Dual Diagnosis
advertisement

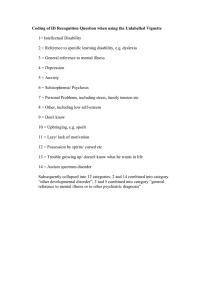
Dual Diagnosis Historically • In the 1970s it was thought that a minority of clients suffered from both a mental illness and an addiction • Today, we know this is not true.... • Today we acknowledge that a majority of our clients suffer from both a mental illness and an addiction • • • Theories of DualDiagnosis Self-medication theory: Substances are selectively used in service of alleviating symptoms of mental illness (i.e. stimulant abuse employed to counter the sedative effects of antipsychotic medications) Alleviation of dysphoria: mental illness creates dysphoria (feeling bad) and this dysphoria leads to drug use to mitigate the experience of these unpleasant feelings Multiple risk: In addition to the alleviation of bad-feelings, there are additional risks such as: social isolation, poverty, lack of daily structure, residing in areas with drug availability, history of traumatic events Theories Continued • • • Supersensitivity: individuals with severe mental illness have biological/psychological vulnerabilities for substance abuse caused by genetic and early environmental factors that interact with life stressors It is important to note that these theories might all be present to varying degree’s in looking at the causal links underlying a dual-diagnosis. There are no definitive quantitative links correlating mental illness/substance abuse apart from heavy adolescent cannabis use and early onset schizophrenia No Universal Agreed Upon Definition • Each disorder is intertwined with the other • Each is able to influence the other (addiction magnifies) • Chicken and Egg as far etiology • Difficult to discern symptoms of one from psychiatric disorder from the addictive disorder • Many psychiatric symptoms omit once addiction is ceased or after a period of abstinence Stigma of the Dually Diagnosed! Likelihood that people with mental illness will commit violent acts No greater than general population! Why worry about it? • Have worse treatment outcomes • Higher health care outcomes • Increased risk of violence, trauma, suicide, child abuse, neglect, involvement with justice system • More prone to helplessness, depression, greater trouble coping Table 22.1 The Overlap Between Substance Use and Disorders and Various Psychiatric Disorders _________________________________________ Lifetime psychiatric Substance use disorder diagnosis Depression Bipolar affective disorder Anxiety disorder Antisocial personality Disorder ADHD Eating disorder Schizophrenia 32% 64% 36% 84% 23% 28% 50% In Canada (Skinner et al. 2004: Concurrent substances use and mental health disorders, 2009, [CAMH]). • 30% of people in Canada with a mental illness will have a substance abuse problem in their lifetime • 37% of people who abuse alcohol in their lifetime will have a mental illness • Meanwhile, 53% who abuse drugs in their lifetime will have a mental illness. Problems in Working with Dual Diagnosis Clients • Fractured support systems • Slow progress • Off and on meds • Significant level of denial • Seeming inability to trust • Collude and transference / idealization / or devalue • Feelings on meds • Field as a whole and turf wars Dual-Diagnosis “Treatment” • • • The term “treatment” is a real set up because it points toward a terminal end-point goal with the dually diagnosed and this, in my experience, is simply not realistic. There are some “approaches” and/or philosophies that have emerged in working with the dual-diagnosed that have varying degrees of efficacy These approaches fall under: Serial Treatment, which treats one condition first followed by the other “Treatment” Continued Parallel: These intervention approaches focus on both substance abuse and mental illness treatment at the same time Integrated: Treatments are delivered at the same time (like the parallel approach) but are coordinated by the same staff team members in the same treatment setting Biological: This is the psychotropic medication arm of treatment and can be effective toward managing symptoms of mental illness which in turn can facilitate treatment of substance misuse “Treatment” Continued • • • • Social and Psychological: This is a broad spectrum term used to describe therapeutic techniques such as: Motivational Interviewing: Engaging in supportive and directed conversation about individuals behaviors and patterns that are designed to increase intrinsic motivation to change Cognitive Behavioral: weakening connections between life stressors and reactive/habitual responses that are negative and destructive. Self-Help Groups: This includes many 12-step groups that can instill peer support and self-discipline Share my experiences /Stories