly assist UCD practitioner students in preparation for clinical intervention at California Medical 10 Facility, Vacaville. Indirectly the development of a proper curriculum can improve the lives of inmates and the public that awaits their reestablishment into society. 11 Chapter 2 REVIEW OF LITERATURE Introduction Medical training in prisons is not a new concept and is documented as far back as 1979 (Kaufman, Holbrook, Collier, Farabaugh, Jackson, & Johnston, 1979). Legitimate and ethical training in the prison environment is relatively new in comparison to medical training as a whole. As shown in the introduction, a prison provides a rich variety of disease processes and challenges that are not seen as often in the general public. Training programs that have undertaken the challenges of training practitioners in this unique environment will be discussed in this chapter. This constantly growing population and ever-changing dynamic area was once an untapped training resource. The following chapter will provide a literature review of previous and current programs that have taken advantage of this Petri dish of education. A systematic review of literature assisted in identifying concepts for syllabus formation. Several resources were utilized during research. Libraries at Memorial Hospital’s Association, St. Joseph’s Medical Center, University of California, Davis, and California State University (both Sacramento and Stanislaus Campus) were of great assistance during the research process. Approximately 150 articles were viewed and of those articles approximately 75 articles were discussed by both authors for the purposes of curriculum needs and development. Through this process it was agreed that approximately 30 articles would be of benefit, relevant, and competent for use. The critique process was performed verbally meeting multiple criteria as suggested by Burns and Grove (2005). 12 Articles were assessed for their direct influence for the care of the incarcerated population and pedagogy strategies for curriculum development in health care. Historical perspectives were researched in order to identify shortcomings and prevent similar mishaps in curricular development. Historically, documented educational programs specific to practitioners training in the prison system has been limited. A comprehensive literature review indicated that contemporary training began approximately 35 years ago (Kaufman et al., 1979). Kaufman et al. (1979) explained, “In 1975 a group of students toured the Los Lunas facility, a small prison farm 30 miles south of Albuquerque, and selected it as the setting of their longitudinal elective experience” (p. 926). Since the 1970s many medical schools have begun rotating students through the prison. During the past 40 years, medical training programs have progressively initiated more structure to take greater advantage of this symbiotic relationship. The following chapter will provide a literature review of previous and current health care programs that have either utilized, or are currently utilizing the prison environment for training. A systematic review of literature assisted in identifying generalized concepts for syllabus formation. Discussion of pedagogical strategies will be presented for adaptation in curricular development. Current Strategies Concepts for curriculum development need to address many concerns. Factors that precipitate curriculum content include the needs of the learner, needs of the beneficiaries, and the desired message to be conveyed. These needs were first identified in chapter one. Individual disease processes for consideration were first evaluated by 13 statistics presented from the California Death Review Committee (CDRC) for the most recent year available, 2006 (Imai, 2006). The purpose of the review was to evaluate deaths that occurred in California’s prison system dependent upon preventable, nonpreventable causes, and possibly preventable deaths. Each death that occurs in the prison system is evaluated by a physician and then presented to the CDRC. The committee meets two to four times monthly to review the deaths. Eventually, this data proposes medical deficiencies that occur in prison health care. Recommendations can then be made. The retrospective study identified multiple limitations that included poorly organized documentation, no standardized templates, misfiling, and analysis dependent upon a single viewer. Despite these limitations, there are several significant facts that occur. The Imai (2006) reported that a total of 319 ‘non-preventable’ deaths were identified. Over 50% were documented as cancer (105), end-stage liver disease (53), and sudden cardiac arrest (28). In the case of ‘preventable deaths’, there were 18 identified causes. The top three contributors included asthma (6), sudden cardiac arrest (3), and congestive heart failure (2). ‘Possibly preventable deaths’ were also considered. A total of 48 deaths were identified in this category. Top contributors identified were sudden cardiac arrest (5), coccidioidomycosis (4), and AIDS (4). It is important that conceptual development of a curriculum address these disease processes. Several programs have been developed over the years to incorporate prison health care into training modalities. In March of 2007, representatives of primary care from Massachusetts, Texas, California, Connecticut, Pennsylvania, Maryland, Rhode Island, the National Commission on Correctional Health Care (NCCHC), and the Federal Bureau 14 of Prisons met to discuss the future of prison health care and training (Hale, Brewer, & Ferguson, 2008). This retrospective investigation of costs had similar limitations of any retrospective investigation: interpretation concerns, possibly incomplete information, and potential biasness (the authors listed were all medical personnel). Further concerns regarding this specific article was a lack of information detailing the method of data collection. The reader is left to ponder how information was collected. Trust is made that the authors used appropriate and accurate references. Several references for this article have been utilized in similar research articles of this nature. Six references were either government agencies or universities. Physicians, nurse practitioners, nurse educators, faculty, and administrators were the participants that represented the various states. Hale et al. (2008) concluded, “All agreed that correctional health offers unparalleled opportunities for primary care research on clinical outcomes for a unique population and setting that offer rich experiences for health professions education and practice” (p. 278). These entities recognized the benefits for all parties concerned as well as the special needs of this specific population. Hale et al. (2008) noted, “The increasing focus on inmate rights, as well as the growing number and diversity of prisoners, heightens the need and opportunity for correctional health as a profession and a specialty” (p. 284). The future of health care in this field requires special training. Objective data reinforcing benefits of training was of concern for the NCCHC. Texas provided the proof in financial benefits. Hale et al (2008) reported that the Texas prison health care system was able to save an estimated $215 million during their initial six years. This savings was reported by improving goal results in diseases, such as; 15 decreased mean glucose levels in type one diabetes patients, lowering low-density lipoproteins levels, and lowering blood pressure in essential hypertension patients. Mortality rates were reduced in chronic diseases, especially AIDS and asthma. University of Massachusett’s Medical School and the Graduate School of Nursing collaborated with the Massachusetts’ Department of Corrections and developed six main themes in order to develop a curriculum (Hale et al., 2008). The six themes were further broken down and competencies were developed. Hale et al. (2008) identified these six themes as: “(a) characteristics of the population being served, (b) prevalent conditions requiring clinical expertise, (c) public health opportunities in correctional facilities, (d) ethics, (e) medical-legal issues, and (f) the correctional health system, structure, and administration” (p. 287). The themes form the basic foundation for curriculum development while allowing for flexibility. The brainstorming led to proposed content area at the University of Massachusetts and will assist in developing the UC Davis proposed curriculum. (Hale et al., 2008, p. 288) (Figure 1) 16 Figure 1. Proposed Content Areas for Correctional Health Care Curricula 1. Tracking your patient orders to advocate for them and make sure your orders are executed, that I, being accountable for your patient’s outcomes. 2. Develop the attitude, “I am the one who has to make sure that things get done.” 3. If you are used to making sure things happen, you do well in the system. 4. If you do not feel responsible for the list of patients you are scheduled to see and follow up on each one who does not show up, then it will not work in corrections. 5. Morbidity around substance abuse and trauma and how it affects inmate behavior and relationships with health care providers, fellow inmates, and correctional officers. 6. 23% of inmates have a history of a gunshot wound. 7. Many inmates were abused as children. 8. Patient advocates against an authoritarian system that may try to use health care as a punishment or reward. 9. The ethics surrounding the question: Are we teaching folks to work in a use-offorce environment? 10. How to work in a chain-of-command environment with reporting relationships as well as command relationships. 11. Understanding how our security colleagues view situations and events compared to how we might view the same event. 12. Use of and formularies consisting of more classic drugs versus the newer, more well-known, highly consumer-marketed drugs. 13. Treatment plans for incarcerated persons might have to differ from those for persons on the outside while maintaining eh standard of care. 14. Patients may choose not to comply, because if they improve, they may have to return to general population or to a different facility where they do not want to go. 15. Ethics should be imbedded; seem to lose sight of patient advocacy role. 16. Not to becoming numb to the situations you are facing. 17. Biggest jeopardy is in female prisons with female nurses. Female inmates have tremendous needs and nurses may eventually shut off. 18. Investigate how health care professionals might feel about the various crimes the inmate may have committed and how that could affect care. Explain the rationale and the value to the health care professional of not knowing the crime. While not all principals are applicable to specific curriculum, many of the idea can be utilized. Nova Southeastern University College of Osteopathic Medicine initiated a pilot training program for third and fourth year medical students that began in 2000 17 (Alemagno, Levy, & Wilkinson, 2004). During the program, students received specific orientations, and directed readings. The actual experience was performed under boardcertified preceptors. Several issues that were addressed during the preparation for the experience included aspects unique to the correctional setting: specific disease pathologies, student concerns, security of all parties, and individual safety issues. This article provided analysis of the subject through qualitative research. The first two years of the program provided 53 students rotating through the experience for one month at a time. Research data was requested from the entire population of participants during the time of implementation. There were 33 responses. Limitations were more subjective based. A student with a poor experience tended to be more verbal about that specific experience. The Nova Southeastern University College noted that curriculum needed to be tailored to the needs of the student as well as the inmates. Developing a curriculum for optimal benefit requires knowledge of basic health care principles and forming a strong knowledge base of the target population. Early programs (and even programs today in their infancy) entered into this rewarding field of training with apprehension and to some degree, confusion. Alemagno et al. reported (2004), “Students requested more structured curriculum and more opportunities to develop content understanding of the unique clinical aspects of prison health care” (p. 123). Alemagno et al. (2004) concluded that the benefits associated with students learning in the prison system are subjective as well as objective. Most of the inmates are typically physically older than their chronological age. Patients frequently suffer from 18 chronic illness and have a multitude of disease processes including infectious and psychological. Given this unique blend of circumstances, students can gain access to pathology not often seen in the general public. During training, many students find the experience rewarding and this exposure may lead to better recruitment for health care providers in the prison system. Students receiving training through the Nova Southeastern University College reported encouraging results. Alemagno et al. (2004) explained, “The findings indicate that students had positive experiences related to continuity of care, access to pathology, access to procedures, and exposure to a unique managed care model” (p.123). Prisons provide an abundance of training, for those allowed to participate. One concern reported by Alemagno et al. (2004), was that students spent more time watching than doing. Initiating learning in a new environment also means initiating teaching in a new environment. Current health care providers might not have experience in teaching due to a lack of exposure in working with students. Curriculum content rarely addresses concerns of this nature (and nor should this be a portion of the curriculum). The concern must be addressed at a teacher and preceptor level. Students should receive instruction for different options in case the student is not gaining maximal benefit from working with an inexperienced preceptor. In order to alleviate this concern, curriculum should be shared with staff members, as well as judicial selection of preceptors. Students not participating (or not allowed to participate) at a substantial level defeats the purpose of the training experience; students, current providers, and inmates all lose out. 19 According to Alemagno et al. (2004) safety must be addressed. During the literature review for this project, there was a dearth of information regarding actual and potential harm to providers and students. Alemagno et al. (2004) went on to explain that even more confusing is the fact that information presented in this discussion does not take into account providers that attended a fully resourced training program with a developed curriculum. Curriculum derived solely from previous experiences at other facilities is not adequate. Improper training could be extremely dangerous and harmful to all involved parties. Curriculum developed specifically for training in the prison setting benefited students in alleviating fears and preparing students for common health care concerns according to Alemagno et al. (2004). Students at Nova Southeastern University College were apprehensive about safety and their ability to care for such potentially complicated patients. The program developed training specific for safety and treating more common pathologies. As the students in the first year of the program completed their rotation many students reported appreciation for the preparation. Results from this first class have encouraged future classes to take advantage of the training. There are currently an average of 72 students rotating through the rotation a year and an unspecified number of students on a waiting list to enter the program (Alemagno et al., 2004). Medical students, as well as midlevel practitioner programs, have recognized an increasing shortfall in providing care for inmates (Reimer, 2007). While answering the need for cares in this population, many colleges are still just beginning to capitalize and develop programs focused on this population. Reimer (2007) reported that recently the 20 University of Colorado in Colorado Springs adopted a program designed for advanced practice nursing in the correctional facility (Reimer, 2007). The Colorado Department of Corrections surveyed 400 health care personnel. Approximately 34 percent of those individuals responded. Through the use of qualitative surveys, the college was able to determine that inmates with addictions and mental illness needed to be a priority for improvement in health care. While the article predominantly focuses on a proposed model, research provided in the article gave ample background for the intended intervention. Limitations included a lack of follow up in assessment of intervention. Readers must be concerned if the proposed model is effective. The proposed model may be open for debate, however the research provided can be utilized in developing a proposed curriculum. Key points of concern were identified by Reimer (2007). Medical components of the proposed model were similar to other literature that has been discussed: infectious disease, chronic illness, psychological aspects, and safety. This article does explore other issues as well, including manipulation and communication. As society has evolved, so has the concern for inmates. Worldwide media, awareness, and a growing prison population that needs to be reintroduced into society have spurned ethical concerns for this vulnerable population (Reimer, 2007). Reimer addressed several ethical concerns regarding prison health care that warrant consideration. Atrocities occurring to prisoners for training purposes have been common knowledge with the most abominable acts occurring during the second World War in Germany. Perhaps Fyodor Dostoevsky had said it best, “The degree of civilization in a society can be judged by entering its prisons” 21 (Quotationspage.com, 2007). When training practitioners in the prison environment, the training programs must realize that the patient population is also at increased risk for mistreatment or lack of treatment. These unfortunate circumstances have not occurred without reason. Reimer reported that many patients fabricate signs and symptoms of disease states in order to go to the clinic. In many cases complaints are true, but extremely exaggerated. These tendencies make training difficult for newer practitioners that may still be learning simple disease processes as well as fostering skepticism for the care of inmates. Situations of this nature require the resources of an experienced practitioner. Ethical concerns bridge beyond just the mere communication of disease processes between practitioner and patient. Reimer (2007) reported that many patients in the incarcerated population come from a variety of backgrounds with a great deal of diversity and disparity. Many social-cultural concerns may play a part in the care of the patients. Much of the prison population has come from backgrounds that did not have adequate healthcare before, which in turn may foster skepticism towards practitioners. This population has a high percentage of individuals that did not receive preventive care before and were involved in high-risk behaviors including substance abuse. More importantly the healthcare practitioner must understand the dynamics of interaction. “The interface between security and health care may be a source of stress for correctional employees; however, the interaction between these two essential functions is critical to successful corrections management” (Reimer, 2007, p. 164). 22 Texas initiated one of the largest programs dedicated to training practitioners in the prison environment in 1994 (Raimer & Stobo, 2004). The program remains intact and has flourished as a perfect example of symbiotic partnership between care provided to inmates and educational experiences for medical students. Throughout the history of the current health care delivery system in the Texas’ prison system the program has evolved to include special interventions in order to improve care and even reduce the cost of health care in the prisons (Raimer & Stobo, 2004). Texas’ system developed groundbreaking interventions by initiating standard disease-management protocols, a common formulary, educational programs for patients and providers, chronic care group clinics, telemedicine, and electronic medical records (Raimer & Stobo, 2004). Unfortunately this retrospective article did not provide strategies for intervention. Benefits of current intervention were discussed and show promising results for the use of academic medicine in the prison population. Pedagogical Strategies Student characteristics and education are the primary concern of this project. Discussing diabetes with sixth grade students versus second year medical students will require massive tailoring of the subject in order to convey the necessary information. While this difference in education levels and student characteristics is easily recognizable, there are more subtle examples of teaching methodologies being tailored for student variance. The first article by Jessee, O’Neill, and Dosch (2006) to be discussed is centered on the needs of undergraduate dental students. The article reviewed multiple reports from previous studies as well as personalities that are identified and then 23 matched with distinct methodologies to obtain optimal teaching methodologies. Several disparities were noted in the reports. Examples of problems addressed in these reports include overcrowded curricula that do not allow for student reflection; outdated information representing the past rather than the future; inadequate link with medicine; and an inability to prepare and stimulate students to be lifelong learners. (Jessee, O'Neill, & Dosch, 2006, p. 644) The article was able to identify several personality types based upon a survey. These students were offered different teaching methodologies that would tend to cater to their needs. Eventually the authors were able to offer multiple benefits that were derived from offering more personal curriculum to the dental students. Teaching strategies that promote the optimal information sharing and application require effective pedagogy manipulation. Curriculum development requires that all learning theories be explored and then the most successful curriculum be applied to a specific learning audience. In some cases, a hybrid of learning theories may be necessary to optimize the education experience. Learning theories can be broken down into five different orientations including: behaviorist, cognitivist, humanist, social learning, and constructivist (Torre, Daley, Sebastian, & Elnicki, 2006). The major limitation of this qualitative analysis is a lack of reference for success. While the article primarily focused on discussing the differences, there was little reference as to how successful each strategy was in specific arenas. Benefits of this article included defining the different strategies as well as the implications each could have on medical education. 24 According to Torre et al. (2006) behaviorist orientation is teacher oriented in that the instructor is manipulating the environment and presentation of information in order to achieve an observable behavior. The instructor must utilize reinforcement to achieve this goal. Benefits derived from this approach can be measured by assessing the correct observable behaviors exhibited by the class. “The behaviorist learning orientation is particularly useful for the development of competencies and for demonstrating technical or psychomotor skills. This learning theory is most advantageous when a change in behavior is the desired outcome of an educational intervention” (Torre et al., 2006, p. 903). Teachers can take advantage of this approach when the goal is to teach students to perform technical skills. Cognitivist orientation is to assist the learner in learning how to learn. Torre et al. clarified (2006), The locus of learning in the cognitivist orientation is the learners’ internal environment and cognitive structures. In this framework, the learner uses cognitive tools, such as insight, information processing, perceptions, and memory, to facilitate learning by assigning meaning to events. (p. 904) Learners are guided into making ‘concept maps’. These maps eventually are used by the students to develop correlations of ideas, thereby assisting the student in learning the information themselves. This reflective learning process can be applied throughout the entire education process. Torre et al. (2006) explained that humanist orientation truly attempts to have an individual reach their full potential. Essentially the teacher encourages the learner to 25 achieve their full potential, harnessing the learners’ need for self-fulfillment. Humanist orientation is personal in development and results in greater autonomous individuality. “Within the humanist framework, learning is viewed as a personal act necessary to achieve the learner’s full potential. The goal of this approach is for the learner to become autonomous and self-directed” (Torre et al., 2006, p. 905). Social learning orientation, according to Torre et al. (2006), requires learners to interact within a structured social environment. Components would include interaction for emulation as well as opportunity to perform rehearsal for solidifying concepts. “Observation and modeling are key characteristics of social learning orientation. Within context of the social learning theory, learners assimilate new information and assume new roles that require role modeling, behavioral rehearsal, and attending to observed behaviors” (Torre et al., 2006, p. 906). Application of this strategy in its entirety may not be efficient in the training of midlevel practitioners due to the need for time required for behavioral rehearsal and potential scarcity of appropriate observed behaviors. Constructivist orientation looks into a learner’s experience for educational purpose. A reflective process occurs in processing events that lead to a particular conclusion. Benefits include a strict attention to detail in order to perform critical reflection on proposed conclusions. This strategy is fairly new in the sciences of pedagogy as reported by Torre et al. (2006). The authors of this article do not acknowledge any negative aspects of this strategy. Concerns should be discussed about potential pitfalls. The learner that does not travel down the correct path for a conclusion could easily be learning the wrong information, and in worse cases the learner could be 26 building the wrong framework for solving problems later on. These limitations indicate that this specific strategy may have room for improvement. Creating a curriculum using concepts from the different orientations can assist in developing a hybrid strategy specific to an audience. Clinical curriculum requires an even more specialized point of focus, according to Essary, Berry-Lloyd, and Morgan (2003). Clinical rotations assist students in real world environments with added benefit of a specified resource. “These clinical rotations are critical building blocks in the student’s preparation as a health care provider, because they require the student to integrate didactic and clinical skills and acquire the confidence needed to function effectively in the clinical setting” (Essary et al., 2003, p. 78). Didactic education and clinical education have certain commonalities. Both will require active student participation and involved instructors for optimal effect. There are also varying degrees of didactic information and clinical involvement necessary. Such importance is placed on experience that clinical curriculum must be implemented with the best resources. This article does not provide a qualitative or quantitative analysis of past interventions. Positive aspects of this article are the consistencies with common themes noted throughout this literature review including; adequate orientation, an accurate syllabus, and adaptability. The research provided by Essary et al. (2003) offers sound advice for curriculum development. Essary et al. suggests, “The curriculum must be flexible, allowing for variation in experience and clinical acumen” (p. 81). Curriculum developed for the clinical experience is an exercise of application of information received from a variety of resources. These resources include previous 27 readings, lectures, and possible electronic sources. Eventually the resources will assist the learner. The learner then must apply all the tools of education into one more step, the clinical experience. “In the clinical portion of the PA curriculum, students are required to integrate and synthesize didactic and clinical information to formulate a differential diagnosis and management plan” (Essary et al., 2003, p. 80). According to Collins (2004), audience understanding must be considered while developing a curriculum. Principles of adult learning must be appreciated and applied to be effective. Although adult education is the basis of health care curricula there can be some commonalities in multiple strategies. Collins (2004) reiterates, “The adult education literature supports the idea that teaching adults should be approached in a different way than teaching children and adolescents (preadults). Many aspects of effective teaching apply to all age groups” (p. 1483). Collins’ (2004) article tends to be a well referenced document with several resources utilized per the listed references. Meta-analysis design was performed for many of the concepts discussed. Limitations include applicability of the material. The material is primarily intended for individualization with several common themes that can meet the needs of the entire class. This is effective for direct clinical instruction and meets the needs for development of a global curriculum intended for an entire class, more specifically, a class of adult learners providing health care. More prominent (and useful) ideals introduced need to come with the understanding that adult learners need an end point. Adult learners need an end-point. Collins (2004) explained, “Adults are goal-oriented. They like to know how the educational activity will help them reach their goals” (p. 1486). 28 Students encouraged to learn on their own will eventually gain the lifelong ability to perform self assessment as suggested by Ragan (2003). This self assessment will lead to self awareness and eventually lead the student to continued learning. A curriculum incorporating the concept of self assessment skills will allow for this process to occur at an academic level. Educators have traditionally desired for this phenomenon to occur. How does this phenomenon become reality? Ragan (2003) proposed, “As the paradigm in medical education shifts toward placing a greater responsibility on students to manage their own learning, so too does the need to strengthen the skills associated with successful outcomes” (p. 50). Giving greater responsibility leads to a greater sense of accountability. Accountability will require that the learner puts greater effort into their own future and learning process. This trait of assessment should be formed early in the training process. Ragan (2003) elucidates, “Assessment must be established as integral and essential for self-evaluation. Setting the tone for the importance of evaluation should be established from the onset of the program” (p. 51). Ragan’s (2003) research is a qualitative approach to analyze the appropriateness of self assessment proficiencies in curriculum. While critiquing Ragan’s (2003) research, one can note that there are limited references, however, the references are impressive thereby giving credibility to her discussion. Ragan’s (2003) proposals should be included in the majority of educational curriculum to enhance lifelong learning. Ragan’s (2003) proposals are imperative to any curriculum. More importantly the proposals are vital for health care professionals to incorporate during their career. Educators must learn to incorporate these concepts into curriculum. Ragan (2003) 29 considers, “As self-assessment and evaluation skills become increasingly important for lifelong learning of the graduate PA, so too has the need to teach these skills” (p. 52). Curriculum development has a responsibility not only to teach information necessary to pass licensing exams, but to also teach the learner the responsibility to provide health care for life. A health care curriculum has a responsibility to not only teach active intervention, but to also encourage prevention. Prevention is a major part of providing effective healthcare that the concept should be a building block of any curriculum. More importantly, in an environment riddled with infectious disease concerns, prevention needs to be an even greater factor in health care provisions. As discussed in the introduction, infectious disease is one of the greatest needs for improvement in the care provided to inmates. There is reason for concern that more emphasis needs to be placed on prevention in curriculum. Cawley (2005) explained, “Yet, in most clinical health professions educational programs, no structured, comprehensive, curriculum integrating the concepts of preventive medicine- more appropriately defined as clinical prevention and population health-exists” (p. 89). Cawley’s (2005) research and proposal was the result of combined efforts from seven clinical disciplines. These seven disciplines together are the driving force of the Healthy People Curriculum Task Force. Significant organizations include: American Association of College of Nursing, National Organization for Nurse Practitioner Faculties, and Association of Physician Assistant Programs. Analysis of Cawley’s (2005) work shows a thorough qualitative focus on past and present preventative strategies employed. The article is well written with sufficient (and 30 impressive) references. The limitations identified were few. One could suggest that the framework may not be easily applied to every level of education. For the purpose of curriculum development at the UCD Family Nurse Practitioner/Physician Assistant program this limitation is not significant. Implementation of preventative medicine requires a focused assessment of the environment (Cawley, 2005). The proposal suggested by the Healthy People Curriculum Task Force has three major components (Cawley, 2005): evidence base for practice, clinical preventive services-health promotion, and health systems/health policy. Key elements for implementing evidence based practice are identifying epidemiology, literature evaluation, costs, and determinants of health. These elements provide the basis of need. The second component (clinical preventive services-health promotion) directly addresses specific needs (Cawley, 2005, p. 93) (Figure 2) 31 Figure 2. Clinical Preventive Services – Health Promotion 1. Screening -Approaches to testing and screening, eg, range of normal, sensitivity, specificity, predictive value, target population -Criteria for successful screening, eg, effectiveness, benefits and harms, cost, patient acceptance -Evidence-based recommendations 2. Counseling -Approaches to culturally appropriate behavioral change, eg, counseling skill training, motivation -Clinician-patient communication, eg, patient participation in decision making, informed consent, risk communication, advocacy -Criteria for successful counseling, eg, effectiveness, benefits and harms, cost, patient acceptance -Evidence-based recommendations 3. Immunization -Approaches to vaccination, eg, live vs. dead vaccine, pre- vs. postexposure, boosters, target population, population-based immunity -Criteria for successful immunization, eg, effectiveness, benefits and harms, cost, patient acceptance -Evidence-based recommendations 4. Chemoprevention -Approaches to chemoprevention, eg, pre- vs. post-exposure, time-limited vs. long-term -Criteria for successful chemoprevention, eg, effectiveness, benefits and harms, cost, patient acceptance -Evidence-based recommendations The third component (health systems and health policy) requires that the institution assess the resources available. These concepts assist in developing the preventative portion of curriculum development. The recommendations provide building blocks, but also allow for variation dependent upon environmental factors. Significant improvement in public health could be positively affected if preventative strategies are implemented in any health care curriculum. The current proposal from the Healthy People Curriculum Task Force is a guideline that can be 32 utilized. This guideline does not need to be precisely duplicated. Cawley (2005) stated, “The aim is to provide general recommendations and identify content areas that may require greater emphasis than has traditionally been the case” (p. 90). Implementing preventative approaches has always been associated as a more positive and productive approach when compared to utilizing curative measures. Peer education programs can also be investigated for use in teaching strategies in curriculum development. Dubik-Unruh (1999) suggested that utilizing inmates to teach other inmates can be extremely effective. Teaching students to effectively communicate with inmates in order to assist inmates to teach other inmates would be another avenue for applying preventative medicine. Dubik-Unruh’s (1999) proposal is a qualitative assessment with the intent of encouraging instructors to prepare students for taking on a teaching role. This study is well written, but has several limitations. There are a moderate amount of references which tend to be utilized for in acknowledging a need, and not necessarily previously successful implementations. Implementation of this strategy may take a great deal of teaching time to assess students’ abilities. Utilization of prisoners would be an effective strategy. Dubik-Unruh (1999) proposed, “In addition, informed prisoners influence their prison communities through discussions with cell mates, impromptu classes in the prison yard, and conversations at meals” (p. 54). Essentially the proposal takes advantage of a simple thought- that prisoners can be educated to educate other prisoners. Assessing the needs and then implementing different avenues would be the most useful strategy. Using other inmates to teach would offer a much more familiar style. According to Dubik-Unruh (1999), “Prisoners want to learn- this has been 33 demonstrated repeatedly by their involvement in quality HIV education programs across the United States” (p. 54). This strategy would be useful, but does require a lengthy rotation and significant investments from instructors to assist students in implementing this curriculum. Summary Outcomes of current curricula in several programs have been noted. There are pitfalls that the proposed curriculum for this project hopes to avoid, such as a lack of preparation. A literature review of current curricula points to inadequate preparation being a major cause of concern. Several promising articles were examined that analyzed current programs. While many students are relatively new in the field of health care, many inmates are practiced in the art of manipulation for years. Students not prepared for this type of interaction may be at risk for misdiagnosis as well as harm to themselves and those around them. Inmate manipulation acts as a deterrent to the adequate care of inmates as well as creating bias in the care of future inmates. Students may become jaded and lose their initial drive to provide health care. Inadequate preparation and follow up in the clinical setting may have serious repercussions. Implementation of the UC Davis curriculum will require a hybrid of concepts and theories in order to cater to the needs of the specific target groups. Once completed, reevaluation for further improvements will need to be conducted on a regular basis. Health care and the prison system are both extremely dynamic and the curriculum must be able to reflect that trait. This shared quality means that the curriculum must be able to adapt to meet the ever-changing needs of teachers, inmates, and students. 34 Chapter 3 THEORETICAL FRAMEWORK Introduction The framework for the developed curriculum is firmly based in the theory of nursing that was authored by Madeleine Leininger, the theory of culture care. Prison society has individual characteristics different from mainstream society classifying the world of inmates into another culture. The impetus for developing the curriculum stems from the realization that the care of the inmate within the correctional facility setting is essentially caring for an individual of a subculture that is physically isolated from the main population’s culture. The physical barriers create a subculture that thrives on a mentality different from the general populace, and also creates situations where the care rendered is complicated due to concerns of security, safety, manipulation, and learning ability. These unique characteristics create the need for healthcare professionals to be capable of working comfortably and safely within the isolated environment. Without treating the incarcerated population as a separate entity of healthcare, appropriate intervention cannot occur. Without appropriate intervention, deficiencies will crossover into the general population. “Improved medical care and prevention services for incarcerated populations benefits communities by reducing disease transmission and medical costs” (Weinbaum, Sabin, & Santibanez, 2005, p. 45). In order to treat the subculture effectively, five of Dr. Leininger’s 13 assumptions can be applied to the creation of a specific curriculum. 35 Five Major Theory Assumptions Within Dr. Leininger’s theory of culture care, there are thirteen major assumptions or definitions upon which the theory is constructed (McFarland, 2006). While all thirteen of these major assumptions are beneficial, the close analysis of five assumptions prepares the foundation for the developed curriculum. The first major assumption within the theory of culture care is the assumption that “Care is the essence of nursing and a distinct, dominant, central, and unifying focus” (McFarland, 2006, p.481). The art of caring is the core of an effective interaction between the provider and the patient. Genuine empathic care conveys the sense of being and belonging to the patient and validates their feelings and concerns without interjecting the provider’s feelings or opinions. The care provided is enhanced parallel to the provider’s increased awareness and understanding of the patient’s holistic situation. It is thereby essential for the provider to diligently seek to understand the patient’s background and current position. The next assumption to be analyzed is the assertion that “Transcultural nursing is a humanistic and scientific care discipline and profession with the central purpose to serve individuals, groups, communities, societies, and institutions” (McFarland, 2006, p. 481). In other words, transcultural nursing uses both a humanistic and scientific approach that is tailored to the target culture’s individual, subgroups, communities, or institutions. In a practical sense, within the correctional facility, the individual is the inmate within the state or federal prison system. The inmate may belong to a subgroup such as a specific gang, transgender group, age classification, or medical situation. These groups exist 36 within the larger community of collective inmates within a specific correctional facility. The larger community or populace of a facility also shares a commonality with other inmates within the entire state’s or federal systems. Transcultural care can be formulated for the broad groupings or can be focused down to smaller subgroups or to specific individuals. The third major assumption to be discussed is the assumption that “Culture care values, beliefs, and practices are influenced by and tend to be embedded in the worldview, language, philosophy, religion (and spirituality), kinship, social, political, legal, educational, economic, technological, ethnohistorical, and environmental context of cultures” (McFarland, 2006, p. 481). This assumption would become more practical on an increasingly narrowed focus of care as would be provided to specific subgroups. The fact that inmates are heavily isolated does not necessarily diminish any of the categories mentioned above as their isolation often forces them to make alliances and a societal system in which to subsist. The more understanding a provider has of the nine contexts above as pertaining to a certain subgroup, the more culturally sensitive the care provided, as well as a more effective interaction. Understanding the culture and the motivating factors upon which the individual or subgroup operates allows the caregiver to anticipate care and education that may be needed to improve the situation of the target group or individual. The fourth major assumption to be analyzed within the theory of culture care is the assumption that “Culturally congruent and beneficial nursing care can occur only when care values, expressions, or patterns are known and used explicitly for appropriate, 37 safe, and meaningful care” (McFarland, 2006, p.481). Dr. Leininger’s fourth assumption indicates a need to delve within the subject’s understanding of care. Once established, the practitioner can seek out the subject’s values and expressions in an attempt to understand specific situations. This maximizes the provider and patient interaction which will lead to more effective energy expended in improving the situation of the patient. Eventually this process allows the provider to assess the subject’s level of education and core beliefs to best formulate a plan of care to be used in the future. The fifth and final major assumption to be examined from Dr. Leininger’s theory states, “Cultural conflicts, cultural impositions practices, cultural stresses, and cultural pain reflect the lack of cultural care knowledge to provide culturally congruent, responsible, safe, and sensitive care” (McFarland, 2006, p. 481). The understanding of this assumption is essential for the provider as this may very well dictate the outcomes of the patient and provider interaction. Application of this assumption is especially critical within the correctional facility due to the human tendency to formulate opinions and stereotypes and then impose them upon someone from a different cultural background. Many providers may enter into the correctional facility healthcare system with preconceived ideas and prejudices that can directly hinder the care they wish to provide. The answer to the naturally occurring cultural conflicts and impositions is for the provider to enter the healthcare system with an open mind toward all patients they encounter and to take the necessary time to learn the culture that the specific individual or subgroup represents. Jacques (2004) explains, “Students must first learn about crosscultural and ethnic barriers to health care and their adverse impact on patient care”. 38 Without the due diligence to learn about the cultural beliefs of the individual or subgroup the provider is allowing a major barrier to be left in place that restricts the quality and the outcomes of the care rendered. Summary The presented theory and several of its’ major assumptions are imperative for the provider to understand that care is the essence of the nursing profession. To provide effective care, the provider must be knowledgeable of the recipient of that care. Dr. Leininger’s assumptions are imperative in a system that has been identified with strong deficiencies. “Inherent within the prison system are inconsistencies in the availability and approach of the health care offered” (Evans, 1999, p.1326). This knowledge must include not only the scientific medical components of disease states and the necessary treatments or practices, but also an extensive knowledge of the patient in humanistic terms. Part of the humanistic knowledge that should be acquired is the understanding of the cultural influences that may be embedded and therefore heavily dictate the patient response to the scientific approaches of quality care. It is when the provider is knowledgeable of the patient’s culture, values, and beliefs, and can capably balance or compromise the humanistic aspects with the scientific care that might be indicated, that the apex of quality care is achieved. 39 Chapter 4 PROJECT OVERVIEW Intent of project This project’s intent is to provide a clinical curriculum to aid the midlevel provider, specifically nurse-practitioner and physician-assistant students, in the clinical setting of a correctional facility and the accompanying inmate subculture. The developed curriculum is intended to guide the students’ clinical focus by highlighting pertinent information. With the assumption that the correctional facility setting is different than most other clinical settings, this curriculum wishes to engage the students in thought about the cultures and subcultures that can be found within the setting and to consider how that affects the care that is provided. This curriculum also looks at how the setting tends to dictate the medical focus of care, and how that medical focus is much different from the general populace. Progression of the Project The idea for this project was conceived when one of the authors (who had also participated in a correctional facility clinical rotation as a student) was approached by a UCD educator and a correctional facility clinical preceptor at the California Medical Facility, Vacaville with the questions of how to improve a currently implemented clinical rotation. At that discussion, the suggestion of implementing a formal, specific correctional facility curriculum was voiced. The projected cost of the endeavor was reviewed and a budget set forth (Appendix A). It was decided by the authors to pursue this suggestion and to formulate a curriculum with the intent as stated above. Current 40 available literature appropriate for the topic was reviewed and critiqued in an endeavor to identify recurring themes and also areas of necessary improvement within similar clinical programs. Students from the UCD Family Nurse Practitioner/Physician Assistant Program who had participated in the corrections facility clinical experience at Vacaville were surveyed to assess the needs of a formal curriculum for that setting, and what concerns should be addressed within that curriculum. Each student was given a ‘Consent for Participation’ form (Appendix B) and a questionnaire (Appendix C). Information obtained from the literature review and the student surveys contributed to the formulation of the curriculum, most specifically to the formation of the coursework objectives. A curriculum template was obtained from the faculty of UCD, Family Nurse Practitioner/Physician Assistant Program. This template was utilized to formulate the actual structure of the syllabus. Upon consultation with the project advisor, it was decided to formulate the curriculum specifically for the UCD Family Nurse Practitioner/Physician Assistant Program to be implemented in their clinical rotation at the California Medical Facility, Vacaville. Pertinent texts that were evaluated for literature review were incorporated into the syllabus as required reading to provide a background for the student prior to actually participating in the clinical rotation. The curriculum was then structured as a stand-alone resource that could be directly implemented in the proper setting without the need for additional educational tools. With that thought in mind, it is intended that this curriculum would be used to guide a clinical rotation rather than be utilized as didactic curriculum. 41 Methodology of Student Sampling The methodology of obtaining student input for the curriculum development incorporated phenomenological inquiry. “Phenomenonology as a research method is a rigorous, critical, systematic investigation of phenomena” (Streubert-Speziale & Carpenter, 2007, p.81). The phenomenon of interest was whether students in the UCD, Family Nurse Practitioner/Physician Assistant Program were adequately prepared to participate in a clinical rotation through the challenging setting of the correctional facility, California Medical Facility, Vacaville. Around this phenomenon of interest, a survey was formed to be presented to a sampling of students who had voluntarily participated in the clinical rotation through the correctional facility. This survey can be reviewed in Appendix C. Survey Sample. The survey sample was taken from the class lists of students in the UCD, Family Nurse Practitioner/Physician Assistant Program who studied at the correctional facility between fall 2007 to spring 2009. Purposive sampling was used in obtaining the sample group. Purposive sampling is a method which “selects individuals for study participation based on their particular knowledge of a phenomenon for the purpose of sharing that knowledge” (Streubert-Speziale & Carpenter, 2007, p.94). Of the total students in the program during the above time, only the students who had participated in the voluntary clinical rotation at the correctional facility were contacted. The participating students were contacted either directly on campus or via email and were given the survey. Of 42 seventeen students contacted, a total of nine students responded by filling out the survey. The survey consisted of four questions specific to the rotation. Survey Results. The survey consisted of four questions regarding the student’s clinical experience. The first question asked the student to indicate what positive outcomes of the rotation contributed to the student’s development as a midlevel provider. The positive responses included: seeing facility staff as role models and educators, the exposure to new experiences that may not be available in the regular clinical settings, and the exposure to medical conditions and co-morbidities that are less frequently seen outside the correctional setting. The second question asked them to identify what negative outcomes the rotation had on their development as a midlevel provider. Of the nine responses, there were only two that indicated any type of negative aspect of the rotation. The negative outcomes were that limited pharmaceutical formularies made for narrowed critical thinking and medication selection, and also that there seemed to be some professional tension between some of the providers that one student felt conflicted with patient care. The third question asked the student participants what they would like to have modified in the rotation. This question garnered the most responses. Some of the suggested changes were to be able to spend more time in the hepatitis and urgent care clinics versus spending time in the primary care setting – some students favored more time in the specialty clinics versus others who favored the time in the primary setting. Other suggestions for change included having more information given prior to the 43 rotation regarding the prison system in general and the healthcare system within the prison, some wanted a longer orientation than the two day orientation provided by the corrections facility. Another suggestion was to review with the students prior to their rotation on how best to provide patient education for medical conditions as pertaining to the physical constraints placed upon the patients due to their incarceration. For example, students should be shown how to provide a narcotic pain killer for an inmate and prevent them from spitting the pill out and selling it later. The final question of the survey asked for the students to identify the medical conditions most often seen. This question was formulated to help identify higher prevalence of specific conditions and to ensure that the most prevalent conditions would be addressed in the developed curriculum. The medical conditions seen included: infectious diseases, HIV, sexually transmitted diseases, Hepatitis C, mental issues, Ear/Nose/Throat (ENT) complaints, chronic pain management, diarrhea, and dermatology complaints. Frequent treatments rendered were medication administration, incision and drainage of abscesses, psychiatric counseling, patient education, and referrals. Data Analysis. Data analysis of the raw data collected from the questionnaire included examining the common themes of the answers rendered. Rather than being quantified, the results of the data were sorted by question and a synopsis of the total sum of the answers to each individual question was then used to determine the focus areas for the development of the 44 curriculum. In this way, all data provided was utilized in guiding the actual development of the curriculum and bears a weight of significance within the curriculum. Discussion of Project Syllabus The syllabus was formulated along the general guidelines of the provided UCD Family Nurse Practitioner/Physician Assistant Program curriculum template. Approval was obtained from the UCD Family Nurse Practitioner/Physician Assistant Program to utilize the template. Each section of the curriculum template that was developed is further discussed below. Course Description. The Vacaville correctional facility rotation enables the student to develop clinical assessment and management skills focusing on the medical management of the inmate population. The goal for the student is to actively participate in medical care of the incarcerated patients. The proposed curriculum wishes to engage the student in thought about the cultures and subcultures that can be found within the setting and to consider how that affects the care that is provided. This is a PASS/FAIL clinical course. The student will be expected to complete a total of two weeks at the California Medical Facility, Vacaville. Teaching Methodology. The student will gain knowledge and understanding through direct clinical experience in the California Medical Facility, Vacaville, where the student can directly participate in patient assessment and management. Utilizing the recommended reading 45 resources and through written summarization of the clinical rotation, it is the student’s responsibility as an adult learner to demonstrate an understanding and completion of the course objectives. The student must achieve the course prerequisites prior to starting this coursework, and must follow this course’s requirements. Prerequisites for the Course. Prerequisites for the course are similar to concurrent courses that the student would be taking in the University of California, Davis program. Prior to starting the correctional facility clinical rotation, the student must have completed all of the didactic and clinical requirements of the first year of the FNP/PA Program. There must also be a memorandum of understanding (MOU) between the student, the preceptor, and UCD authorizing the student to participate in the clinical rotation. The student is unable to participate in the clinical rotation until they have received an MOU approval letter from the FNP/PA Program. The FNP/PA Program will contact the California Medical Facility, Vacaville regarding the student’s proposed clinical rotation as California Medical Facility, Vacaville must complete a background check on the student prior to approval. Course Requirements. The course requires that the student completes two weeks of clinical experience and is tracked by hours logged, the number of patients seen, and the amount of minimum clinical requirements that have been met. The rotation also requires that the student give his or her preceptor, and any other clinician they work with, a brief description of their current training level and their past clinical experiences. The preceptor and student should discuss the student’s rotation objectives for clear understanding by both parties. 46 Another of the course requirements is for the student to complete two written assignments: a summary of objectives and a summary of a patient care conference. The final requirement is for the student to keep proper records during their clinical rotation. The student is to retain any patient visit documentation that is not entered in the medical chart. Part of the student records includes the summary of objectives in which the student discusses which objectives they have met each day. Evaluations completed at the end of the rotation and the student log of patient contact and minimum clinical requirements are also part of the student’s record of the rotation. Expectation of the Student. During the rotation, the student is expected to participate as an active member in clinical assessment and management, and discuss patient progress for those patients to which he or she is assigned. The student is expected to be able to discuss resources and texts and independently abstract information from references to assist in the care of the inmate. The student must actively assume responsibility for his or her learning in the correctional facility. The student is expected to demonstrate knowledge of the pathophysiology, risk factors, complications, management, and patient education appropriate to medical conditions seen during the rotation. Objectives for the Correctional Facility Rotation. At the conclusion of the correctional facility experiences the student should be able to correctly obtain and record all the information needed for a complete history and physical exam. The student must then be able to use the information gained from the history and physical to be able to order (and interpret) the proper lab-work, diagnostic 47 tests, and treatments. During this gathering of information, the student should be able to recognize when a patient needs a higher level of care. During the clinical rotation, it is expected that the student participate in providing basic medical and surgical procedures appropriate for the care of the inmate. The student should also show familiarity with the correctional facility and be able to correctly order the services of ancillary departments and other resources within the facility. The student is expected to demonstrate understanding of medical conditions as pertaining to fluids, electrolytes, volume replacement, signs of shock, pain management, pharmacological therapy, various systembased infections and diseases, nosocomial infections, legal considerations, patient records and orders, and patient education. The student must then show a proficiency in using his or her understanding of medical conditions in implementation of treatments for the patients. The student are also expected to observe, and possibly participate in, a patient plan of care conference and then be able to submit a written explanation of that conference at the end of the rotation. Evaluation Criteria. The student will be held to specific criteria and documentation will be in the same format that the student has already utilized in previous University of California, Davis courses. Information must be submitted to the correctional facility rotation IOR within 30 days of completion of the rotation. All forms are found in the “Forms and Samples” section. The student is expected to submit his or her paperwork with a 3-ring binder or a large clamp. 48 Two evaluation forms are included within the syllabus. These include the form for the preceptor’s evaluation of the student. This form should be given to the preceptor and to one other clinician that the student worked with. There is also a form for the student’s evaluation of the preceptor and should include the second clinician as well. All of these forms must be turned in at the end of the rotation as described in the rotation checklist. Grading. Grades are awarded as a PASS/FAIL completion and based upon the IOR’s determination. The IOR will base his or her grading upon evaluations by attending physicians, residents, clinicians, and the IOR’s own interactions. Evaluation by preceptors will make up 40% of the grade. The summary of objectives for the Correctional Facility Rotation will account for 60% of the grade. The student must score 70% or higher in order to pass. Rotation Description. The student is expected to attend all FNP/PA Program classes. Rotations must be scheduled around classes. Correctional Facility rotations will be scheduled by the Instructor of Record. The student starting the rotation will usually overlap with the current students on the Correctional Facility rotation from one day to one week. This allows for orientation. All details of these rotations, including MOUs etc., need to be arranged by the individual student and approved by the advisor and the correctional facility Instructor of Record. A sample letter designed to inform medical staff of the role requirements is included in the forms and samples section of the syllabus. 49 Correctional Facility Rotation Forms. This section includes a generic form that is presented by the student to a prospective preceptor to explain the role of the preceptor, the student, and the responsibility of the University. This states that the preceptor must be approved by the University and an MOU must be on file before the student may work with the preceptor. This form also states that the student is never to be unsupervised. The contract between the University and the preceptor also extends the professional liability coverage of the University to the preceptor to ensure that the preceptor is protected should claims against the student arise. This form also discusses the specific objectives of the clinical rotation so that the preceptor is prepared to guide the student in these areas. In this section of the syllabus, there is a general information form explaining the role of the student and how the student is to be supervised in certain instances. This form also includes an IOR contact number should a problem arise between the preceptor and the student. Charting Examples. Charting examples include a History and Physical (H&P), a procedural note, and a sample prescription. These examples are provided as a template for the student and give prompting to ensure that comprehensive documentation takes place within the clinical setting. The student signs all documentation except for the prescriptions. All documents are co-signed by the preceptor, and only the preceptor signs the prescriptions. Corrections Facility Rotation Checklist. The checklist is a list of all the necessary components the student must turn in to the IOR at the end of the two week rotation. The required paperwork must be turned in 50 for grading and includes the PCR sheet, the MCR sheet, the student Summary of Objectives write-up, the student’s evaluation of the preceptor and one other clinician with whom the student may have worked. Evaluations of the student must be submitted by the preceptor and one other clinician. Patient Contact Record (PCR). The patient contact record must be an accurate record of the number of patients seen directly by the student during the length of the rotation. This does not include patient cases that the student merely discussed with the preceptor, but did not participate in direct care. This record must have a traceable identifier for each patient so that the student could obtain the specific patient’s chart should the IOR wish to audit the student’s documentation or should questions arise. Minimum Clinical Requirements (MCR). The minimum clinical requirements must be met to successfully complete this rotation. Exceptions may be allowed by the IOR on an individual basis. The requirements are both diagnosis and interventions. These MCRs are based upon current need as identified in the literature critique. The MCRs include various mental health diagnoses, sexually transmitted infections, chronic medical conditions such as diabetes, congestive heart failure, pain management, episodic conditions such as upper respiratory infections and rashes, and also interventions such as I&Ds and suture placement. Several complete H&Ps are also required so as to ensure that the student address health care maintenance and chronic conditions within the confines of the correctional facility. Summary of Objectives. 51 The Summary of the Objectives is a listing of the course objectives as stated above. It is recommended that, at the end of each day within the clinical rotation, the student document what objectives were met that day. This encourages the student to keep close observation so as to meet all of the objectives by the end of the clinical rotation. At the end of the rotation, it is required for the student to complete a write-up of how they actually met each of the course objectives as outlined, or to explain why they were unable to meet a specific objective. This must be turned in to the IOR for a final grade. General Rotation Policy and Procedures. At the very end of the syllabus, there is an extensive section that includes the University of California, Davis, Medical Center policies and procedure for students who might come in contact with blood or other bodily fluids, or would have a needle-stick exposure. These policies discuss prevention, hygiene, immunizations, and treatment in the event of an actual exposure. These exposures must be reported to the proper personnel promptly so that the proper treatment can be administered in a timely fashion and the necessary documentation be completed. 52 Chapter 5 CONCLUSION Introduction Correctional facility health care is a specialty field requiring the most dynamic of professionals that are capable of working with a wide variety of patients. This project has discussed the purpose and significance of developing a correctional facility clinical curriculum and the significance of developing the curriculum to patients and health care. Most importantly, a strong need for a specific curriculum was reported and verified by previous students. An extensive literature review was performed explaining current practices and proposed strategies. These strategies were then systematically applied to Dr. Leininger’s theory of cultural care. After constructing specific thought processes, a curriculum was formed. The proposed project delves into concerns that were addressed in the introduction and tackles those concerns directly. Most of the concerns were addressed specifically by asking participants to incorporate specific disease processes and interventions into their patient assessments. Encouraging students to seek out specific diagnosis from the patient population should enhance the students’ knowledge base of current concerns involved in providing health care to this very unique population. Theoretically, the student is better prepared to work with inmates in an organized fashion with health care goals in mind. This fashion of teaching incorporates many aspects of successful teaching styles as discussed in the second chapter. 53 Disturbing points of interests, as identified in the introduction, were utilized as the basis for intervention. Commonalities associated with health care in the prison system were identified. Concerns that have become prevalent in the health care of inmates have included infectious disease with emphasis on hepatitis C, human immunodeficiency virus, and tuberculosis. Health care maintenance proved to be an area of concern. Behavioral health was also identified as a troublesome matter. Palliative care was recognized as an area in need of improvement. Provider well-being was also discussed in order to protect providers and to assist in alleviating fears. These issues were areas of concerns that stimulated specific portions of the proposed curriculum and allowed for guided objectives to be put into practice. Evaluation This project has not been implemented to date. Projects without implementation have little true resources for complete evaluation. The evaluations cannot be directly measured by implementation outcome analysis. The evaluation of this project is based upon critiques from experts in the field. These experts bring a wealth of experience as well as training. In order to evaluate the proposed project, several individuals were contacted. These individuals were selected due to their individual knowledge bases of teaching, curriculum development, and experience with the population of interest. All of the evaluators are practicing health care providers and participate in the education of health care providers. The proposed syllabus was submitted to two instructors from the UCD Family Nurse Practitioner/Physician Assistant program. These individuals were Duane DeAmicis 54 (F.N.P.-C, M.S.N., and Faculty instructor) and Shelly Stewart (F.N.P.-C, M.S.N., and Associate Director of the Family Nurse Practitioner/Physician Assistant program). California State University, Sacramento Nursing Division Chair Ann D. Stoltz (PhD., R.N.), was also utilized as a reader for the project. Modesto Junior College Nursing Division Director, Lisa Riggs (M.S.N., R.N.) and Assistant Director Terry Ward (M.S.N., R.N.) were also approached for their expertise in developing nursing curriculum. The final individual selected for evaluation, was selected for her long history and good standing with the UCD Family Nurse Practitioner/Physician Assistant program. Agnes Warhover (PA-C) is a current employee of the California Medical Facility, Vacaville institution and has worked with a variety of health care students. The evaluations proved to be invaluable. Several suggestions were investigated and many changes were made. These changes were made only after significant consideration was given for potential negative repercussions. Changes that did not seem to have merit based upon previous research, or suggestions that conflicted with previously documented data were not implemented. Limitations Limitations for the proposed project are primarily due to the specificity of the subject. Literature resources are limited for providing care in the correctional facilities. Hundreds of textbooks exist on medicine, psychiatry, surgery, and assessment. Only one book exists pertaining to correctional medicine. Clinical Practice in Correctional Medicine by Puisis is currently the only known textbook and is currently in its second edition as of 2006. Curriculums in the past have not relied heavily on this resource. 55 Educational facilities have most likely shied away from this resource due to the cost. The cost is currently listed at 600 to 1,000 dollars by multiple search engines including Amazon, Borders, and Barnes & Noble. The disadvantage is that this is the only textbook that curriculums can rely on heavily for training purposes. Resources for the curriculum are not the only area of concern. The curriculum can only be used with certain populations. Strict editing must occur to adapt the curriculum to other environments. Female prisons have existing gender specific concerns that this syllabus does not address. Considering the difficulty in maintaining the routine medical monitoring in the general public the healthcare practitioner must be aware of concerns regarding routine healthcare in the correctional facility. A qualitative study that analyzed the routine healthcare of women in the California prison system explored concerns focused on papanicolaou testing and treatment (Magee, Hult, Turalba, & McMillan, 2005). Magee et al. (2005) explained, “The women spoke of inconsistencies in the process to obtain Pap tests, the frequency of lost results, the lack of appropriate follow-up care, and significant delays throughout the spectrum of care” (p. 1716). Essentially the article pointed out multiple deficiencies in the routine monitoring of cervical cancer. Concerns included inadequate screening, lost results, inefficient follow-up, and poor exam techniques. In a text by Blitz, Wolff, and Paap (2006) discussion centers on the findings and conclusions of a study regarding women’s behavioral health needs in prison. The study further illustrates a limitation of gender specific curriculum. “This study examined whether women with behavioral health needs are more likely to receive treatment for 56 these problems in prison or in the community and to what extent prison disrupts or establishes involvement in treatment for these women” (Blitz et al., 2006, para. 1). The authors of this study did a large sample population survey of women in prison, seeking the attitudes of the inmates in regards to health care, access, and usage of said health care. The basic conclusion of this study was that these women actually had greater access to behavioral health care while in prison than before incarceration. This study also showed that if these women would have had better community access to behavioral health care, they may have averted incarceration. Direct limitations must be analyzed with caution. The limitations discussed so far are basic and easily recognizable. Further discussion of the project would be theoretical. Teaching styles utilized, concerns stressed, and framework implemented can all be identified as points of limitations based upon personal preference. The curriculum provides a framework to work within and may require further changes as potentially new limitations are identified. Literature Review Impact Data analysis performed during the literature review provided the strategies for curriculum development. The need had been established for an intervention. A plan needed to be developed to cure the shortcomings. The literature review provided information on several currently existing similar programs. The literature surrounding these programs indicated positive results for similar curriculums. Looking into the effectiveness of these programs provided hopeful scenarios. Looking into the limitations 57 of the programs (as well as the articles) granted the opportunity to identify room for improvement. Strategies implemented by the National Commission on Correctional Health Care (NCCHC), as identified by Hale et al. (2008), were extremely beneficial in identifying a successful intervention. Principals from the NCCHC were the initial guiding light behind the proposed curriculum. Further analysis of current literature provided similar approaches to the identified problems. While other articles were examined and found to be similar, these similarities provided greater confidence that the proposal would be successful. Variations identified were assessed for their appropriateness and their optimal benefits to the current curriculum. Teaching strategies have historically been developed to assist educators in relaying information to specific student populations. Philosophies are based upon ability of students and type of material. The proposed project utilized the five different learning theories recommended by Torre et al. (2006). These five theories provided a structured learning basis for information to be presented effectively in the curriculum. Components of the learning theories were seen throughout the literature review and tended to be quite effective in encouraging life long learning habits. Implications for Nursing Nursing can benefit from implementation of the proposed project. The extent at which nursing can benefit will be based upon two factors: students and inmates. Students will need to employ the objectives of the curriculum. Inmates will be directly affected by the implementation of the project. Assessment of both populations will then need to be 58 performed in order to analyze the implications for further development. Implications are centered on the notion that future generations of health care providers will feel a need to provide care to this unique population. Future generations will feel the need to improve care. Future generations will adapt portions of the syllabus to other environments of care outside the currently proposed population. Summary Nursing as a whole has been considered an extremely compassionate profession. Society has had time-honored respect for nursing. History has provided ideal role models that include Florence Nightingale, Dorothea Orem, and Madeleine Leininger (to name only a few). While nursing has evolved to meet the ever dynamic needs of healthcare, the fundamentals of nursing still exist- caring for the ill. Time has provided multiple avenues for providing care. Walking into several different floors of any given hospital an individual can see more wires and tubes than under the hood of a car. Under all of the spaghetti-like bio-medical devices lies a person suffering from an illness. Nursing does not differentiate, and should never discriminate, about societies’ sick. Focus of health care has shifted to medical and science advancement. Patient intervention centers on physiological well-being. Medicines designed to manipulate the most out of a patient’s Krebs’ cycle, are consistently being developed. Patients are a conglomerate of complicated processes at the micro and macro levels. These processes are the identity of individuals. The nursing implications of this project go beyond the mechanical and medical aspect of health care; the implications look at a special population that has been 59 identified as underserved. The project looks to provide quality health care to the ever growing society and to assist those in performing those duties. 60 APPENDIX A Budget Budget Items Paper Cost per Item 500 pages @ $5 Total Cost $20.00 Print cartridge 3 cartridges @ $50 50.00 Postage Miscellaneous 50.00 Computer software APA software and update 50.00 Data entry Provided by researchers 0.00 Typist services Provided by researchers 0.00 Manuscript paper 250 pages X 3 copies Travel costs Gas, parking, food Communication costs: Provided by researchers Costs of presenting research Microfilming, packaging, etc. 70.00 300.00 Time off from work 0.00 100.00 3600.00 (Researchers to forgo scheduled work hours, resulting in a loss of income, Estimated total hours: 80 hrs @ $45/hr) Unexpected costs 200.00 Total $4440.00 61 APPENDIX B Consent of Participation California State University, Sacramento Consent of Participation in A Research Study Purpose Statement: The Purpose of this study is to assess the subjective levels of student satisfaction in regards to having utilized formal curriculum prior to the correctional facility clinical rotation. This study will include students who have participated in the curriculum and students who did not utilize the curriculum prior to their clinical rotation. This study will ask that each participant (regardless of using curriculum or not) complete a Likert scale questionnaire, taking approximately 20-25 minutes to complete. Risks or Identifiable discomforts: Minimal risks are expected to the participants of this study. The participants will be asked to complete a questionnaire. As such the risks would be minimal (i.e. paper cuts, etc.) Benefits to participants: Benefits include opportunity to influence the future education of midlevel practitioners in the correctional care facilities. Confidentiality: Participants’ identifications will be kept confidential. Signing this document entitles the researchers the use of your answers. Your names will not be utilized, only the answers provided. Returned correspondence will be accepted anonymously to ensure participant confidentiality. Participants returning correspondence with their names will have their correspondence shredded after the answers are collected to ensure confidentiality. 62 Contact information: Participants may contact the research team under the leadership of James Avery and Ken Bowman at (209) 823-8040 with any concerns including: pertinent questions, risks, rights, and any sustained injuries. Participants may also contact the Department of Nursing at California State University, Sacramento at (916) 278-3869 if there are any concerns pertaining to the research team members. Voluntary Participation: Participation is not mandatory and each participant reserves the right to discontinue the study at any given time. There is not a need to provide a reason or cause for leaving the study. Nor is the participant held to any penalties or loss of any identified benefits for leaving the study. Confidentiality will be maintained even for those individuals that leave the study. Your signature below indicates that you have read and understand this consent. You also agree to participate in the research as described in the consent. -----------------------------------Signature of Participant ----------------Date 63 APPENDIX C Study Questionnaire California State University, Sacramento Study Questionnaire Dear_________________________________ You are being contacted for your opinion in regard to a clinical rotation you participated in while in the UC Davis FNP/PA Program. The rotation in question is the clinical rotation through the California Medical Facility, Vacaville. We would like for you to share your experiences and opinion of the rotation with us. We are currently working on compiling data and organizing that information in accordance with the Master’s Project guidelines set forth by CSU, Sacramento. Be aware that the information you provide may be directly quoted, but you will remain anonymous within the Project. Our Project is to develop a formal Correctional Facility Rotation Curriculum to be utilized specifically by the UC Davis FNP/PA Program for future midlevel practitioner students. Your participation is appreciated. 1) Please indicate what positive outcomes the prison rotation had for your development as a midlevel provider: 2) Please indicate what negative outcomes the prison rotation had for your development as a midlevel provider: 64 3) What changes to the current rotation would you suggest or like to see implemented to make the rotation more informative and beneficial to a midlevel student: 4) What were the most common disease processes that you encountered (please list the 3 most common)? What were the most common treatments that you performed (please list 3)? Sincerely, James Avery, RN, BSN, PA-C Ken Bowman, RN, BSN, PA-C 65 APPENDIX D Syllabus CORRECTIONAL FACILITY ROTATION Syllabus Academic Year: Instructor of Record: Duane DeAmicis, FNP-C, MSN Year II – PA and FNP-MSN Track 66 TABLE OF CONTENTS Definition of Syllabus Terms…………………………………..………………………...68 Course Description……………………………………………...………………………..70 Teaching Methodology…………………………………………...……………………...70 Prerequisite for Course…………....……………………………………………..70 Course Requirements…………………………………...………………………..71 Expectation of the Student………………………………………………………...……..74 Objectives for the Correctional Facility Rotation…………………………………...…...74 Reading Assignments…………………………………………………………………….77 Evaluation Criteria……………………………………………………………………….78 Grading…………………………………………………………………………………..79 Rotation Description………………………………….………………………………….79 Correctional Facility Rotation Forms and Samples……………...………………………80 Corrections Facility Preceptor………………………………….………………..80 General Information Form……………………………………….………………86 Example of History and Physical……………………………….………………..87 Example of Procedural Note…………………………………….……………….89 Example of Prescription Writing………………………………………….……..90 Correctional Facility Rotation Checklist……………………………..……….....91 PCR Form………………………………………………………………….…….92 MCR Form……………………………………………………………………….95 Summary of Objectives…………………………………………………….…….96 67 Evaluation of Student by Preceptor………………………………………….…..99 Evaluation of Preceptor by Student……………………………………….……101 General Rotation Policy and Procedures, UCD Health System………………………..102 68 Definition of Syllabus Terms Minimal Clinical Requirements (MCR): Diagnosis or procedures that must be directly addressed by the student to complete the objectives outlined in the syllabus. Patient Contact Record (PCR): A list of patients with whom the student has had direct responsibility in some aspect of the patient’s care whether addressing diagnosis or interventions participated in. The patient must be listed with an identifier so that the student is able to review the medical records at a later date should the student be audited by faculty. Instructor of Record (IOR): The U.C.D. instructor who is responsible for the students within the clinical rotation. Memorandum of Understanding (MOU): The documentation that allows nonfaculty medical professionals to precept the student and clearly defines the roles and responsibilities of said preceptor, the student, and the University. Family Nurse Practitioner and Physician Assistant Program (FNP/PA Program): Direct reference and abbreviation of the U.C.D., Family Nurse Practitioner/Physician Assistant Program. History and Physical (H&P): An extensive medical exam that includes patient’s personal and familial medical history, social habits, medications, allergies, and includes a comprehensive physical exam. Incision and Drainage (I&D): Specific procedural intervention implemented for treatment of abscesses. 69 NPO: An abbreviation for “nothing by mouth”, a medical intervention used on occasion for certain labs, diagnostics, interventions, or in certain medical conditions. 70 I. COURSE DESCRIPTION The clinical correctional facility rotation enables students to develop clinical assessment and management skills focusing on the medical management of the inmate population. The goal for the student is to actively participate in medical care of the incarcerated patients. This is a PASS/FAIL clinical course. Students will be expected to complete a total of two weeks at the California Medical Facility, Vacaville. The correctional facility rotation may be credited only after completion of all Year I didactic and clinical requirements. II. TEACHING METHODOLOGY Students will gain knowledge and understanding through direct clinical experience in the California Medical Facility, Vacaville, where the student can directly participate in patient assessment and management of medical need. A. PREREQUISITES FOR COURSE 1. All Year I clinical preceptorship requirements (hours, Minimum Clinical Requirements [MCRs] and Year I Procedural MCRs) must be completed and signed off by the Year I Instructor of Record (IOR) for the 340 or 240A-C Clinical Preceptorship. 2. A Memorandum of Understanding (MOU) between the medical professional, student and U.C.D. must be approved before beginning the correctional facility rotation. 3. The MOU for any preceptor excluding volunteer clinical faculty will not be in 71 effect until an approval letter from the program is received by the student. The student may not work with any preceptor without an approved MOU, unless the preceptor has a U.C.D. Family Practice volunteer clinical faculty appointment. The student should check with the Student Affairs Office if there is a question regarding the need for an MOU. 4. The U.C.D. Family Nurse Practitioner/Physician Assistant (FNP/PA)Program office will notify the California Medical Facility, Vacaville of the student’s proposed correctional facility rotation. 5. California Medical Facility, Vacaville will perform a background check of the student prior to the student receiving security clearance for the clinical rotation. 6. The student should retain a copy of the approved MOU with this syllabus. The MOU will include the starting and ending dates for each rotation. Hours of correctional facility experience that are recorded and do not coincide with effective MOU dates will be disallowed, and disciplinary action may result. B. COURSE REQUIREMENTS 1. Clinical Hours a. The student will complete two weeks of experience participating in the diagnosis and treatment of patients on the Medical/Family Practice service. The clinical day may be longer than eight hours. b. Hours: Patient contact hours for the correctional facility rotation may be counted toward hours for 341 or 240D-F Clinical Preceptorship. c. Patient Count: Patients seen on the correctional facility rotation will 72 count toward the patient count for 341 or 240D-F Clinical Preceptorship. d. MCRs: Patients seen on the correctional facility rotation may be counted in the MCRs for 341 or 240D-F Clinical Preceptorship. 2. Orientation of the Attending Physician a. Students should discuss with the attending, and any other clinician on the medicine team who participate in the student’s education, their past work and clinical experience and briefly describe their current level in the FNP/PA Program. b. Students should provide to the attending, and any other clinician on the medicine team who participate in the student’s education, a copy of the correctional facility rotation objectives. 3. Written Assignments (to be submitted as a packet) a. The student will complete the summary of objectives for the correctional facility rotation, typed and submitted with the correctional facility packet. b. The student will complete one summary of a patient care conference (i.e. the diagnosis of patient discussed, difficulties w/ management of care, plan of care discussed). 4. Clinical Progress The completed correctional facility packet must be submitted to the IOR within 30 days of the completion of the rotation. Failure to submit the 73 packet within 30 days may result in failure of the correctional facility rotation. 5. Record Keeping a. All write-ups that are not recorded in the medical chart must be retained by the student. These write-ups may be audited. b. Complete the Summary of Objectives Correctional Facility Rotation. Briefly document how you have met the course objectives. It is advisable to review each day’s experience and make note of your progress toward achieving the course objectives. c. The student evaluation of preceptor, including the attending and one other clinician on the medicine team who participated in the student’s education, must be completed. A separate form for each preceptor must be submitted. d. The correctional facility preceptor’s evaluation of student - must be completed by the attending physician and any other clinician on the team who consistently teaches students. The form must signed by a preceptor with an MOU. When completed, the preceptor must return the evaluation form to the student who will submit it with the completed correctional facility rotation packet to the IOR. A separate form from each preceptor must be obtained. e. The correctional facility MCR sheet must be completed. f. Correctional facility patient contact record (PCR) sheet: This list should 74 contain patient name or identifying number for all patients for whom you wrote an admission H&P, procedure notes, progress notes, discharge planning, discharge summary, discharge orders, ordered tests, or obtained consent. Do not list patients on PCR sheet if you didn’t participate in their care, i.e., you only discussed the patients during rounds or conferences. III. EXPECTATIONS OF THE STUDENT During the rotation, the student is expected to: 1. Participate as an active member in clinical assessment and management, and discuss patient progress for those patients for whom he or she is assigned. 2. Discuss resources, texts, and independent abstract information from references used to assist in the care of the inmate. 3. Actively assume responsibility for his or her learning in the correctional facility. 4. Demonstrate knowledge of the pathophysiology, risk factors, complications, management, and patient education appropriate to medical conditions seen during the rotation. 5. Identify the Bloodborne Pathogen Exposure Control Plan in this facility. IV. OBJECTIVES FOR THE CORRECTIONAL FACILITY ROTATION At the conclusion of the correctional facility experiences the student will be able to: 75 1. Recognize when a patient needs higher levels of medical care. 2. Obtain and record an appropriate medical history. 3. Perform and record an appropriate physical exam. 4. Order, record, and interpret appropriate laboratory and diagnostic tests for assigned patients in collaboration with a preceptor. 5. Perform basic medical and surgical procedures appropriate for the diagnosis of the specific inmates (abscess I&D, laceration repair, medication injections, etc.). 6. Demonstrate familiarity with the correctional facility setting, departments (their functions), and ancillary resources. 7. Demonstrate knowledge of the following: a. Common fluid, electrolyte and related acid-base problems. b. Volume replacement as to type, amount and rate of replacement based on specific need or diagnosis. c. Patients presenting with signs of shock (hypovolemic, cardiogenic, septic, and neurogenic). d. Pain management of specific needs appropriate for inmates. e. Appropriate pharmacologic therapy of medications commonly used in the correctional facility setting. f. Complications including, but not limited to: fever, infections, thrombophlebitis, urinary retention, atelectasis, pneumonia, pulmonary embolus and other sequelae of extended bed rest. 76 g. Factors related to infection including: pathogenesis, nosocomial infection (e.g. Clostridium difficile, methicillin-resistant staphylococcus aureus [MRSA], central line infection). h. Legal considerations in reference to obtaining informed consent and permits in special circumstances. 8. Demonstrate proficiency with documentation on patient progress notes and with appropriate orders by writing progress notes on all assigned patients. 9. Participate in the management of patients, including patient education, in collaboration with a preceptor. 10. Participate in the appropriate management of: a. Fluid, electrolyte and acid-base problems. b. Patients presenting with signs of shock (hypovolemic, cardiogenic, septic, and neurogenic). c. Chronic pain during the length of incarceration. d. Pharmacologic therapy related to specific diagnosis. e. Problems arising from extended bed rest including, but not limited to: fever, infections, thrombophlebitis, urinary retention, atelectasis, pneumonia, pulmonary embolus, and skin breakdown. f. Factors related to infection including pathogenesis and antibiotic use. g. Patient nutritional status including prolonged NPO status, tube feedings and hyperalimentation (Hospice Inmates). 11. Demonstrate proficiency in: 77 a. Participating in the formulation of discontinuation plans. b. Providing accurate patient education regarding the disease process, plan of care and rationale for treatment. 12. Participation/Observation of Plan of Care Conference. V. READING ASSIGNMENTS The texts listed under recommended ‘Recommended are designed more specifically for the content. ‘Suggested’ texts have limited resource ability. A. Recommended: * Goldman, L. & Ausiello, D. (2004) Cecil Textbook of Medicine. 22nd ed. On-line. W.B. Saunders Co. * Clark, M. (2007) Community Health Nursing: Advocacy for Population Health.5th ed. * Puisis, M. (2006) Clinical Practice in Correctional Medicine. 2nd ed. Daily readings as appropriate based upon the diagnoses of the patients to which the student is assigned. Online resources available: ePoctrates Essential PDA Program 2010. Web site: http:/www2.epocrates.com/index.html B. Suggested Texts: Students are encouraged to review any literature recommended by other health care providers (see medical library at U.C.D.) or wherever the experience takes 78 place. Include utilization of MEDLINE or other Internet sources for more information. In addition, the following texts may be previewed before purchase, if the student chooses to buy additional text(s): * American Medical Student Association. Survival Manual: Guide to the Clinical Years. * Shubhada, N, et al (Ed.). The Washington Manual of Medical Therapeutics. * Gilbert, DN, Moellering, RC, Sande, MA. The Sanford Guide to Antimicrobial Therapy. VI. EVALUATION CRITERIA The following information must be submitted to the correctional facility rotation IOR within 30 days of completion of the rotation. All forms are found in the “Forms and Samples” section. Secure your paperwork with a 3-ring binder or a large clamp. Submit paperwork in the following order with the “Correctional Facility Packet Checklist” as the first document: 1. Correctional Facility PCR Sheet. 2. Correctional Facility MCR Sheet. 3. Summary of Objectives for Correctional Facility Rotation. 4. Student’s Evaluation of Attending and one other clinician who consistently participated in the teaching. 5. Correctional Facility Preceptor’s Evaluation of Student - The attending and one other clinician will be evaluating you. They will submit the 79 evaluations to the student who will include it in the correctional facility rotation completion packet to be submitted to the IOR. Evaluation by the facility preceptors accounts for 40% of the final grade. VII. GRADING PASS/FAIL based on review of experience by IOR and evaluations by attendings, residents, and clinicians. Evaluation by preceptors 40% Summary of Objectives for Correctional Facility Rotation 60% A total grade of 70% or higher is required to pass this course. PASS=70–100% FAIL=<70% COMPLETION OF THE CORRECTIONAL FACILITY ROTATION: The completed Correctional Facility packet must be submitted to the IOR within 30 days of the completion of the rotation. Failure to submit the packet within 30 days may result in failure of the Correctional Facility rotation. This failure may necessitate repeating the rotation as determined by the IOR. VIII. ROTATION DESCRIPTIONS Students are expected to attend all FNP/PA Program classes. Rotations must be 80 scheduled around classes. Correctional Facility rotations will be scheduled by the IOR. Students starting the rotation will usually overlap with the current students on the Correctional Facility rotation from one day to one week, providing time for orientation. All details of these rotations and documentation, including MOUs etc., need to be arranged by the individual student and approved by the advisor and the Correctional Facility IOR. A letter designed to inform medical staff of the role requirements is included in the forms and samples section of the syllabus. IX. CORRECTIONAL FACILITY ROTATION FORMS AND SAMPLES Dear Corrections Facility Preceptor: This letter provides details you will find helpful regarding the UC Davis Family Nurse Practitioner/Physician Assistant student’s role during the Correctional Facility Rotation proposed at the California Medical Facility, Vacaville. The University of California, Davis School of Medicine provides a two-year Family Nurse Practitioner/Physician Assistant Program through the Department of Family and Community Medicine. Students in this program are officially “special status” students in the School of Medicine and are trained clinically in their home communities by primary care preceptors. Clinical requirements include inpatient and ambulatory care settings. Preceptor must be approved by the University via a formal Memorandum of Understanding (MOU) agreement. The physician covered by the MOU is responsible for precepting the student. Students and preceptors with MOUs operating under these 81 guidelines are covered by the University malpractice policy. It is important to note that because these students function under strict supervision, potential liability situations are unlikely. In accordance with state law and sound practice, no student may be unsupervised. All actions by students must be reviewed by the supervising physician. Supervising physicians must observe all invasive procedures. Students may begin work in the Correctional Facility only with the advance notification of and prior approval by appropriate area Correctional Facility personnel. All medical records must be co-signed by the supervising physician, who shall insure at all times that the student is not acting autonomously. All orders must be signed by the supervising MD before orders can be carried out. This concept is familiar to most physicians in that it is based on the clerkship model of medical education. Students should be considered as students in the School of Medicine completing rotations with community preceptors. In most cases this obviates the need for timeconsuming meetings and extensive paperwork. It is a concept consistent with the Joint Commission and should not pose problems with accreditation or hospital licensure. As a part of the clinical portion of the FNP/PA Program, students work at the Correctional Facility with approved preceptors. Once a Memorandum of Understanding (MOU) is in effect, the licensed physician (whose name appears on the MOU) accepts an appointment as Preceptor (for the student named in the MOU) and as an Agent of the University for the purpose of providing supervision of the FNP/PA student during the correctional facility rotation. During the period of the correctional facility rotation, the 82 FNP/PA student shall be a continuing student at the University of California, Davis. The University provides professional liability coverage for students while students are providing care in approved clinical settings. The University of California, Davis is self insured. Duration of current coverage is indicated by the dates on the MOU. As an Agent of the University, professional liability coverage is extended to the Preceptor for claims arising out of the performance of duties described in the MOU, but only in proportion to and to the extent such liability, loss, expense, attorney’s fees, or claims for injury or damages are caused by or result from the negligent or intentional acts or omissions of the student while acting within the course and scope of the University’s sponsored teaching program. An integral part of the clinical program for students is learning how to function in the clinical setting. Ideally, students will function at approximately the same level as a third-year medical student clerk. The Correctional Facility rotation has the following objectives and at the conclusion of the correctional facility experience, students will be able to do the following: 1. Recognize when a patient needs higher levels of medical care. 2. Obtain and record an appropriate medical history. 3. Perform and record an appropriate physical exam. 4. Order, record and interpret appropriate laboratory and diagnostic tests. for assigned patients in collaboration with a preceptor. 5. Perform basic medical and surgical procedures appropriate for the diagnosis of the specific inmates (abscess I&D, laceration repair, 83 medication injections, etc.). 6. Demonstrate familiarity with the correctional facility setting, departments (their functions), and ancillary resources. 7. Demonstrate knowledge of the following: a. Common fluid, electrolyte and related acid-base problems. b. Volume replacement as to type, amount, and rate of replacement based on specific need or diagnosis. c. Patients presenting with signs of shock (hypovolemic, cardiogenic, septic, and neurogenic). d. Pain management of specific needs appropriate for inmates. e. Appropriate pharmacologic therapy of medications commonly used in the correctional facility setting. f. Complications including, but not limited to: fever, infections, thrombophlebitis, urinary retention, atelectasis, pneumonia, pulmonary embolus and other sequelae of extended bed rest. g. Factors related to infection including: pathogenesis, nosocomial infection (e.g. Clostridium difficile, methicillin-resistant staphylococcus aureus [MRSA], central line infection). h. Legal considerations in reference to obtaining informed consent and permits in special circumstances. 8. Demonstrate proficiency with documentation on patient progress notes 84 and with appropriate orders by writing progress notes on all assigned patients. 9. Participate in the management of patients, including patient education, in collaboration with a preceptor. 10. Participate in the appropriate management of: a. Fluid, electrolyte and acid-base problems. b. Patients presenting with signs of shock (hypovolemic, cardiogenic, septic, and neurogenic). c. Chronic pain during the length of incarceration. d. Pharmacologic therapy related to specific diagnosis. e. Problems arising from extended bed rest including, but not limited to: fever, infections, thrombophlebitis, urinary retention, atelectasis, pneumonia, pulmonary embolus, and skin breakdown. f. Factors related to infection including pathogenesis and antibiotic use. g. Patient nutritional status including prolonged NPO status, tube feedings and hyperalimentation (Hospice Inmates). 11. Demonstrate proficiency in: a. Participating in the formulation of discontinuation plans. b. Providing accurate patient education regarding the disease process, plan of care and rationale for treatment. 12. Participation/Observation of Plan of Care Conference. 85 Care of the inmate allows students insight into the problems and rewards of taking care of the corrections population. Students will be exposed to problems such as limited personal space for the inmates and the stress this can produce. They will be exposed to ideas such as solitary confinement needed to prevent pandemic episodes in such a secluded population. Sincerely, Program Director FNP/PA Program Medical Director FNP/PA Program 86 General Information: Students in the UCD FNP/PA program are trained through the community preceptorship model to serve in primary care situations. They are “special status” students in the School of Medicine. Ideally, students will function at approximately the same level as a third year medical student. In accordance with state law and sound practice, students should be supervised at all times. All findings should be reviewed by the resident or attending physician and all invasive procedures should be observed until competency is ensured. When assisting procedures, the student cannot substitute for a licensed physician or other certified personnel when state law, hospital regulations or sound medical practice dictates that licensed or certified personnel serve that function. If a problem should arise - Please Call: Forrest Long, FNP-C, PA, MSN, Faculty, Family Nurse Practitioner/ Physician Assistant Program, Office: (916) 734-1493 or Pager: (209) 995-4592 87 H&P CONTENT REQUIREMENTS (Example) 1. ADMISSION DATE and CHIEF COMPLAINT 2. HISTORY of PRESENT ILLNESS (the source and results of pertinent pre-admission laboratory, x-ray, and/or consultation date when available) 3. PAST MEDICAL HISTORY (allergies; operations; injuries, illnesses; pregnancies; previous medications) 4. SOCIAL HISTORY (marital history; occupational history; habits, particularly alcohol, drug and smoking habits) 5. FAMILY HISTORY 6. REVIEW OF SYSTEMS (cardiac; respiratory; gastrointestinal; genitourinary; gynecological; neuromuscular; skeletal; endocrine). 7. PHYSICAL EXAMINATION (general appearance; sex; race; vital signs (temperature, pulse, blood pressure, respirations); skin; HEENT; funduscopic exam (optional for normal newborn and pediatrics); neck; lymphatics; cardiovascular/pulses; chest; lungs; back/spine; abdomen; rectal; pelvic/genitalia; breast; musculoskeletal; neurologic (minimental status; cranial nerves; deep tendon reflexes; motor; cerebellar; sensory). 8. ASSESSMENT AND PLAN CONSULTATION CONTENT REQUIREMENTS (Example) 1. TYPE OF CONSULT and CONSULT DATE 2. REQUESTING PHYSICIAN 3. REASON for consultation 4. PERTINENT PAST MEDICAL HISTORY, FAMILY HISTORY, SOCIAL 88 HISTORY, and SYSTEMS REVIEW (“Refer to dictated History & Physical” statement is acceptable) 5. Significant LABORATORY and RADIOLOGY FINDINGS 6. ASSESSMENT and RECOMMENDATIONS Student Signature, Co-Signature 89 EXAMPLE OF PROCEDURE NOTE (Example) 1/25/04 Procedure note-lumbar puncture 3:00 am Procedure-lumbar puncture. Indications – Patient admitted with mental status change, combative and confused. Not able to obtain history – blood ETOH negative. Elevated WBC and fever. R/O CNS infection. Consent – Risks, benefits and alternatives have been explained to thee patient who agrees to procedure and has signed consent. (In front of chart). Major risks including, but not limited to; bleeding, infection or possible neurological damage have been explained. Patient unable to sign consent due to confusion and mental status change. Procedure considered emergent- two licensed physicians have signed consent. Procedure– patient was placed in the left lateral decubitus position with knees to chest. With sterile technique the back was prepped with betadine and draped. Local anesthesia was obtained with 1.5cc 2% lidocaine. A 25 gauge spinal needle was introduced into the L/4-L/5 interspace and 4cc of clear fluid was collected in 4 tubes. O.P. (opening pressure)=15cm H20. Tubes sent for VDRL, bacterial and fungal culture, stat gram stain, cell count, differential protein, and glucose. Needle was withdrawn and pressure held until bleeding stopped. Pt. tolerated procedure without difficulty. Complications - None Student Signature, Co-Signature 90 PRESCRIPTION WRITING Students may be asked to write discharge prescriptions or prescriptions for clinic patients. To do this, blank prescription forms are used (available from ward clerk or in clinic). Controlled substances must be written by the signing prescriber – therefore, you may not write any part of these prescriptions.) 1. Stamp the patient’s name/medical record number with their Address-O-Graph card. 2. Write on: First line: Name of drug (generic), strength, and number to be dispensed. Second line: How many to take at what interval and route. Third line: Special instructions (e.g. with meals, take until gone). EXAMPLE: Ampicillin 500 mg tablets #40 1 tablet PO q6h x 10 days Take all capsules Refill Ø. 3. Mark number of refills patient is allowed (lower left corner). For antibiotics or one time medications, mark zero. For antacids or chronically used medications like insulin, prescribe more than one refill or at least make sure they will have enough until their next appointment. 4. The intern or resident signs the prescription(s) and stamps with his/her California license & DEA numbers (students do not sign prescriptions). 91 UNIVERSITY OF CALIFORNIA, DAVIS FNP/PA PROGRAM CORRECTIONAL FACILITY PACKET CHECKLIST This checklist should be the first page of the student’s completed Correctional Facility packet. Student Name: ________________________Rotation Dates:_____________________ Facility Name: _________________________Preceptor Name:___________________ The following information must be submitted to the Correctional Facility Rotation IOR within 30 days of completion of the rotation. All forms are found in the “Forms and Samples” section. Secure ONLY the following paperwork (do NOT submit your entire syllabus). Submit paperwork to the IOR in the following order: 1. Correctional Facility PCR Sheet. 2. Correctional Facility MCR Sheet. 3. Summary of Objectives for Correctional Facility Rotation. 4. Student’s Evaluation of Preceptor and one other clinician who consistently participated in the teaching. 5. Correctional Facility Preceptor’s Evaluation of Student: The Preceptor and one other clinician will be evaluating you. They will submit the evaluations to the student who will include it in the Rotation completion packet to be submitted to the IOR. 40% of your grade is determined by their evaluations. 92 UNIVERSITY OF CALIFORNIA, DAVIS FNP/PA PROGRAM CORRECTIONAL FACILITY PCR’s 001 002 003 004 005 006 007 008 009 010 011 012 013 014 015 016 017 018 019 020 021 022 023 024 025 026 027 028 029 030 031 032 033 034 93 UNIVERSITY OF CALIFORNIA, DAVIS FNP/PA PROGRAM CORRECTIONAL FACILITY PCR’s 035 036 037 038 039 010 041 042 043 044 045 046 047 048 049 050 051 052 053 054 055 056 057 058 059 060 061 062 063 064 065 066 067 068 94 UNIVERSITY OF CALIFORNIA, DAVIS FNP/PA PROGRAM CORRECTIONAL FACILITY PCR’s 069 070 071 072 073 074 075 076 077 078 079 080 081 082 083 084 085 086 087 088 089 090 091 092 093 094 095 096 097 098 099 100 101 102 95 UNIERSITY OF CALIFORNIA, DAVIS FNP/PA PROGRAM CORRECTIONAL FACILITY MCRs Task Date: Patient ID Patient Diagnosis Preceptor Signature Abscess I&D Abscess I&D Bipolar DX Bipolar DX Trauma/Injury Trauma/Injury Hep. C Hep. C HIV/AIDS HIV/AIDS HIV/AIDS HIV/AIDS Stress/Depression Stress/Depression Stress/Depression CHF Edema DM Suture placement CA - any Pain Management Pain Management HTN HTN RASH RASH URI/TB URI/TB Complete H&P/HCM Complete H&P/HCM Complete H&P/HCM _________________________________________ ____________________________ Student Signature Date 96 Summary of Objectives for Correctional Facility Rotation At the end of each day, review this form and record those objectives you have been able to achieve. This will help you identify specific areas to focus on in your clinical experience, and make it easier to complete your typed summary (using this format) at the end of the rotation. Discuss how you have met the following objectives: 1. Recognize when a patient needs higher levels of medical care. 2. Obtain and record an appropriate medical history. 3. Perform and record an appropriate physical exam. 4. Order, record, and interpret appropriate laboratory and diagnostic tests for assigned patients in collaboration with a preceptor. 5. Perform basic medical and surgical procedures appropriate for the diagnosis of the specific inmates (abscess I&D, laceration repair, medication injections, etc.). 6. Demonstrate familiarity with the correctional facility setting, departments (their functions), and ancillary resources. 7. Demonstrate knowledge of the following: a. Common fluid, electrolyte and related acid-base problems. b. Volume replacement as to type, amount, and rate of replacement based on specific need or diagnosis. c. Patients presenting with signs of shock (hypovolemic, cardiogenic, septic, and neurogenic). d. Pain management of specific needs appropriate for inmates. 97 e. Appropriate pharmacologic therapy of medications commonly used in the correctional facility setting. f. Complications including, but not limited to: fever, infections, thrombophlebitis, urinary retention, atelectasis, pneumonia, pulmonary embolus and other sequelae of extended bed rest. g. Factors related to infection including: pathogenesis, nosocomial infection (e.g. Clostridium difficile, methicillin-resistant staphylococcus aureus [MRSA], central line infection). h. Legal considerations in reference to obtaining informed consent and permits in special circumstances. 8. Demonstrate proficiency with documentation on patient progress notes and with appropriate orders by writing progress notes on all assigned patients. 9. Participate in the management of patients, including patient education, in collaboration with a preceptor. 10. Participate in the appropriate management of: a. Fluid, electrolyte and acid-base problems. b. Patients presenting with signs of shock (hypovolemic, cardiogenic, septic, and neurogenic). c. Chronic pain during the length of incarceration. d. Pharmacologic therapy related to specific diagnosis. e. Problems arising from extended bed rest including, but not limited to: fever, infections, thrombophlebitis, urinary retention, atelectasis, 98 pneumonia, pulmonary embolus, and skin breakdown. f. Factors related to infection including pathogenesis and antibiotic use. g. Patient nutritional status including prolonged NPO status, tube feedings and hyperalimentation (Hospice Inmates). 11. Demonstrate proficiency in: a. Participating in the formulation of discontinuation plans. b. Providing accurate patient education regarding the disease process, plan of care and rationale for treatment. 12. Participation/Observation of Plan of Care Conference. 99 100 101 UNIVERSITY OF CALIFORNIA, DAVIS FNP/PA PROGRAM STUDENT EVALUATION OF PRECEPTOR Preceptor Name:________________________Rotation Date:______________________ Rotation Location:______________________Student Name:_______________________ Circle the number that corresponds to your evaluation of the Preceptor: 5=Excellent 1=Poor N=Not Applicable Medical Information is Current: Reliable: Relevant: 5 5 5 4 4 4 3 3 3 2 2 2 1 1 1 When Precepting Procedures: Willing to Assist: Helpful Instructions: 5 5 4 4 3 3 2 2 1 1 Interaction w/ Students: Listens Well Guides without Controlling: Is Available: Gives Feedback: Ability to Teach: 5 5 5 5 5 4 4 4 4 4 3 3 3 3 3 2 2 2 2 2 1 1 1 1 1 If Feedback is given, is it: Useful: Supportive: 5 5 4 4 3 3 2 2 1 1 Overall Evaluation: 5 4 3 2 1 Would you recommend this preceptor/clinician to other students? Explain: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 102 GENERAL ROTATION POLICIES & PROCEDURES The UC Davis Health System “Blood/Body Fluid Exposure” and “Needlestick” Hospital Policies and Procedures – 2167 Revised 7/26/04 have been added to give students a sample of the types of policies and procedures to review before starting the Inpatient rotation. Student Bloodborne Pathogen Exposure Control Plan By University administrative procedure, Cowell Student Health Center maintains an exposure control plan for all students whose course work duties include routine or reasonably anticipated tasks or procedures where there is actual or potential exposure to blood or other infectious material posing a risk for bloodborne pathogen transmission. Exposure Prevention Students covered by this policy will receive instruction in exposure prevention in accordance with guidelines from USPHS on bloodborne pathogen precautions through their departments, colleges and educational or internship programs. Upon a studentpatient’s individual request, Cowell clinical staff may provide individual exposure prevention education as clinically appropriate. In such cases, the following exposure prevention guidelines shall be advocated: 1. Bloodborne pathogen precautions are intended to supplement and not replace outine infection control recommendations, such as hand washing and the use of gloves to prevent gross bacterial contamination of the hands. 2. Bloodborne pathogen precautions apply to blood and other body fluids containing visible blood. Blood is the single most important source of HIV, 103 Hepatitis B virus, and other bloodborne pathogens. These precautions also apply to tissues, semen, vaginal secretions, and the following fluids: cerebral spinal, synovial, pleural, peritoneal, pericardial, and amniotic. These precautions do not apply to feces, nasal secretions, sputum, saliva, sweat, tears, urine, and vomitus that do not contain visible blood. 3. The following precautions are to be observed by all persons with potential exposure to the potentially infectious material identified above: A. Appropriate barrier precautions should be used routinely to prevent skin and mucous membrane exposure whenever contact with blood or bodily fluids is anticipated in the patient care setting. Gloves should be worn for touching skin, body fluids, mucous membranes, non-intact skin, for handling items or surfaces contaminated with blood or body fluids, and for performing venipuncture or other vascular access procedures. Masks and protective eyewear or face shields should be worn during procedures that are likely to generate droplets of blood or other body fluids to prevent exposure of mucous membranes of the mouth, nose, and eyes. Gowns or aprons are to be worn during procedures that are likely to generate splashes of blood and other body fluids. B. Gloves should be changed after contact with each patient. Gloves should not be washed or disinfected for reuse. They should not be used when visibly soiled, torn, punctured, or when their ability to function as a barrier is compromised. 104 C. All personal protective equipment should be removed immediately upon leaving the work area and placed in appropriately designed areas or containers for storage, washing, decontamination, or disposal. D. Hands and other skin surfaces should be washed thoroughly with soap and water. Mucous membranes should be flushed with water immediately or as soon as feasible if contaminated with blood or body fluids. Hands should be washed immediately after gloves or other personal protective equipment is removed. 1) All procedures involving blood or other potentially infectious material shall be performed in such a manner as to minimize splashing, spray, or aerosolization of these substances. i) Precautions should be taken to prevent injuries caused by needles, scalpels and other sharp instruments or devices while handling instruments during procedures, and with disposal or cleaning of instruments after procedures. Needles should not be recapped, bent or broken by hand, removed from syringes, or otherwise manipulated. After use, disposable sharps should be placed in puncture resistant containers. Reusable sharp instruments and large bore needles should be placed in appropriate puncture resistant containers for cleaning. ii) To minimize the need for mouth-to-mouth resuscitation, 105 mouthpieces, resuscitation bags, and pocket masks should be used preferentially to initiate respiratory resuscitation. E. People with exudative or weeping dermatitis should avoid direct patient contact and handling of patient care equipment until the condition has resolved. F. Eating, drinking, smoking, applying cosmetics, lip balm, or contact lenses should never be done in patient care areas, laboratories, or other areas where potentially infectious materials may be present. Pre-Exposure Bloodborne Pathogen Prophylaxis All students covered by this policy should be evaluated for pre-exposure immunity and vaccination status for bloodborne pathogens for which testing and/or immunization procedures are available. Currently antibody testing and vaccine induced immunity have only been developed for Hepatitis B virus. Immunity testing and immunization is the financial responsibility of the student. Medical Students and NP/PA program participants are required to document adequate Hepatitis B vaccination or antibody titers to meet school and program entrance requirements. Students may have antibody titer testing and/or vaccination for Hepatitis B virus performed at Cowell Student Health. Persons seeking to demonstrate naturally acquired immunity shall document adequate titers of Hepatitis B core antibody. Persons demonstrating immunity following vaccination shall document adequate titers of Hepatitis B surface antibody. All persons who have completed a Hepatitis B vaccination 106 series are advised to demonstrate adequate immunity by having Hepatitis B surface antibody testing at least one month after their last injection, however, documentation of this testing is not essential to meeting the Hepatitis B immunization entrance requirement. Post-Exposure Bloodborne Pathogen Prophylaxis /Wound Care Any student covered by this policy who has a parenteral or mucous membrane exposure to blood or other body fluids or who has a cutaneous exposure involving large amounts of blood or prolonged contact with blood, especially when the exposed skin is chapped, abraded, or affected with dermatitis should decontaminate the exposed area and have a medical evaluation of the exposure risk. In the event of exposure, immediate wound care measures should be taken to decontaminate the area. Students covered by this document are advised the following wound care instructions: 1) Needle stick and open skin exposure: Thoroughly scrub the area with betadine solution and water for 3-5 minutes. 2) Mucous membrane exposure: Thoroughly rinse with plain water for 5 minutes. Following wound care, medical evaluation should be sought. Medical Evaluation Sites All registered students are eligible to receive medical evaluation for blood and body fluid exposures at Cowell Student Health Center. Exposed persons should phone (530) 752-2300 to arrange care with the Student Health Center Advice Nurse prior to arriving at the center. Evaluation is available at the center’s Urgent Care during all clinic 107 hours. Cowell Student Health Center is closed during University holidays. If Student Health is closed, call UCDMC Infection Control (916) 734-2011, Hospital Infection Control Nursing Supervisor. Students must call (916) 734-2011 to speak to the Hospital Infection Control Nursing Supervisor to arrange for care. MS I and MS II students are provided a “Blood and Body Fluid Exposure Wallet Card” to advise them of the contact persons available for medical evaluation of exposure risks. Students whose course work or internship site provides an Employee Health or Occupational Medicine service should check to see if they are eligible for care in association with their program activity. Every medical facility will have a policy regarding blood and body fluid exposure and should inform students in their facility of their eligibility for evaluation after an exposure event. Students who are unable to access care at the facility site or any of the above facilities are advised to seek care at the nearest urgent care or emergency department. Medical evaluation and post-exposure prophylaxis are the financial responsibility of the student. Students may seek to have the cost of care covered by their private health insurance. Students covered by University administered student insurance (GSHIP/USHIP) should contact the Patient Accounts office at the Student Health Center at (530) 752-2612 as soon as possible whenever care is received. (Benefits under GSHIP and USHIP require authorization for care. Claims are paid in accordance with specific benefits and limitations of each plan) Medical Evaluation Procedures The medical evaluation of any student sustaining parenteral of mucous membrane 108 exposure to blood or body fluids (or a significant cutaneous exposure to these potentially infectious materials) will include a documentation of the circumstances of the exposure including: 1. The route(s) of exposure. 2. The activity/procedure resulting in exposure. 3. The extent of exposure. 4. The source of exposure. 5. The exposed student’s vaccination history for Hepatitis B virus (and tetanus prophylaxis if appropriate) as well as pre-exposure Hepatitis B, Hepatitis C, and HIV antibody status. Exposures involving a puncture wound shall receive vigorous cleaning and thorough wound care in addition to assessment of bloodborne pathogen risk. All should be evaluated for tetanus prophylaxis. Injuries should be followed up for any sign of bacterial infection at the wound site. Post-exposure prophylaxis requires an assessment of the HBV, HCV, and HIV infectivity risk of the potentially infectious material. After appropriate consent has been obtained, the source individual (unless unidentifiable) will be tested for Hepatitis B, Hepatitis C and HIV infectivity. Blood samples for Hepatitis B surface antigen, Hepatitis B core antibody, ALT, Hepatitis C antibody, and HIV antibody will be drawn. When consent is not legally required, available blood samples shall be tested and results documented. Source individuals are provided pre-test and post-test counseling and referral as needed. Results of the source individual’s testing shall be made available to 109 the exposed person along with information regarding applicable laws and regulations concerning disclosure of the source’s identity and infectious status. In the event of an unidentified source of blood or body fluid exposure, the contaminated instrument, equipment, or potentially infectious material should be retrieved by an area supervisor (using appropriate safety precautions) for possible bloodborne pathogen testing whenever possible. Post-exposure prophylaxis requires an assessment of the susceptibility of the exposed person to HBV, HCV and HIV. After appropriate consent has been obtained, the exposed student shall have serology testing for Hepatitis B surface antigen, Hepatitis B core and surface antibody, Hepatitis C antibody, ALT, and HIV antibody. Pre-test and post-test counseling for HIV serology shall be provided. Students who decline consent for HIV serological testing are advised to have a sample drawn and preserved for at least 90 days in the event they elect to have testing at a later date. Hepatitis B Virus Exposure When the source is negative for Hepatitis B surface antigen, no post-exposure prophylaxis is required, however previously unvaccinated individuals should be started on the pre-exposure prophylaxis hepatitis B vaccination series. Exposed persons whose vaccination series is not complete should resume and complete pre-exposure prophylaxis. Persons previously vaccination should have a Hepatitis B surface antibody checked with each exposure. Persons who have been previously vaccinated and are known nonresponders to vaccine require no additional Hepatitis B antibody testing. When the source serology is unknown or the source is unavailable for testing, 110 Hepatitis B risk may be estimated from the medical or personal history of the source. Risk for transmission of bloodborne pathogen related diseases is high for source patients with the following histories: 1. Acute hepatitis (symptoms or clinical findings) or undetermined etiology. 2. Intravenous drug users. 3. Homosexual males. 4. Prisoners/Prostitutes. 5. Recipients of blood products or transfusions. 6. Renal dialysis patients. 7. Patient with history of long-term institutional care for mental illness or developmental disability. 8. Asian immigrants. 9. Known HIV+ history. High risk source patients may be assumed for purposes of post-exposure prophylaxis to be positive for Hepatitis B virus infectivity and exposed persons should be advised post exposure prophylaxis accordingly (see below). Where source history is completely unavailable, and there is no known high risk, it is appropriate to: 1. begin or complete the vaccination series for unvaccinated or incompletely vaccinated exposees. 2. give a single vaccine booster dose to exposed persons who have been vaccinated and demonstrate current inadequate Hepatitis B surface antibody levels. 111 3. give Hepatitis B Immunoglobulin post-exposure and one month later to persons who are known non-responders to the vaccination series. When the source tests positive for Hepatitis B surface antigen, Hepatitis B prophylaxis is required unless the exposed person has naturally acquired immunity (known Hepatitis B core antibody+ status) or has received a complete vaccine series and is known to have adequate Hepatitis B surface antibody levels within the last two years. The following procedures are advised based on the vaccination history and the Hepatitis B surface antibody status of the exposed person: 1. Exposee not previously vaccinated: Start vaccine series and give 1 dose of HBIG* (0.06ml/kg). 2. Exposee incompletely vaccinated: Finish vaccine series and give 1 dose of HBIG (0.06ml/kg) 3. Exposee vaccinated with adequate titer (>10mlU/ml): No treatment. 4. Exposee vaccinated with inadequate titer (<10mlU/ml) and prior history of adequate titer: Give single booster dose of vaccine. 5. Exposee vaccinated with inadequate titer (<10mlU/ml) and no prior adequate titer: Restart Vaccine series and give 1 dose of HBIG (0.06ml/kg). 6. Exposee vaccinated and known non-responder to vaccine series: Give 1 dose of HBIG (0.06ml/kg) now and second dose 1 month later. *HBIG should be administered as soon as possible after an exposure, preferably within the first 72 hours. Except in unusual circumstances it must be administered within 7 days of exposure to reduce Hepatitis B virus risk. 112 Hepatitis C Virus Exposure Assessment of bloodborne pathogen exposure for Hepatitis C virus is complicated by a lack of diagnostic tests to confirm infectivity of the source or susceptibility of the exposee. Additionally, there are no current pre-exposure or post-exposure prophylactic therapies known to be effective. Testing the source for Hepatitis C antibody, Hepatitis B core antibody, and ALT will help determine if the potentially infectious material poses a high risk for Hepatitis C virus transmission. Testing the exposee for Hepatitis C antibody, Hepatitis B core antibody and ALT will help determine if the exposee is likely to have pre-existing Hepatitis C virus exposure or natural immunity. When the source tests positive for Hepatitis C antibody, Hepatitis B core antibody, or elevated ALT, the exposee should receive follow-up testing of liver function tests at 6 weeks (and again at 3 and 6 months). Hepatitis C antibody testing should be performed at 6 months unless exposee is already known to be Hepatitis C antibody positive. At the current time there is no pre or post exposure prophylaxis. HIV Exposure Assessment of HIV risk from blood and body fluid exposure is dependent upon HIV status of both the source and the exposee as well as the extent of exposure. Testing of both the source and exposee requires informed consent and pre and post test counseling. Local laws may permit testing of available source blood without HIV testing consent, in the event of an exposure to blood and body fluids by: 1. a health care professional. 2. an employee, volunteer or contracted agent of a health care provider. 113 3. emergency response personnel [SD 1239, 1993-94 Stat. Ch 708; Cal Health and Safety Code 199.65 et.seq.]. Where the source is unavailable for testing, high-risk status may be assumed if the source is male homosexual or an injection drug user. The determination to use post-exposure prophylaxis is also based on the degree of exposure. Significant exposure includes the following events: 1. needle stick or cut from a needle or sharp object visibly contaminated with blood or body fluids. 2. splash of blood or body fluids to open cuts, dermatitis, or abraded skin. 3. splashing blood or body fluids onto a mucous membrane: eye, nose or mouth. Exposures to potential infectious material from a source individual known to be HIV+ or high risk for HIV infection warrants exposee counseling regarding infection risk, transmission prevention, follow-up clinical evaluation and testing for evidence of HIV infection. Following the initial test for HIV, the exposee should be retested at 6 weeks, 12 weeks, and again at 6 months after the exposure. The exposee should be advised to receive medical evaluation for any acute febrile.illness within 12 weeks of exposure particularly if characterized by fever, rash, or lymphadenopathy. HIV post-exposure management is an evolving area of infectious disease medicine. The exposee should be informed of the current USPHS guidelines for postexposure management. A consultation should be obtained for any definitive exposure to 114 known HIV+ source blood or body fluids for current recommendations. Contact should be made with one of the following: UCDMC Infection Control Services (Dr. Stuart Cohen, beeper (916) 762-6021; or Nursing Supervisor, beeper (916) 762-5364; or Infectious Disease Fellow on-call available through the hospital operator at (916) 7342011). You may also refer to your Bloodborne Pathogen Exposure laminated wallet card for these important directions and phone numbers, since you are unlikely to have this manual in the clinical setting with you. Record the exposure incident on-line to UCDMC Employee Health at www-med.ucdavis.edu/. When the UC Davis School of Medicine home page appears, type in the following in the “Location” window: “employee exposure”. This is the official record of the exposure, and there will be a prompt to print the required laboratory forms you will need. Susan Sutherland, RN is the BBP Exposure Nurse, 916-734-7585. Since 1998, post-exposure chemoprophylaxis has been recommended for selected exposure circumstances. (See current CDC recommendations at: www.cdc.gov/mmwr/ “Public Health Service Guidelines for the Management of Health care Worker Exposures to HIV & Recommendations for Post-exposure Prophylaxis”; May 15, 1998/47 (RR-7); 1-28 or most current recommendations. Recommended prophylaxis for selected exposure circumstances include: 1. Massive exposure – Recommended. 2. Needlestick or injection of blood – Endorsed. 3. Superficial puncture or mucous - Available (most appropriate). 4. Membrane contact if source suspected of high HIV viremia. 115 5. Low risk body fluid contact – Discouraged. 6. Cutaneous contact - Not available. Persons prescribed chemoprophylaxis should receive counseling regarding the risks and benefits of chemoprophylaxis. They should also receive contraceptive counseling. Before beginning chemoprophylaxis, a baseline blood profile should be obtained to include CBC with platelet count, chemistry panel, and urinalysis. All persons prescribed chemoprophylaxis should be referred for ongoing medical care. Multidrug antiretroviral therapy may not be required for some individuals if the source patient had not taken antiretroviral drugs in the past, or if the exposure was considered low risk. If the patient medication history of HIV + status cannot be determined within 2 hours after exposure incident, then multidrug therapy should be initiated. The current drugs of choice are zidovudine, lamivudine and nelfinivir. Administration of drugs should be taken within two hours of a known HIV+ bolus exposure. 116 UC Davis Health System Blood/Body Fluid Exposure (Needlestick) Hospital Policies and Procedures - 2167 Revised 7/26/04 I. PURPOSE This section outlines the policy and procedures to be followed for the treatment of employees suffering accidental exposures to human immunodeficiency virus (HIV) via blood or body fluids. It also provides guidelines for prophylaxis of employees who sustain blood or mucous membrane exposure to blood or high-risk fluids as the result of accidents such as needlestick, puncture, scalpel laceration, human bite or blood splash on mucous membrane (eye, mouth, nose), and outlines the policy and procedures for cleansing the skin, eyes, mouth or personal clothing following exposure to blood at the University of California, Davis, Health System (UCDHS). II. SETTING Health System III. DEFINITION Employee—for purposes of this section, employee means those persons employed by, being trained at or affiliated with UCDHS. This includes UCDHS staff employees, UCD campus or School of Medicine personnel assigned to UCDHS, volunteers, active medical staff (with the exception of volunteer faculty), medical students, interpreters, temporary staff and contractual employees. 117 Body fluids—semen, vaginal or cervical secretions, peritoneal fluid, blood products, cerebrospinal fluids, synovial fluid, pleural fluid, pericardial fluid, amniotic fluid and concentrated HIV viruses. Exposure—the definitions listed below refer to blood/body fluids from known HIV-infected patients. A. Massive exposure: Transfusion of blood. Injection of large volume of blood/body fluids (1ml) or parenteral exposure to laboratory specimens containing high titers of human immunodeficiency virus. B. Definite parenteral exposure: Intramuscular (IM/deep) injury, injection of blood/body fluid other than transfusion, bleeding wound, such as a laceration produced by an instrument that is visibly contaminated with blood or body fluids or laceration or similar flesh wound inoculated with blood/body fluid. Any inoculation with HIV (usually research setting) not included in paragraph IV C.1.a-c, above. C. Possible parenteral exposure: Subcutaneous (SQ/superficial) injury, a wound produced by blood/body fluid-contaminated instrument that does not cause visible bleeding, existing wound or skin lesion, or a Mucous membrane inoculation with blood/body fluid. D. Doubtful parenteral exposure that occurs with non-bloody body fluid. E. Non-parenteral exposure—intact skin visibly contaminated with blood/body fluid. IV. POLICY 118 Employees shall receive appropriate prophylaxis for all needlestick injuries, scalpel wounds or any type of break in the skin surface contaminated with patient’s blood or high-risk body fluids or for contamination of mucous membranes with patient’s blood. A. Known Source B. HIV prophylaxis is recommended for all hospital employees who suffer MASSIVE or DEFINITE parenteral exposure to HIV via blood or body fluids, as defined above. C. Unknown Source But High Risk for HIV Employees with MASSIVE exposures to blood/body fluids from high-risk patients may also be offered HIV prophylaxis. High-risk patients include hemophiliacs, male homosexuals, IV drug users and prisoners. V. PROCEDURE/RESPONSIBILITY A. Employees shall receive appropriate treatment or prophylaxis ( based on risk factors or source patients lab results) for needlestick injuries, scalpel wounds or any type of break in the skin surface contaminated with patient’s blood or highrisk body fluids or for contamination of mucous membranes with patient’s blood. B. The immediate reporting and work up of a blood and body fluid exposure (needlestick) is urgent. The work up includes the ordering of lab tests and the assessment of risk factors on the source patient. C. The lab tests to be ordered are: 1. HBsAg—hepatitis B surface antigen. Positive test indicates carrier of 119 hepatitis B. 2. Hepatitis C antibody. 3. Rapid HIV—human immunodeficiency virus. Positive test suggests carrier of AIDS virus. D. Risk factors are listed on the Employee Report of Blood/Body Fluid Exposure or Needlestick form (#71431-048 or 71463-376) or by the Incident Reporting System (IR) and are used to evaluate an employee’s risk of exposure to hepatitis B, hepatitis C or HIV. E. The results of lab tests and risk factors are used to determine a treatment plan for the exposed employee. F. Employee: 1. First aid, scrub the wound site with antimicrobial solution (Betadine or Exidine) for three minutes; or rinse mucous membrane (eye, mouth) contamination with water for five minutes. 2. Contact the charge nurse of the unit the patient is on if help is needed to order appropriate lab tests or identify risk factors on the source patient. If the patient cannot be located in the hospital, call Bed Control (extension 42456) to obtain that information. It is not necessary to contact the unit charge nurse if no assistance is needed to complete the report form or order the necessary laboratory tests. 3. Complete the Employee Report of Blood/Body Fluid Exposure, Needlestick form, or use the IR to report the incident. Without the form, 120 no labs can be sent. Forms are available in patient care areas. 4. Verify that the report form is fully completed and that risk factors have been identified. Verify that lab tests have been ordered. 5. The exposed person keeps a copy (goldenrod) of exposure report form and forwards the first two pages to Patient Care Services administrative office, Main Hospital, 4th floor for EHS pick up Monday through Friday; or it can be hand carried to EHS. 6. Notify EHS during business hours or the nursing supervisor after 4:00 p.m. weekdays, weekends and holidays. Regardless whether EHS is closed report the exposure to the Bloodborne Pathogen phone line at 734 - 7585. EHS will provide all the treatments and follow ups for all exposures. Location: EHS: Cypress Building suite “A,” Phone: 4-7585 - Days: Monday through Friday - Hours: 7:00 am to 4:00 pm. EHS will telephone the employee for follow-up. Do not go to the Emergency Department for needlestick exposure unless emergency care is needed (e.g., for a laceration requiring sutures). Baseline labs on the employee can be done within three days after the exposure date and are to be drawn in EHS only. G. Nursing Supervisor 1. Act as contact person when EHS is closed. 2. Assure that employee has cleansed area appropriately and has initiated first aid. 3. Instruct employee to initiate the exposure procedure. Use only current 121 report forms or use the Incident Reporting System (IR). Contact the charge nurse of the unit the patient is on and request assistance in history of known risk factors or assist in ordering appropriate lab tests. If the source patient is unknown, indicate this in the upper left-hand corner box of the report form, and forward to EHS within 24 hours (or sooner if needlestick is at a high-risk area) of the incident. For additional help after 4 pm weekdays, weekends and holidays, regarding exposure, contact the ID Fellow on call. 4. Receive call from employee reporting exposure to known HIV-positive patient or high-risk HIV patient. Contact the on-call ID Fellow for employees seeking consideration for prophylactic therapy. a. For massive or definite exposure to a known HIV-positive source, send the employee directly to EHS for treatment during normal business hours. b. If EHS is closed, call the Infectious Disease Fellow listed oncall or available by calling the hospital operator and asking for the Occupational Exposure number. c. Medications are prescribed based on risk factors or HIV viral loads and antiviral medications an HIV positive patient is currently taking. H. Unit Charge Nurse 1. Patient risk factors: Assess risk factors of the source patient for all 122 exposures. Check appropriate risk factors on Employee Report of Blood/Body Fluid Exposure, Needlestick form, or use the IR system. 2. Known patient source: a. Have the source patient’s blood drawn for needlestick/body fluid-secretion exposure as soon as possible and send the pink copy of the Bloodborne Pathogen Exposure Report form with two tubes of blood and hand carry to North 2 lab for rapid HIV test. If using the IR reporting system the lab slip will not be pink. The IR will print the appropriate lab slip according to risk factors identified. b. For all exposures, instruct employee to contact the EHS Bloodborne pathogen phone line at 734-7585 within 24 hours. c. EHS will contact the employee as soon as possible. 3. Unknown source patient: Write Source Unknown in the upper left-hand corner box and complete remainder of report form. EHS will follow up as necessary. During business hours contact EHS or send employee immediately. After 4 p.m. weekdays, weekends and holidays, call the Nursing Supervisor to assist you. 4. HIV screening: a. Obtain informed consent on the Consent for HIV Antibody Testing form (#71431-087) prior to obtaining a blood sample for testing for HIV antibody (antibody to the AIDS virus). For further 123 information see UCDHS Policies and Procedures Section 1425, Obtaining HIV Antibody Tests and Counseling Patients with Suspected Exposure to the AIDS Virus. NOTE: Patient must consent to HIV testing before the test can be conducted. The source patient’s attending physician, legal designee or other licensed personnel can consent the source patient. b. HIV can be done on a refusal (for further information, telephone the EHS manager at 734-7585, or consult the Bloodborne Pathogen Users Guide which is available at every nurses station or the Nursing Supervisor). I. Employee Health Services 1. Provide appropriate follow-up to employee following EHS Needlestick Policy and Procedure. 2. If employee has not contacted EHS within 72 hours with an exposure to blood from a high-risk body fluid of known hepatitis or “high-risk” patient, this may delay treatment. 3. Contact employee by letter with source patients lab results and recommendations for follow-up. 4. Maintain log of all Employee Report of Blood/Body Fluid Exposure or Needlestick forms. VI. VARIANCE IN PROTOCOL FOR NEONATAL SOURCE PATIENT 124 Differences in data regarding risk factors and altered immune responses in the neonate necessitate modifications of the protocol for needlestick injuries from these patients. If the mother is also in the hospital, use the mother’s blood, and indicate the mother’s name and unit number in the upper left-hand corner box of the form as well as the name of neonate. The following guidelines should apply: A. HIV and HEP C—serology should preferentially be obtained on the mother. If the mother denies HIV consent, consent should be requested for an HIV test on the infant. Indicate on the report whether the test is pending on the mother or on the neonate. Cord blood is acceptable to use. If the infant has received blood transfusions, mother’s blood will not be acceptable. B. HBsAg—obtain only if the maternal HBsAg is unknown and you are unable to obtain a blood sample. If the mother is HBsAg positive, the infant should be presumed infectious (although this percentage is very low in infants who have received HBIG and HBV vaccine). Indicate the mother’s HBsAg result on the report form. VII. VARIANCE IN PROTOCOL FOR EMERGENCY DEPARTMENT AND LIFE FLIGHT A. The Emergency Department employees may obtain a first dose of triple drug therapy from the charge nurse after the approval from the administrative emergency physician. Life Flight personnel may take triple drug therapy from the medications box after approval by the administrative emergency physician. If the 125 employee needs additional medications (i.e., source patient tests positive for HIV, or testing is delayed, the employee will be instructed to page EHS physician or the on call ID Fellow for further counseling). A verbal prescription of a three day PEP (post-exposure prophylaxis) regime will be called into the second floor pharmacy or, if time permits, to the pharmacy located at the Cypress Building. B. Medications for the Emergency Department and the Life Flight medications box are replaced using the standard drug order form and Pharmacy Stores will deliver during routine deliveries. C. Pharmaceutical Services 1. The intent of this policy is to provide current therapy in accordance with UCD/UCDHS EHS, Division of Infectious and Immunologic Diseases and Infection Control Committee recommendations. Therefore, choice and dosage of the drugs used may change in the future. 2. Multidrug antiretroviral therapy may not be required for some individuals if the source patient had not taken antiretroviral drugs in the past, or if the exposure was considered low risk. If the patient medication history cannot be determined within 2 hours after exposure incident, then multidrug therapy is initiated. 3. The current drugs of choice are zidovudine, lamivudine and nelfinivir. Administration of drugs should be taken within two hours of the exposure to an HIV bolus. 4. Tower 2 Pharmacy will maintain a supply of medication that can be 126 released 24 hours a day by authority of the ID Fellow, EHS MD/NP or the Bloodborne Pathogen Surveillance Nurse. 5. Suspense PEP medications identified by the ID Fellow or EHS provider with confidential codes provided. 6. Ask exposed party while picking up meds if he/she is taking any other meds to ensure if compatible with current regime. 7. Supply medication information sheet if dispensing the PEP medications. D. Clinical Director, Department of Epidemiology and Infection Control Advise Pharmaceutical Services of current policy on medication administration by participation on the Infection Control Committee and the Pharmacy and Therapeutics Committee. VIII. DEFINITIONS OF PERSONAL PROTECTIVE EQUIPMENT A. Personal protective equipment (PPE)--provided by the employer and includes disposable isolation gowns, cover gowns or aprons, gloves, masks and shoe covers. B. Personal clothing—includes any clothing purchased by the employee. IX. POLICY A. Spills or Splashes of Blood onto Broken or Non-Intact Skin: 1. Broken or non-intact skin anywhere on the employee’s body is covered 127 with a band-aid or bandage. 2. If the Band-aid or bandage becomes damp or soaked with blood or body fluids, remove the wet dressing, scrub the broken skin with the approved germicide used for employee handwashing. Replace the bandage using a clean, dry dressing. 3. Skin that becomes broken due to a percutaneous injury with a sharp device is washed for three minutes with the hospital approved germicide used for employee handwashing. 4. Wash skin for three minutes with Hospital approved germicide used for employee handwashing. 5. If clothing (personal, non-disposable and/or uniforms) is soiled with blood or any other bodily fluid, follow the procedures in paragraph IX. C.1-8, below as soon as possible. B. Splashes of Blood to Eyes or Mouth 1. Go to eye wash station or flush eyes under faucet for five minutes. 2. Wash face with soap and water; rinse mouth for five minutes with water. 3. Report exposure to supervisor. 4. Initiate Bloodborne Pathogen Exposure reporting procedure. a. For Blood and Body Fluid Exposure fill out form 71431-048, or access UCDHS Incident Reporting Program by computer. b. Labs are ordered on the source patient by utilizing the 128 Blood/Body Fluid Report form or by the IR program automatically. 5. Contact EHS at 734-7585 to report the incident as soon as possible. C. Care of Personal Clothing Items Soiled with Blood (Includes street clothing or uniforms): 1. Obtain scrub suit from Distribution/Linen Services Department. 2. Put on gloves. 3. Remove clothing; put on scrub suit. 4. Rinse blood from personal clothing using a 1:10 dilution of chlorine bleach and water. a. Request for bleach is made by the employee’s supervisor. Call Environmental Services at 4-8288 (answered 24 hours). b. Employee can pick up the bleach from Environmental Services. c. Employees are to wear eye protection when using bleach. d. Health care settings where blood often soils employee clothing may call Environmental Services to obtain bleach to store on unit. 5. Place decontaminated personal clothing in a plastic bag for transport home. 6. Remove gloves; wash hands. 7. Put on gloves at home to remove clothing from bag. 8. Machine wash clothing alone using warm water and detergent. 9. Caveat: Bleach at high concentration can destroy fabric. Mix bleach 129 wearing eye protection as described in a 1:10 dilution. Do not wear clothing that may be harmed by bleach. Sent to the following for review: Marsha Koopman, RN Neil Speth, DO Susan Sutherland, RN HIPAA Policy Workgroup Medical Staff Executive Committee http://intranet.ucdmc.ucdavis.edu/policies/hosp/2167.htm 7/26/2004 130 REFERENCES Alemagno, S., Wilkinson, M., & Levy, L. (2004). Medical education goes to prison: why? Academic Medicine, 79(2), 123-127. Allen, S. A., Spaulding, A. C., Osei, A. M., Taylor, J. D., Cabral, A. M., & Rich, J. D., (2003). Treatment of chronic hepatitis C in a state correctional facility [Electronic version]. Annals of Internal Medicine, 138(3), 187-190. Retrieved February 18, 2008 from: www.annals.org. American Nurse’s Association, Code of ethics, Retrieved March 14, 2008 from American Nurse’s Association’s web site: http://ana.org/ethics/code/ethicscode150.htm. Blitz, C. L., Wolff, N., & Paap, K. (2006). Availability of behavioral health treatment for women in prison [Electronic version]. Psychiatric Services, 57(3), 356-360. Retrieved February 4, 2008 from: ps.psychiatryonline.org. Burns, N., & Grove, S. K. (2005). The practice of nursing research: conduct, critique, and utilization (5th ed.) (L. Henderson, Ed.). St. Louis, Missouri: Elsevier Saunders. (Original work published 1987). California department of corrections and rehabilitation. (2009). Institution statistics [website]. Available from Ca.gov, Retrieved December 13, 2009 from: http:// www.cdcr.ca.gov/visitors/facilities/cmf-institution_stats.html. Cawley, J. F. (2005). A curriculum in clinical prevention and population health for physician assistants. Perspective on Physician Assistant Education, 16(2), 89-95. Collins, J. (2004, September-October). Education techniques for lifelong learning. Radiographics, 24(5), 1483-1489. 131 Conklin, T. J., Lincoln, T., & Tuthill, R. W. (2000). Self-reported health and prior health behaviors of newly admitted correctional inmates [Electronic version]. American Journal of Public Health, 90(12), 1939-1941. Retrieved February 20, 2008 from: https://vpn.lib.ucdavis.edu/sites/,DanaInfo=www.ncbi.nlm.nih.gov+entrez. Dubik-Unruh, S. (1999). Peer education programs in corrections: curriculum, imlementation, and nursing interventions. Journal of the Association of Nurses in Aids Care, 10(6), 53-62. Essary, A. C., Berry-Lloyd, C., & Morgan, C. (2003). A student-centered approach to physician assistant clinical rotations. Perspective on Physician Assistant Education, 14(2), 78-83. Evans, N. (1999). Preparing nurses to work effectively in the prison environment. British Journal of Nursing, 8(19), 1324-1326. Hale, J. F., Brewer, A. M., &Ferguson, W. (2008). Correctional health primary care: research and educational oppurtunities. Journal of Correctional Health Care, 14(4), 278-289. Howerton, A., Byng, R., Campbell, J., Hess, D., Owens, C., & Aitken, P. (January 2007). Understanding help seeking behavior among male offenders: qualitative interview study. Bmj. Retrieved March 22, 2008 from BMJ Web site: bmj.com. Imai, K. (2006). Analysis of CDCR Death Reviews 2006. San Jose, California: California Prison Health Care Receivership Corp. 132 Jacques, P. F. (2004). Cultural competency curriculum: components for inclusion in physician assistant education. Perspective on Physician Assistant Education, 15(2), 102-105. Jessee, S. A., O'Neill, P. N., & Dosch, R. O., (2006). Matching student personality types and learning preferences to teaching methodologies [Electronic version]. Journal of Dental Education, 70(6), 644-651. Kaufman, A., Holbrook, J., Collier, I., Farabaugh, L., Jackson, R., & Johnston, T., (1979). Prison health and medical education. Journal of Medical Education, 54, 925-931. Khaw, F., Stobbart, L., & Murtagh, M. J. (2007). I just keep thinking i haven't got it because i'm not yellow: a qualitative study of the factors that influence the uptake of hepatitis c testing by prisoners [research article]. Retrieved February 18, 2008 from BioMed Central at: http://www.biomedcentral.com/1471-2458/7/98. Lincoln, J. M., Chen, L-H., Mair, J. S., Biermann, P. J., & Baker, S. P. (2006). Inmatemade weapons in prison facilities: assessing the injury risk [Electronic version]. Injury Prevention, 12, 195-198. Retrieved February 20, 2008 from: http://journals.bmj.com/cgi/reprinform. Linder, J. F., & Meyers, F. J. (2007). Palliative care for prison inmates: 'don't let me die in prison' [Electronic version]. Journal of the American Medical Association, 298(8), 894-901. Retrieved March 21, 2008 from: www.jama.com. 133 Loeb, S. J., Steffensmeier, D., & Myco, P. M. (2007). In their own words: older male prisoners' health beliefs and concerns for the future. Geriatric Nursing, 28(5), 319328. Macher, A., Kibble, D., & Wheeler, D. (2006). HIV transmission in correctional facility [Electronic version]. Emerging Infectious Diseases, 12(4), 669-671. Retrieved February 20, 2008 from: www.cdc.gov/eid. MacNeil, J. R., Lobato, M. N., & Moore, M. (2005). An unanswered health disparity: tuberculosis among correctional inmates, 1993 through 2003 [Electronic version]. American Journal of Public Health, 95(10), 1800-1805. Retrieved February 20, 2008 from: https://vpn.lib.ucdavis.edu/sites/,DanaInfo=www.ncbi.nlm.nih.gov+entrez. Magee, C. G., Hult, J. R., Turalba, R., & McMillan, S. (2005). Preventive care for women in prison: a qualitative community health assessment of the papanicolaou test and follow-up treatment at a california state women's prison [Electronic version]. American Journal of Public Health, 95(10), 1712-1717. Retrieved February 20, 2008 from: https://vpn.lib.ucdavis.edu/sites/,DanaInfo=www.ncbi.nlm.nih.gov+entrez. McFarland, M. (2006). Nursing theorists and their work (6th ed.) (A. M. Tomey & M. R. Alligood, Eds.). St. Louis, MO: Mosby Elsevier. QuotationsPage.com. (2007). The quotations page. Message posted to http:// www.quotationspage.com/quotes/Fyodor_Dostoevsky/. 134 Ragan, P. (2003). Integrating self-assessment skills into the curriculum. Perspective on Physician Assistant Education, 14(1), 50-52. Raimer, B. & Stobo, J. D. (2004). Health care delivery in the Texas prison system: the role of academic medicine. Journal of the American Medical Association, 292, 485489. Reimer, G. (2007). Transforming correctional health care through advanced correctional nursing education. Journal of Correctional Health Care, 13(3), 163-169. Sieminska, A., Jassem, E., & Konopa, K. (2006, July 7). Prisoners' attitudes towards cigarette smoking and smoking cessation: a questionnaire study in poland. Bmc Public Health. Retrieved March 22, 2008, from BMC Public Health Web site: http:// www.biomedcentral.com/1471-2458/6/181. Streubert-Speziale, H. J. & Carpenter, D. R. (2007). Qualitative research in nursing (4th ed.). Philadelphia: Lippincott, Williams, & Wilkins. (Original work published 1995). Torre, D. M., Daley, B. J., Sebastian, J. L., & Elnicki, D. M. (2006). Overview of current learning theories for medical educators. The American Journal of Medicine, 119(10), 903-907. Weinbaum, C. M., Sabin, K. M., & Santibanez, S. S. (2005). Hepatitis b, hepatitis c, and hiv in correctional populations: a review of epidemiology and prevention [section 1: vulnerable populations]. Aids Official Journal of the International Aids Society, 19, 41-46. 135 Weiskopf, C. S. (2005). Issues and innovations in nursing practice, nurse's experience of caring for inmate patients. Journal of Advanced Nursing, 49(4), 336-3. 136