AN EVALUATION OF FADING PROCEDURES IN THE TREATMENT OF
PEDIATRIC FEEDING DISORDERS: A COMPONENT ANALYSIS
A Thesis
Presented to the faculty of the Department of Psychology
California State University, Sacramento
Submitted in partial satisfaction of
the requirements for the degree of
MASTER OF ARTS
in
Psychology
(Applied Behavior Analysis)
by
Jillian K. LaBrie
FALL
2012
© 2012
Jillian K. LaBrie
ALL RIGHTS RESERVED
ii
AN EVALUATION OF FADING PROCEDURES IN THE TREATMENT OF
PEDIATRIC FEEDING DISORDERS: A COMPONENT ANALYSIS
A Thesis
by
Jillian K. LaBrie
Approved by:
__________________________________, Committee Chair
Dr. Becky Penrod
__________________________________, Second Reader
Dr. Caio Miguel
__________________________________, Third Reader
Dr. Linda Copeland
____________________________
Date
iii
Student: Jillian K. LaBrie
I certify that this student has met the requirements for format contained in the University
format manual, and that this thesis is suitable for shelving in the Library and credit is to
be awarded for the thesis.
__________________________, Graduate Coordinator
Dr. Lisa Harrison
Department of Psychology
iv
___________________
Date
Abstract
of
AN EVALUATION OF FADING PROCEDURES IN THE TREATMENT OF
PEDIATRIC FEEDING DISORDERS: A COMPONENT ANALYSIS
by
Jillian K. LaBrie
In the treatment of food selectivity, packages consisting of multiple components are
typically utilized, often including an escape extinction procedure. Previous research has
demonstrated that these treatment packages are successful in increasing consumption of
target foods, as well as decreasing inappropriate mealtime behaviors. However, due to
initial negative side effects of escape extinction (i.e., an immediate increase in
inappropriate mealtime behaviors), caregivers may be likely implement and/or to adhere
to the procedures. The current study investigated the role of less intrusive interventions
prior to the introduction of escape extinction. Specifically, the current study evaluated
various fading procedures (e.g., texture and liquid fading) using a component analysis by
first introducing fading, then differential reinforcement, and finally escape extinction,
when needed. Results indicated that escape extinction may not be necessary in all cases
v
and contribute evidence to the recommendation to include and/or start with antecedent
based interventions when treating food refusal.
_______________________, Committee Chair
Dr. Becky Penrod
_______________________
Date
vi
ACKNOWLEDGEMENTS
Many people in my life have contributed to where I am today, from childhood to
my undergraduate and post-graduate education. I would like to give special thanks to my
advisors, cohort, friends, and finally my family. Dr. Becky Penrod, you are a remarkable
person, clinician, and advisor/mentor; I am privileged to have had the opportunity to
work with and learn so much from you, both academically and professionally. Dr. Caio
Miguel, you provided me with wonderful experiences that I would have never had the
opportunity to be a part of it weren’t for you. Thank you both so much for all you have
done for me academically, professionally, and personally.
Next, I would like to acknowledge my amazing cohort, Jonathan Fernand,
Kathryn Lee, and Michelle Sutherland. Learning from and working with all of you has
been a priceless experience that I will cherish for the rest of my life. I would also like to
thank the individuals who I had the pleasure of learning from and consequently shaped
my love for behavior analysis as an undergraduate at the University of Nevada, Reno,
most notably, Molly Day Dubuque and Jillian DeFreitas. In addition, I could not have
completed this project without the help of Krista Bolton and support from my other
colleagues at Sacramento State.
Lastly, I would not be here if it were not for the support of my family. Thank
you, mom for always encouraging my education, both formally and informally, as well as
supporting me even when we didn’t see eye to eye. To my husband, Brian Lewis, thank
you for always having faith in my goals and supporting me during the toughest times.
vii
TABLE OF CONTENTS
Page
Acknowledgements .................................................................................................... vii
List of Tables .............................................................................................................. ix
List of Figures ............................................................................................................... x
Chapter
1. INTRODUCTION ..............................................................................................… 1
Stimulus Fading Procedures ............................................................................. 4
Stimulus Fading in the Treatment of Feeding Disorders ................................. 6
Demand Fading ..................................................................................... 7
Simultaneous Presentation with Fading ................................................ 9
Apparatus and Distance Fading .......................................................... 13
Texture Fading .................................................................................... 14
Summary ......................................................................................................... 16
Purpose of the Study ....................................................................................... 16
2. METHOD ............................................................................................................. 18
Participants and Setting................................................................................... 18
Response Measurement and Data Collection ................................................. 19
Interobserver Agreement and Treatment Integrity ......................................... 21
Food Preparation ............................................................................................ 24
Experimental Design ...................................................................................... 27
Assessments .................................................................................................... 27
Procedures ....................................................................................................... 30
3. RESULTS ............................................................................................................. 35
4. DISCUSSION ....................................................................................................... 51
Appendix Data Sheets………………………………………………………………. 61
References................................................................................................................... 64
viii
LIST OF TABLES
Tables
Page
1. Fading steps: Liquid ……… ...........................................………………………… 24
2. Fading steps: Texture ………..……………….… ..............……………………… 25
3. Fading steps: Demand (Bolus size)…...…………….….....……………………… 26
ix
LIST OF FIGURES
Figures
Page
1. Bastion Paired-Choice Preference Assessment (Purees)…………………….....… 36
2. Bastion Pre/Post Paired-Choice Preference Assessment (Final Form)…….…….. 37
3. Vincent Paired-Choice Preference Assessment (Preferred Foods)…………….… 37
4. Vincent Paired-Choice Preference Assessment (Toys #1)……………………….. 38
5. Vincent Reinforcer Assessment (Toys #1)......…………………………………… 39
6. Vincent Paired-Choice Preference Assessment (Toys #2)...................................... 40
7. Vincent Reinforcer Assessment (Toys #2).....……………………………………. 40
8. Bastion Percentage of Bites Consumed without Expulsions……..………………. 43
9. Bastion Percentage of Inappropriate Mealtime Behaviors per session………..…. 45
10. Vincent Percentage of Bites Consumed without Expulsions…………………… 47
11. Vincent Percentage of Inappropriate Mealtime Behaviors per session…………. 50
x
1
Chapter 1
INTRODUCTION
Food selectivity and inappropriate mealtime behaviors have been reported to be
problematic for typically developing children, as well as children with autism spectrum
disorders, developmental disabilities, and intellectual disabilities (Ahearn, Castine, Nault,
& Green, 2001; Bandini, et al., 2010; Gal, Hardal-Nasser, Engel-Yeger, 2011; Schreck,
Williams, Smith, 2004; Volkert & Vaz, 2010; Williams, Gibbons, Schreck, 2005).
Furthermore, children with autism are more likely than typically developing children to
display problems with feeding (restricted intake by type and texture, refuse novel foods)
(Schreck, et al.). It has been reported that up to 25% of typically developing children
(Williams et al.) and 90% of children with autism (Volkert & Vaz) display feeding
difficulties and/or food selectivity. In addition, one study found that 97% of children with
intellectual disabilities that participated exhibited some sort of feeding-related deficit
(e.g., oral motor) and/or food refusal/selectivity (Gal et al.). Moreover, numerous
negative outcomes have been reported for individuals that have been diagnosed with
feeding disorders or who display some type of food refusal behavior. First, individuals,
especially infants and children, who do not consume enough volume or variety of food,
may be at risk for developing preventable health issues and illnesses (Nicklas, 2003;
Reynolds, et al., 1999). Additionally, an individual’s growth and development may be
hindered due to deficient weight gain (Riordan, Iwata, Finney, Wohl, & Stanley, 1984).
Inadequate intake due to a limited variety of foods in an individual’s diet can contribute
2
to a deficiency in essential vitamins and nutrients (Nicklas; Reynolds et al.).
Furthermore, inadequate food intake and nutrition can lead to inhibited brain
development which may be accompanied by learning and academic difficulties (Bryan,
Osendarp, Hughes, Calvaresi, Baghurst, & Van Klinken, 2004; Dykman, Casey,
Ackerman, & McPherson, 2001), and children diagnosed with severe feeding disorders
have a greater chance of being diagnosed with other developmental delays (Ahearn,
Kerwin, Eicher, & Lukens, 2001). Additionally, childhood feeding problems can lead to
disruptive or high stress mealtimes for the family or primary feeder, which can also have
an effect on potential socialization opportunities. A child with challenging mealtime
behavior may not be included in the family meal and instead fed at a different time or in a
different area of the home so as to avoid unpleasant or stressful mealtime situations.
An individual may develop food selectivity in regards to one or many different
physical or sensory properties of food or the mealtime environment. Food selectivity
may develop due to a negative experience, physiological abnormalities (e.g., cleft palate
and swallowing difficulties), physical/developmental disabilities (e.g., cerebral palsy and
autism) and/or other underlying medical conditions. Some possible events, which may
contribute to food aversions, include choking, gagging, vomiting, indigestion, or other
uncomfortable physiological events. The properties of the item to which the child has
developed an aversion may also generalize to other food items that share similar physical
(e.g., size and color) or sensory (e.g., olfactory, gustatory, and tactile) characteristics of
the original item. An individual may display selectivity by type, texture, color, brand,
and/or taste. In addition, the presentation of food such as shape (e.g., how the food is cut)
3
or temperature, as well as the location of the meal and eating utensils (e.g., spoon, plates,
etc.) can play a role in an individual’s food selectivity and inappropriate mealtime
behaviors.
There is a broad range of feeding difficulties that can be categorized as food
selectivity by type, such as refusal to eat items from particular food groups (e.g.,
vegetables), only consuming snack or junk foods, and refusal to consume liquids (i.e.,
total liquid refusal or liquid selectivity). Food selectivity of any kind can lead to harmful
nutritional and developmental consequences. For instance, if a child does not consume a
sufficient amount of liquids it could lead to dehydration. Another type of feeding
difficulty of concern is food selectivity by texture. An individual that displays selectivity
by texture may only consume food in a puree form and the variety of food types in their
repertoire may be limited. In this example, if a child does not have the opportunity to
advance to age-appropriate textures, they may run the risk of underdeveloped oral motor
skills (Southall & Martin, 2010) and potentially low muscle tone that could contribute to
poor caloric intake. In addition to these health concerns, there may be negative social
consequences associated with various forms of food selectivity. For instance, an
individual that displays selectivity by texture may be isolated or teased by peers for
eating food not typically presented in a puree form. Children with feeding disorders may
stand out from their peers by not participating in events with peers (e.g., birthday parties)
because they don’t eat the same foods as their peers (e.g., birthday cake, pizza, hotdogs,
etc.). These children may stand out more by bringing their own food to peer-related or
other events because of refusal to try new things and/or a limited food repertoire. In
4
summary, feeding problems, particularly food selectivity, can result in deleterious effects
upon the individual by contributing to potential oral motor delays, nutritional and
developmental deficiencies, as well as impeding socialization opportunities.
Stimulus Fading Procedures
Previous studies have demonstrated the effective use of fading procedures in the
reduction of behavior excesses that interfere with an individual’s daily functioning, as
well as increasing skills that would otherwise restrict an individual from participation in
certain activities that are beneficial to their survival or wellbeing (e.g., Shabani & Fisher,
2006). For instance, fear or aversions to preventative or necessary medical procedures or
simply visiting a doctor can have detrimental consequences for an individual.
Additionally, and even more relevant to this study, are challenging behaviors associated
with feeding disorders.
Antecedent interventions, such as stimulus fading, can be used to eliminate or
minimize the motivating operation for negatively reinforced behavior by altering the
value of escape as a reinforcer (Michael, 1982, 1993; Zarcone, Iwata, Smith, Mazaleski,
& Lerman, 1994). Stimulus fading can be used in an effort to reduce inappropriate
behaviors, as well as facilitate acquisition of new responses (e.g., McCord, Iwata,
Galensky, Ellingson, & Thomson, 2001; Ringdahl, Kitsukawa, Andelman, Call,
Winborn, Barretto, & Reed, 2002; Zarcone et al., 1994). In particular, one variation of
stimulus fading, known as demand fading, has been attributed to an immediate reduction
of maladaptive behaviors (e.g., self-injurious behavior) maintained by negative
reinforcement in the form of escape from instructional demands while remediating the
5
effects of an extinction burst when used in conjunction with escape extinction (EE), as
opposed to EE without the use of demand fading for two of three participants (Zarcone,
Iwata, Vollmer, Jagtiani, Smith, & Mazaleski, 1993).
Previous research has demonstrated the utility of implementing a stimulus fading
procedure for behaviors maintained by negative reinforcement (McCord et al., 2001;
Reitman & Passeri, 2008; Ringdahl et al., 2002; Shabani & Fisher, 2006). Specifically,
Shabani and Fisher used a stimulus fading procedure combined with differential
reinforcement of other behaviors for an adolescent with autism who had a needle phobia.
It was necessary for the participant to learn to accept blood being drawn in order to
manage his diabetes and specifically monitor his glucose levels. Shabani and Fisher used
stimulus fading in order to decrease behaviors maintained by negative reinforcement
(e.g., crying, screaming, elopement, self-injury, aggression, and pulling away from the
needle) when in the presence of needles. For this study, the initial criterion was set based
on the participant not displaying any of the target problem behaviors when the proximity
of the needle was a certain distance from his hand. This initial criterion was used to
ensure the participant would come into contact with the reinforcement contingency.
During each phase, the distance of the needle from the participant’s hand was gradually
decreased following two or three sessions without the participant’s hand moving more
than 3cm in a 10-s trial. Follow-up data taken two months later demonstrated that results
of the intervention were maintained.
In another study, Reitman and Passeri (2008) taught a child diagnosed with
Attention Deficit Hyperactivity Disorder to swallow a pill by using a fading procedure in
6
which the size of pieces of candy to be swallowed was systematically increased and
eventually the child’s medication (Ritalin) was targeted. The treatment package included
modeling, differential reinforcement using tangible items, and stimulus fading. EE was
not necessary and there was a 50 min session cap for all phases of treatment. The
participant met terminal criterion within 15 sessions (approximately 100 trials), and
responding was maintained at both 3- and 12-month follow-up sessions. Reitman and
Passeri were successful in demonstrating the effectiveness of stimulus fading without the
use of an EE procedure. Even though EE was not necessary for acquisition of the target
response, stimulus fading was used as part of a treatment package consisting of
differential reinforcement and modeling which does not allow for conclusions to be
drawn about the contribution of the fading procedure if implemented alone.
Stimulus Fading in the Treatment of Feeding Disorders
Many studies have demonstrated the efficacy of implementing fading procedures
for individuals who demonstrate food selectivity (e.g., Luiselli, Ricciardi, & Gilligan,
2005; Tiger & Hanley, 2006); however, it should be noted that fading procedures are
often used as one component of treatment packages consisting of various behavioral
strategies such as reinforcement, chaining, and EE (e.g., Freeman & Piazza, 1998;
Hagopian, Farrell, & Amari, 1996).
Within-stimulus fading is a strategy that has been effective for remediating the
negative outcomes of acquired food aversion. Within-stimulus fading procedures involve
altering some dimension of the target item or stimulus (e.g., texture, taste, size, color,
shape, amount, etc.) to facilitate acquisition of a desired response (Miltenberger, 2012).
7
Within-stimulus fading procedures focus on the same target response during each
learning opportunity while the physical properties of the associated stimuli progressively
change as mastery occurs. Moreover, when stimulus fading is used, responses or skills
that have been observed to occur in the past are targeted and then the response
requirement is gradually increased as the individual meets criterion with the previous
response requirements. Programming for acquisition in this manner can reduce the
likelihood of errors and thereby reduce the likelihood of negative emotional responses or
inappropriate behaviors (e.g., Shabani & Fisher, 2006).
Research has shown that behavior analytic interventions including fading
components are effective in addressing feeding problems (e.g., Luiselli, 2000; Sharp &
Jaquess, 2009; Tiger & Hanley, 2006). Fading can be advantageous in addressing
feeding problems by gradually exposing and changing relevant antecedent stimuli in
order to decrease problem behaviors and make the events, stimuli, or activities associated
with eating less aversive. Methods of stimulus fading can be applied in many different
ways for the treatment of feeding disorders. Specifically, various fading procedures can
be described as demand fading (bite size or number of bites), apparatus fading, distance
fading, texture fading, and simultaneous presentation with fading. The aforementioned
list of fading procedures is not exhaustive and other variations or combinations could be
utilized. Some variations of fading procedures are outlined below.
Demand Fading
Demand fading or instructional fading, also known as bite fading within the
feeding literature, has been shown to be an effective procedure for increasing
8
consumption of liquids and solids for individuals that display food selectivity and refusal
(e.g., Freeman & Piazza, 1998; Galensky, Miltenberger, Stricker, Garlinghouse, 2001;
Valdimassdottir, Halldorsdottir, & Sigurdardottir, 2010). When demand fading is
implemented, the initial response requirement is small and attainable so as to increase the
likelihood of the individual coming into contact with the predetermined reinforcement
contingency (e.g., termination of the activity, presentation of preferred items, etc.). Once
the behavior is reliably occurring at the minimum response requirement, the frequency of
instructions, or in the case of feeding interventions, the number of bites or amount of
fluid that is required to be consumed is progressively increased in order for the individual
to access reinforcement.
For instance, Hagopian et al., (1996) used backward chaining and fading as an
intervention for total liquid refusal. Backward chaining and fading components were
implemented concurrently such that as success was demonstrated with chained responses
and the response requirement was increased, the volume of liquid intake was also
increased. For this study, backward chaining consisted of three main steps:
1) swallowing, 2) accepting water into the mouth, and 3) bringing the cup of water to the
mouth. Reinforcement was first contacted when the participant swallowed without the
presentation of water or a drinking apparatus, then reinforcement was provided when a
swallow occurred following the presentation of an empty syringe into the participant’s
mouth. Once the participant was consistently accepting and swallowing small amounts
of water with a syringe, the volume of liquid was systematically increased along with the
introduction of a cup as the final drinking apparatus. Hagopian et al. demonstrated that
9
fading without EE might be successful for treating liquid refusal; however, since a
backward chaining procedure was also used, the contribution of the fading procedure is
not entirely clear.
As another example, Freeman and Piazza (1998) demonstrated the efficacy of a
treatment package consisting of bite fading, reinforcement, and EE in increasing
consumption of non-preferred foods for a girl with autism and other diagnoses. Similarly,
Valdimassdottir et al. (2010) were successful in expanding the food repertoire for a child
diagnosed with autism that displayed food selectivity by implementing bite fading and
reinforcer thinning with EE across two caregivers and settings. Additionally, demand
fading combined with reinforcement has been shown to be effective in establishing selffeeding and oral consumption, as well as expanding the number of foods consumed, for a
typically developing young boy that was G-tube dependent (Luiselli, 2000). In summary,
previous studies have demonstrated the efficacy of demand fading used in conjunction
with various behavioral strategies, but further research is needed to determine the
individual effects of common procedures (e.g., fading, reinforcement, and extinction)
used in the treatment of pediatric feeding disorders. Treatment for individuals may vary
in that some cases require more comprehensive interventions while others will necessitate
fewer or less intrusive interventions.
Simultaneous Presentation with Fading
Simultaneous presentation of foods or liquids, with demand fading, has been
shown to be an effective treatment for individuals with feeding problems (Luiselli et al.,
2005; Mueller, Piazza, Patel, Kelley, & Pruett, 2004; Patel, Piazza, Kelly, Ochsner,
10
&Santana, 2001; Tiger & Hanley, 2006). Liquid and food blending used in the treatment
of feeding disorders involves increasing consumption of liquids or food through mixing
preferred and non-preferred items or flavors and gradually increasing the amount of
liquids or food that have previously been refused when presented by themselves.
In a study conducted by Patel et al. (2001) a treatment package consisting of
fading with differential reinforcement of alternative behavior (DRA) and EE was used to
increase fluid consumption for one individual. The participant initially refused milk with
Carnation Instant Breakfast (CIB) and water with CIB, but would consume water by
itself. The fading procedure started by slowly introducing CIB mix into water; then, after
the participant was successfully drinking the water mixture with the entire package of
CIB, water was gradually replaced by milk until the solution consisted of only milk and a
whole packet of CIB. Patel et al. were successful in establishing acceptance of CIB
mixed with milk; however, the effect was only demonstrated with one participant.
Similarly, Luiselli et al. (2005) examined the effectiveness of fading alone to
increase the variety of liquids consumed for a girl diagnosed with autism. Prior to
treatment, the participant would independently drink a mixture of 50/50 Pediasure to
milk ratio and refused to consume milk when not mixed with Pediasure (i.e., refused
the presentation of 100% milk). Luiselli et al. increased the milk to Pediasure ratio by
adding approximately 6.3% more milk for each fading step. Baseline and treatment
conditions both included an instruction to take a drink when a 60-s lapse in consumption
occurred and praise was provided contingent upon consumption of the target mixture.
11
Fading alone could have been the contributing variable to the observed success given that
conditions remained constant from baseline to treatment and there was no increase in
consumption of the 100% milk beverage during baseline conditions. On the other hand,
praise may have served as positive reinforcement for liquid consumption or negative
reinforcement by the termination of the instruction may have played a role in treatment
outcomes. However, given that periodic probes were conducted with 100% milk
throughout the fading steps and consumption of the terminal target beverage did not
occur until the final stages of fading, it is likely that fading without the use of EE was a
contributing factor to an increase in milk consumption.
Furthermore, Tiger and Hanley (2006) used stimulus fading, in addition to
reinforcer pairing, in order to establish milk drinking for a typically developing
preschooler. Chocolate syrup, which was reported to be highly preferred, was used as an
antecedent intervention by mixing the syrup with milk and then eventually fading out the
chocolate syrup completely. Success was demonstrated across settings (i.e., preschool
and home), as well as across caregivers (i.e., preschool teacher and parents). Milk
consumption without the use of chocolate was increased to criterion during treatment;
however, plain milk consumption was not maintained at very high levels. The participant
did continue to consume plain milk following the study, but the amount decreased from
treatment. Even though milk consumption was not maintained for the recommended
nutritional percentages, it was increased significantly without the use of EE compared to
consumption prior to treatment.
12
Previous research has also demonstrated the effectiveness of food blending and
fading in conjunction with reinforcement (i.e., DRA or non-contingent reinforcement)
and EE (Mueller et al. 2004). Mueller et al. blended preferred and non- preferred foods
together as a puree and the volume of non-preferred food was increased by about 10% as
participants met criterion for the previous fading step. Consumption increased for the
target foods across both participants following the implementation of the treatment
package. Both participants had a prior feeding intervention, which consisted of
reinforcement and EE; the previous intervention was successful in increasing
consumption of some but not all foods. When the blending and fading procedure was
added to the treatment package the variety of foods consumed for the participants was
expanded even further. These researchers discussed possible mechanisms responsible for
the increase in variety of foods consumed such as the altering of motivating operations or
effects of flavor-flavor conditioning. First, the presentation of preferred foods may have
reduced the aversive properties of the non-preferred foods and decreased the
effectiveness of escape as reinforcement (Michael, 1982, 1993). On the other hand,
pairing of sweet tasting preferred foods with non-preferred foods may have facilitated the
increase in consumption of non-preferred foods through the process of flavor-flavor
conditioning (Zellner, Rozin, Aron, & Kulish, 1983). However, because the treatment
package also utilized a DRA and EE procedure, it is difficult to parse out the utility of the
fading procedure.
13
Apparatus and Distance Fading
Apparatus fading and distance fading have also been demonstrated as effective
treatments for food/liquid refusal and selectivity. For instance, Babbit, Shore, Smith,
Williams, and Coe (2001) used apparatus fading and EE to treat children who would
consume solids but refused liquids. They used a spoon to cup fading procedure and
provided preferred edibles contingent on meeting the response requirement (i.e.,
consumption of liquids) within a given phase. Participants began by receiving liquids on
a spoon with a cup attached to the handle (farthest away from the head of the spoon)
which was gradually moved closer to the head of the spoon until participants were
drinking from the cup with the spoon no longer attached. The fading procedure, in
conjunction with EE, was effective in increasing cup drinking for both participants in the
study.
A study conducted by Rivas, Piazza, Patel, and Bachmeyer (2010) examined
spoon distance fading with and without EE, as well as EE alone. They found that
distance fading alone was somewhat effective. Distance fading was effective until the
distance of the spoon from the participant’s lips was reduced and a reemergence of
inappropriate mealtime behaviors occurred. Fading with EE was successful in increasing
acceptance, however, when compared with EE alone, fading with EE resulted in slower
progress and more trials to criterion. On the other hand, when fading was combined with
EE a reduction in inappropriate mealtime behaviors was observed immediately, as
opposed to an extinction burst that occurred when EE was implemented in isolation.
Rivas et al. demonstrated that multiple factors contribute to what type of treatment will
14
be best for different individuals and their families. For instance, if a caregiver objects to
the use of a treatment that may evoke more problematic behaviors, it may be best to
recommend the use of a treatment package consisting of a fading procedure.
Alternatively, if rapid results are the primary concern of caregivers and/or medical
professionals, then a function-based procedure without the use of fading could be the best
option.
Texture Fading
Texture fading is used to aid children in advancing from pureed or blended food
to solid table foods or more age-appropriate textures. Texture fading has been
implemented as part of treatment packages for food selectivity (Patel, Piazza, Santana,
&Volkert, 2002; Sharp & Jaquess, 2009; Shore, Babbitt, Williams, Coe, & Snyder, 1998)
and packing (Patel, Piazza, Layer, Coleman, & Swartzwelder, 2005). For instance, Shore
et al. (1998) evaluated a treatment package that consisted of texture fading,
reinforcement, and EE. The primary steps in the fading procedure were as follows: 100%
pureed, 100% junior, 100% ground, and 100% chopped fine, while some intermediate
textures were introduced for a couple of the participants. The treatment package used in
this study was successful in the treatment of food selectivity with all 4 children. That is,
by the end of the study all participants were consuming age-appropriate textures and
volume. Shore et al. discussed that in the absence of the fading component, the
reinforcement and extinction contingencies could have together contributed to results
observed for the participants. Thus, similar results may have been obtained without the
addition of the fading component in treatment. Nonetheless, fading was the likely
15
component responsible in reducing the amount of gags emitted by the participants given
that gagging was frequently observed when a higher texture was introduced without the
use of intermediate textures (e.g., going from puree immediately to chopped). In
addition, expulsions decreased for participants who initially displayed them prior to this
study. By using fading and gradually introducing more dense textures, participants may
have had more opportunities to learn the skills needed to control food within their mouth
than if there was an abrupt change in the type of food. Due to the incorporation of
differential reinforcement and EE, the contribution of the fading component could not be
clearly established.
In another study, Sharp and Jaquess (2009) found that a treatment package
consisting of EE, texture and bite fading, and non-contingent access to preferred items,
was effective in increasing the variety of foods consumed by a child diagnosed with
autism; however, the participant in this study still displayed deficits in eating appropriate
volumes and higher texture foods. EE was used to expand his variety by moving from
only consuming Pediasure presented by a syringe to consuming multiple pureed foods.
This participant was advanced to a wet ground texture during this treatment but not
beyond (i.e., the participant did not consume chopped texture as targeted for the terminal
criteria). There were high rates of gagging and refusal behaviors when ground texture
was introduced and the researchers went back to the wet ground. This may have been
due to inadequate oral motor skills. The researchers did state that they later increased to
ground by using smaller increments; however those data were not reported. Once again,
16
given that EE, as well as non-contingent reinforcement (NCR) were included treatment
components, the role of fading is not entirely clear.
Summary
The above findings have all demonstrated that fading procedures in the treatment
of feeding disorders are effective when combine with other treatment components. In an
effort to evaluate antecedent interventions in the treatment of food selectivity due to
consumer and professional concern many studies include antecedent components.
However, caregivers and other professionals are still apprehensive in the use of EE even
with the combination of antecedent procedures. Thus, it is necessary for the field to
evaluate all possible combinations of treatment procedures, both as packages and as
individual treatments.
Purpose of the Study
The present study aimed to evaluate various fading procedures without the use of
additional treatment components in an effort to expand the variety of foods or liquids
consumed by participants, by progressively increasing the amount of non-preferred foods
or liquids in their repertoire. It was presumed that fading procedures would decrease the
motivation to engage in food refusal behaviors when participants were presented with
non-preferred items. In many of the studies described previously, the contribution of the
fading component could not be clearly established because each of the treatment
packages utilized an EE procedure, which is known to increase consumption and
decrease problematic mealtime behaviors (e.g., Ahearn, 2002). The current study aimed
to replicate and extend the aforementioned studies on food selectivity by evaluating
17
fading procedures in the absence of other treatment components (e.g., backward
chaining) and without the initial introduction of differential reinforcement and EE.
Procedures similar to other research evaluating fading as a component of interventions
for individuals with feeding disorders (e.g., Luiselli et al.,2005; Mueller et al. 2004; Patel
et al., 2001; Shore et al., 1998) were replicated; however, this study used a sequential
introduction of treatment components by first introducing fading, then DRA, and finally
EE when necessary. The order of treatment components were introduced in a least to
most intrusive fashion.
18
Chapter 2
METHOD
Participants and Setting
Participants included 2 young boys, Bastion 4-years 3-months and Vincent 4years 7-months, both diagnosed with an autism spectrum disorder and who exhibited
problems with feeding (i.e., food and/or liquid selectivity). Specifically, participants
were selected based upon their inadequate consumption of an age-appropriate variety of
food, display of problematic behaviors during mealtime (e.g., crying, disruption,
tantrums, aggression, self-injury, etc.), and particular to Bastion, the consumption of
atypical foods for his age (i.e., only liquid/puree). At the beginning of and throughout the
study participants were not diagnosed with any feeding related medical conditions such
as failure to thrive, and there were no medical concerns regarding their current weight.
The study was conducted at the Pediatric Behavior Research Lab at California State
University, Sacramento. Participants sat in a high-chair during all feeding sessions.
Prior to the study, Bastion only consumed a specifically prepared sweet tasting
liquid/puree mixture (with various items such as spinach, almond milk, apples, bananas)
from a bottle. Before participation in this study, Bastion had not received treatment
addressing his feeding problems besides an unsuccessful attempt to introduce cup
drinking by his private early intensive behavior treatment provider. Following a
procedure consisting of NCR and physical guidance to increase independent feeding
skills (i.e., eating from a spoon) with the main researcher, Bastion would eat a thickened
19
version (more consistent with a puree texture as opposed to liquid) of the preferred
mixture from a spoon, independently. Per parent report, before Bastion became even
more selective, he previously ate pureed bananas, apple sauce, and yogurt. Bastion
refused stage 3 baby foods when his mother tried to transition away from purees.
Following spoon training, Bastion’s mother was able to reintroduce pureed baby food
(Gerber jarred); however, Bastion continued to refuse any novel food of other textures or
different textures of preferred flavors. Thus, prior to treatment, Bastion was eating seven
types of pureed jar food (e.g., sweet potatoes, bananas, and pasta primavera), as well as
peach and banana-strawberry yogurt; however, he did not consume any solid/table-top
textures.
Previous to participating in this study, Vincent independently ate solid foods;
however, the variety and nutritional content was severely limited. His food repertoire
consisted of cheeseburgers from 3 specific fast-food restaurants, macaroni and cheese
from a specific restaurant, French fries from fast food restaurants, and some crunchy
snack foods (e.g., goldfish and pretzels). In addition, Vincent drank water regularly and
from any cup. Vincent had a history of discontinuing consumption of foods that were
previously consumed (e.g., pancakes, Pediasure, spaghetti, yogurt, apple sauce, and
fried rice).
Response Measurement and Data Collection
Data were taken on accepts, expulsions, gags, and whether the bite was consumed
(measured by mouth clean checks) per trial. An acceptance was defined as an entire bite
placed in the child’s mouth which completely passed the plane of the lips. Expulsions
20
were defined as a whole bite of food, which was previously accepted, leaving the plane of
the child’s lips. A swallow or mouth clean was defined as the child’s mouth containing a
piece of food no larger than the size of a pea, given that expulsion did not occur. The
experimenter conducted mouth clean checks 15-s after the bite was placed in the
participant’s mouth and thereafter every 10-s if the participant did not swallow the food
or refused to open their mouth.
Instances of inappropriate mealtime behaviors were collected on a trial-by-trial
basis. Inappropriate mealtime behaviors were divided into groups depending on the
topography of each participant’s problematic behaviors, which included aggression (e.g.,
biting and hitting), negative vocalizations (e.g., screaming), disruptive behaviors (e.g.,
pushing the spoon/experimenter’s hand away and crushing the cup), self-injury (e.g.,
biting any part of his body), and biting objects (e.g., the back of the high chair), for
Vincent. Bastion engaged in two topographies of refusal behaviors, negative
vocalizations (e.g., crying) and disruption (e.g., pushing the spoon away). For each trial,
when any of the behaviors within a certain group were observed, it was recorded as one
instance. The exact frequency of inappropriate behaviors were not counted, only whether
or not any behaviors within a group occurred during the trial. All responses were
recorded using pen/pencil and paper with data sheets specifically prepared for this study
(see Appendix).
Data were reported as percentage of bites consumed without expulsion for each
10 trial session. Data were taken per trial across four topographies which included:
accept, expulsion, gag, and whether a swallow occurred (i.e., mouth clean). Percentage
21
occurrence for the dependent variable was calculated by dividing the total number of
bites consumed without expulsions by the total number of trials (i.e., 10) and then
multiplying by 100. In addition, the percentage of trials with inappropriate mealtime
behavior was obtained by using the same formula.
Interobserver Agreement and Treatment Integrity
Interobserver agreement data were collected across treatment components, as well
as fading steps throughout the study with a second observer present during the session or
via video recording. A second independent observer collected data on all dependent
measures and interobserver agreement was calculated for accepts, expulsions, mouth
cleans, gags and inappropriate mealtime behaviors. Data were collected by a second
observer during 82% of banana sessions and 70% of sweet potato sessions for Bastion, as
well as recorded during 67% of Pediasure sessions and 46% of rice sessions for
Vincent. Interobserver agreement for measures related to consumption (e.g., accepts,
mouth cleans, etc) and inappropriate mealtime behaviors was calculated using the pointby-point agreement method. That is, each trial must have been scored by both observers
marking either a plus or minus for each dependent variable in order for that trial to be
scored as an agreement. A percentage for interobserver agreement was obtained by
dividing the total number of agreements for each dependent measure by the total number
of trials per session (i.e., 10) and multiplied by 100. Interobserver agreement for
acceptance, expulsion, mouth clean, and gagging was 100% during banana and sweet
potato sessions for Bastion with one exception for gagging during sweet potato sessions
which resulted in 99.79% (range 90-100%) agreement. Interobserver agreement for
22
inappropriate mealtime behaviors during Bastion’s banana and sweet potato sessions
were 97.69% (range 70-100%) and 97.45% (range 70-100%) for negative vocalizations,
respectively, and 99.85% (range 90-100%) and 99.79% (90-100%) for disruptions,
respectively. Interobserver agreement for acceptance, expulsion, and gagging was 100%
during all sessions (i.e., Pediasure and rice) for Vincent. In addition, interobserver
agreement for mouth clean was 99.72% (range 90-100%) for Pediasure and 100% for
rice. Interobserver agreement data for all topographies of inappropriate mealtime
behaviors, excluding negative vocalizations and disruption, during Vincent’s sessions
was 100%. During Pediasure sessions, interobserver agreement was 98.82% (range 80100%) for negative vocalizations and 99.19% (range 90-100) for disruptions; during rice
sessions, interobserver agreement was 97.33% (range 80-100%) for negative
vocalizations and 100% for disruptions.
Researchers gathered treatment integrity data across varying treatment
components (i.e., baseline, fading, and DRA) during the course of the study. Treatment
integrity was evaluated for bite presentation (i.e., pre-scooped and placed in front of the
participant), prompting, termination of trials for expulsions and refusal behaviors, mouth
clean checks, and consequences for swallows (i.e., praise only during fading and praise
plus delivery of item during DRA). For Bastion, data were gathered during 63% of
banana sessions and 51% of sweet potato sessions. Treatment integrity during Bastion’s
sessions was 100% for both foods with a few exceptions. For instance, mouth clean
checks were implemented with 99.80% (range 90-100%) and 99.41% (range 90-100%)
23
integrity for banana and sweet potato, respectively. Treatment integrity for trial
termination due to refusal behaviors during sweet potato sessions was 99.41% (80100%). Finally, praise was provided with 99.60% (90-100%) and 99.41% (90-100%)
integrity for banana and sweet potato sessions, respectively. For Vincent, data were
collected during 64% of Pediasure sessions and 66% of rice sessions. Treatment
integrity during Vincent’s sessions was 100% for both foods, except for mouth clean
checks during Pediasure which was implemented with 99.41% (range 90-100%)
integrity.
24
Food Preparation
In order to ensure consistency in food preparation, the main researcher prepared
the food during all sessions by referring to predetermined fading criteria and written
directions (see Tables 1-3 below).
Table 1
Fading steps: Liquid
Main and Intermediate Fading Steps Preparation Instructions for Liquid Selectivity
Liquid Fading
(Flavor-Flavor)
Step 1
Preparation Directions
100ml preferred liquid
95ml preferred/5ml non-preferred
Step 2
90ml preferred/10ml non-preferred
Intermediate
85ml preferred/15ml non-preferred
Step 2
80ml preferred liquid/20ml non-preferred liquid
1.
75ml preferred/25ml non-preferred
Step 3
2.
70ml preferred/30ml non-preferred
Intermediate
3.
65ml preferred/35ml non-preferred
Step 3
60ml preferred liquid/40ml non-preferred liquid
1.
55ml preferred/45ml non-preferred
Step 4
2.
50ml preferred/50ml non-preferred
Intermediate
3.
45ml preferred/55ml non-preferred
Step 4
40ml preferred liquid/60ml non-preferred liquid
1.
35ml preferred/65ml non-preferred
Step 5
2.
30ml preferred/70ml non-preferred
Intermediate
3.
25ml preferred/75ml non-preferred
Step 5
10ml preferred liquid/80ml non-preferred liquid
1.
15ml preferred/ 85ml non-preferred
Step 6
2.
10ml preferred/ 90ml non-preferred
Intermediate
3.
5ml preferred/ 95ml non-preferred
Step 6
100ml non-preferred liquid
Note: Target items used for Vincent with this fading sequence (liquid blending) were
1.
2.
3.
Pediasure (non-preferred) and water (preferred).
25
Table 2
Fading steps: Texture
Main and Intermediate Fading Steps Preparation Instructions for Texture Selectivity
Texture Fading
Step 1
Puree
Step 2
Intermediate
Step 2
Wet Ground
Step 3
Intermediate
Step 3
Ground
Step 4
Intermediate
Step 4
Finely Chopped
Step 5
Intermediate
Preparation Directions
Puree: Equal parts water and food item blended in a blender until
smooth (also, pre-packaged/jarred).
1.
90g puree/15ml water & 30g ground size
2.
60g puree/30ml water & 60g ground size
3.
30g puree/45ml water & 90g ground size
Cut with an electric food chopper into pieces the size of a ½
grain of rice and combined with 15 ml water per 30g of food
1.
11.25ml water/30g ground size
2.
7.5ml water/30g ground size
3.
3.75ml water/30g ground size
Cut with an electric food chopper into pieces the size of ½ grain
of rice
1.
75g ground/25g finely chopped
2.
50g ground/50g finely chopped
3.
25g ground/75g finely chopped
Less than ¼ inch with food chopper or sharp knife (extra small
piece)
1.
75g finely chopped /25g chopped
2.
50g finely chopped/50g chopped
3.
25g finely chopped /75g chopped
Step 5
Chopped
About ½ inch by ¼ inch with natural thickness (small piece)
¼ of final size
½ of final size
¾ of final size
Step 6 (final)
About 1 inch by 1 inch with ¼ inch slice or natural thickness
Table Top
(large piece or typical presentation)
Note: Target foods used for Bastion with this fading sequence were banana and sweet
Step 6
Intermediate
1.
2.
3.
potato (preferred as puree form).
26
Table 3
Fading steps: Demand (Bolus size)
Main and Intermediate Fading Steps Preparation Instructions for General Selectivity
Demand Fading
(Bolus Size)
Preparation Directions
½ piece
1 piece
2 pieces
Step 1
3 pieces
1.
4 pieces
Step 2
2.
5 pieces
Intermediate
3.
6 pieces
Step 2
7 pieces
1.
8 pieces
Step 3
2.
9 pieces
Intermediate
3.
10 pieces
Step 3
11 pieces
1.
12 pieces
Step 4
2.
13 pieces
Intermediate
3.
14 pieces
Step 4
15 pieces
1.
16 pieces
Step 5
2.
17 pieces
Intermediate
3.
18 pieces
Step 5
19 pieces
1.
20 pieces
Step 6
2.
21 pieces
Intermediate
3.
22 pieces
Step 6
23 pieces
Note: This fading sequence is used when introducing new and/or non-preferred foods by
Step 1
Intermediate
1.
2.
3.
themselves (i.e., without blending). Target food used for Vincent with this fading
sequence was rice (non-preferred).
27
Experimental Design
A multiple probe design across foods with probes prior to the introduction of a
new fading step was utilized to demonstrate experimental control and control for
additional, unnecessary exposure to the target food introduced in the second tier of the
design. The intervention in each baseline/tier was introduced in a staggered fashion and
was introduced when responding in each baseline was stable. Probes were introduced for
the next fading step and final target food/liquid prior to moving to the next step in the
fading procedure. When probes were required for the first targeted food, prior to the
introduction of the second food into treatment, probes were also conducted for the second
tier food. In addition, probes and sessions for each tier food were conducted in a
concurrent fashion. Each treatment component was introduced in a sequential fashion:
first fading with praise only, then fading plus DRA (praise and tangible or edible), and
finally, fading plus DRA and EE (however, EE was not needed for either participant in
this study).
Assessments
For the current study, food items that were preferred or consumed prior to
participation in research were used as the initial fading step for Bastion (both tier 1 and 2
foods) and Vincent (tier 1 food only) in order to better ensure consumption, lower the
chance for the occurrence of maladaptive behaviors, and facilitate success during
conditions that did not involve a DRA or EE component. Preferred food items were used
because participants were expected to self-feed and no physical prompts (with the
exception of Vincent who required assistance with spoon-feeding as to not spill the
28
liquid) or EE were implemented during the first two treatment components. In order to
determine preferred foods to be targeted for treatment, paired-choice preference
assessments were conducted prior to starting treatment, using procedures described by
Fisher, Piazza, Bowman, Hagopian, Owens, and Slevin (1992). Paired-choice preference
assessments included foods or liquids that the child consumed prior to the start of the
study. The foods used in the study were selected based upon consumption during the
preference assessment, as well as parent priority, and ease of use with a fading
(specifically, food blending) procedure.
In addition, a pre and post paired-choice preference assessment (Fisher et al.,
1992) was used for one participant to evaluate consumption of the final target foods or
liquids. This assessment was used in order to demonstrate whether following treatment
implemented with two non-preferred foods, results would generalize to foods not targeted
during treatment. Foods that were targeted during treatment were included in the prepost assessment, as well as foods not targeted during treatment.
Lastly, in order to determine appropriate items to be used during the DRA
component, a third paired-choice preference assessment (Fisher et al., 1992) was
completed prior to the introduction of differential reinforcement for the participants who
necessitated the DRA component (i.e., Vincent). This assessment included tangible items
that were identified by parents as being highly preferred. For the top three items
identified as preferred from this preference assessment, a reinforcer assessment was
conducted to determine if the items functioned as reinforcement for Vincent’s behavior.
The response used for Vincent during the first reinforcer assessment (when DRA was
29
determined to be necessary for Pediasure) was drinking water from a cup (a skill he
demonstrated on his own terms, however, inconsistent consumption of water was
observed during treatment sessions) and when the DRA component was added to the
treatment package addressing the refusal of rice, a second reinforcer assessment was
conducted where the response of drinking Pediasure was evaluated. A progressive ratio
schedule was used to identify the breaking point for each preferred item similar to the
procedures described by Roane, Lerman, and Vorndran (2001). That is, the response
requirement increased by one as the previous requirement was met. In order to control
for ratio strain during the reinforcer assessment, each progressive ratio schedule was
implemented twice before increasing the reinforcement schedule. When the participant
stopped responding for three consecutive minutes, the reinforcer assessment for that item
was terminated. For Vincent, three items were identified and used as reinforcement
during the first tier food (i.e., Pediasure) during the implementation of the DRA
treatment component. Items included a caterpillar game, shooting ice-cream cone, and a
sound train puzzle. The three new items that were identified via preference and
reinforcer assessments to use for the DRA component for the second tier food (i.e., rice)
were a child piano, sound farm animal puzzle, and a ball spinner. Brief preference
assessments were conducted at the beginning of each session and within a session if
refusal behaviors were observed or other behavioral antecedents (e.g., not playing with
the item on the previous trial, increase in stereotypical behavior, and a decrease in
attending behaviors) suggesting habituation to that item were observed.
30
Procedures
Criteria for Phase and Component Advancement
Probes were conducted for the next step and final target form prior to moving to
the next phase in the fading procedure. At any point when participants met the criterion
of 80% or better consumption of the final target form during probe sessions, the final
target form was introduced with the current treatment component. Participants were
required to consume at least 80% of bites during a next step probe session in order for the
next step to be introduced in treatment. If participants consumed less than 80% of bites
during a next step probe session, then the intermediate fading sequence was introduced.
If following the introduction of the intermediate fading sequence the participant
consumed less than 80% of bites for 3 consecutive sessions, then the next treatment
component (i.e., fading plus DRA and fading plus DRA plus EE) was introduced. If
participants met criteria for advancement to the next step and then during that phase the
percentage of bites consumed fell below 80% for 3 consecutive sessions, then the
intermediate fading sequence was introduced. Mastery criteria for any phase during
treatment were 3 consecutive sessions with bites consumed at 90% or better. If gags
occurred more than 20% during a session, then that session was not counted in the
criterion (3 consecutive sessions) to advance fading steps. That is, gags must have fallen
below 20% for the participant to move forward in treatment phases.
Baseline
Baseline probe sessions were used to determine the step at which to begin fading.
During baseline sessions 10 presentations (trials) of each main fading step were assessed.
31
For the food item introduced in the second tier of the design, probe sessions were
conducted periodically so that the participant was not exposed to an unnecessary amount
of sessions with the food not currently targeted. The researcher issued a vocal prompt
stating that it is time to eat and placed a bite in front of the participant or held the bite in
front of the child’s mouth. No programmed consequences were in place for accepted
bites. If participants accepted and swallowed any bite, then praise (e.g., “Nice eating,”
“Awesome,” “You’re fantastic,” etc) was provided. Escape was allowed (i.e., removal of
the bite/termination of the trial) if the participant said “no,” pushed the food away,
engaged in other inappropriate mealtime behaviors, or after 15-s had elapsed (whichever
occurred first).
Treatment
General Procedures. Food preparation and fading procedures varied depending
upon the type of target foods and fading procedures (e.g., texture, liquid, etc.) necessary
for each participant (See tables 1-3 above for each type of fading preparation). For
instance, when texture fading was used then the fading sequence steps were measured
based upon the viscosity of the food (e.g., puree, wet ground, ground, etc.) and when
liquid fading was used then the measurement was based upon milliliters. Each fading
step increased by 20% increments, thus there was a total of 6 main fading steps (i.e., 0%
[currently accepted form], 20%, 40%, 60%, 80%, and 100% [final form]). If the main
fading increments were not successful, then an intermediate fading procedure was
implemented prior to advancing treatment components. Intermediate fading steps
consisted of the following sequence: 1) 75% previously successful step/25% next step, 2)
32
50% previously successful step/50% next step, 3) 25% previously successful step/75%
next step, 4) 100% next step.
For each trial, the therapist prepared a pre-scooped bite of food and placed the
bite in front of the participant or presented the bite in front of their mouth. The prescooped bite was used to maintain a consistent bite size and consistent amount of food
being presented across sessions. Bite sizes varied between participants depending upon
the child’s current skill level. A gestural prompt or vocal prompt to “take a bite” or “eat
your food” was given after 15-s without independent initiation of self-feeding or failure
to open their mouth following the presentation of the bite for each trial. Following bite
acceptance and given that an expulsion did not occur, mouth clean checks were
conducted 15-s after a bite was accepted. When there was food in the participant’s mouth
following a check, then the experimenter vocally prompted the child to swallow and
continued to check for mouth clean every 10-s. A mouth clean check consisted of the
researcher saying, “Show me that the food is gone” or a similar statement only once and
no physical prompts were provided. If an expulsion occurred, then the trial was
terminated and recorded as a minus for consumption or mouth clean, unless the
participant independently initiated another acceptance and/or responded to a
vocal/gestural prompt to finish the bite. During the fading or fading plus DRA
conditions, when the child refused to take a bite by vocally stating “no,” engaged in any
other refusal behaviors (e.g., disruption), or did not respond by taking a bite after 15-s of
the bite presentation, then the trial was recorded as a minus and the bite was represented
33
as a new trial (with the exception of Bastion, an additional vocal/gestural prompt was
used). Each subsequent refusal was consequated in the same manner.
Fading with praise only. This condition began by presenting food/liquid that
was currently consumed with minimal to no inappropriate mealtime behaviors by
participants (i.e., participants’ preferred food/liquid). During this condition the therapist
gave prompts as described above (in “treatment” section) and provided praise contingent
on food consumption. After 3 consecutive meals with 90% consumption without
expulsions and gags (below 20%), the next fading step was introduced. Phase
advancement criteria and criteria to move backwards (i.e., to intermediate fading steps or
introduction of more intrusive treatment components) was followed as outlined above.
Both the next fading step and final target item probes were conducted before moving to
the next fading step. If there were 3 consecutive meals where consumption was below
80% after the intermediate fading phase sequence had been presented, then the
participant moved to fading plus DRA.
Fading plus DRA. Procedures in this condition were identical to fading with
praise except that the participant received praise and a preferred tangible or edible
contingent on each bite consumed. When this component was introduced, an additional
paired-stimulus preference assessment and a reinforcer assessment were conducted to
determine preferred items to be used as reinforcement. Criteria for fading step
advancement was followed as outlined above. If there were 3 consecutive meals where
consumption was below 80% after the intermediate fading sequence had been presented,
then the participant moved to fading plus DRA and EE. However, it should be noted that
34
EE was not necessary for either participant; had EE been necessary, it would have been
implemented following the procedures described below.
Fading plus DRA and EE. In this final condition, procedures would have been
identical to fading plus DRA except EE in the form of a non-removal of the spoon (NRS)
procedure would be added. Prior to implementing the NRS procedure, the therapist
would place a pre-scooped bite in front of the participant and vocally instruct the
participant to eat the food. If the participant did not pick up the spoon and place the bite
in their mouth within 5-s of the spoon presentation, then the therapist would provide a
gesture and another vocal instruction to eat the food. Once again, if the participant did
not respond within 5-s, the therapist would implement NRS, during which a bite on a
spoon would be within 1 inch of the participant’s mouth, following the mouth if head
turns or other disruptions occurred. The therapist would insert the bite into the
participant’s mouth when the opportunity arose (i.e., participant independently opens
their mouth). Criteria for fading advancement would be followed as outlined above.
35
Chapter 3
RESULTS
Assessments
Preference Assessments
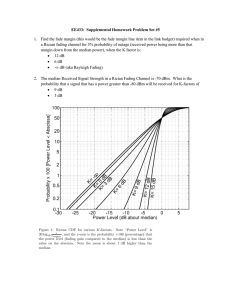
For Bastion, two paired-choice preference assessments were conducted with
jarred purees reported by his mother to be preferred and results are displayed in Figure 1.
The assessment included banana, banana-strawberry yogurt, lasagna, chicken noodle,
pasta primavera, peach yogurt, sweet potatoes, herb chicken, mixed veggies with chicken,
and apple sauce. All purees, except apple sauce, were selected during both assessments;
however, only five (banana, lasagna, pasta primavera, sweet potato, and herb chicken) of
the ten foods presented in the first assessment were assessed again in an attempt to
remove the more difficult puree mixtures to fade by texture. Banana and sweet potato
were chosen as the target foods based upon consumption during preference assessments,
parent preference, and feasibility to use with the texture fading procedure.
Results from Bastion’s pre- and post-treatment paired-choice preference
assessment are presented in Figure 2. The pre- and post-treatment assessments were
conducted with the final (table-top) form of the target foods (i.e., banana and sweet
potato). During the preference assessment conducted prior to treatment implementation,
Bastion did not consume any of the foods presented as the final form, although during the
same assessment conducted following completion of the study, Bastion consumed both
target foods, but none of the non-targeted foods. It should be noted that only the puree
36
form of one of the foods (i.e., apple) presented at a table-top texture was ever consumed
as a puree. Bastion consumed apple sauce prior to and throughout the study. These data
show that generalization to novel table-top foods and table-top foods that were consumed
in a different form (i.e., puree) did not occur.
Cheeseburger, macaroni and cheese, French fries, goldfish, Cheez-its and water
were evaluated for Vincent’s preferred foods assessment (see Figure 3). Water was the
most preferred, followed by cheeseburger and macaroni and cheese. Vincent never
selected the French fries, goldfish, or Cheez-its. In addition to water being selected
most frequently, Vincent requested for water during the preference assessment when
other items were presented as options and after the assessment was completed.
100
90
Precent Selected
80
70
60
50
40
30
20
10
0
Figure 1. Bastion paired-choice preference assessment (purees). Percentage of trials
with consumption during two paired-choice preference assessments prior to treatment.
37
100
90
80
Percent Selected
70
60
50
40
Pre
30
20
Post
10
0
Figure 2. Bastion pre/post paired-choice preference assessment (final form). Percentage
of trials with consumption during assessments of table-top textures.
100
90
Percent Chosen
80
70
60
50
40
30
20
10
0
Figure 3. Vincent paired-choice preference assessment (preferred foods). Percentage of
trials with consumption during the preference assessment prior to treatment.
38
Reinforcer Assessment for DRA Component (Vincent Only)
The first paired-choice preference assessment (see Figure 4) included eight
tangible items (toys) as follows: ice-cream cone (shooting), bee book, dog book (with
interactive stuffed dog), caterpillar game, spinning top, sound train puzzle, butterfly in a
jar, and a gerbil in a ball. The top three items were caterpillar, train puzzle, and icecream cone. Results from the reinforcer assessment (see Figure 5) demonstrated that all
items selected during the preference assessment functioned as reinforcement for Vincent
with the breaking points at PR-9 (train puzzle), PR-8 (caterpillar game), and PR-3 (icecream cone). All toys were selected during brief preference assessments during sessions
and used throughout the DRA treatment component when Pediasure was the target.
100
90
Percent Chosen
80
70
60
50
40
30
20
10
0
Figure 4. Vincent paired-choice preference assessment (Toys #1). Preference
assessment for toys to use as reinforcement during the DRA component for Pediasure.
39
100
90
80
Frequency
70
60
50
Amount of PRItem
Break
Presentatins
Total # of
Trials
40
30
20
10
0
Train Puzzle
Caterpillar
Ice-Cream cone
Figure 5. Vincent reinforcer assessment (Toys #1). Reinforcer assessment for toys used
as reinforcement during the DRA component for Pediasure.
The second paired-choice preference assessment (see Figure 6) included 10
tangible items (toys) as follows: ice-cream cone (shooting), guitar, llama book, caterpillar
game, hula girl, sound train puzzle, sound farm animal puzzle, ball spinner, child piano,
and wind-up dog. The top three items from the preference assessment were piano, animal
puzzle, and ball spinner. Results from the subsequent reinforcer assessment (see Figure
7) demonstrated that all items selected during the preference assessment functioned as
reinforcement for Vincent with the breaking points at PR-8 (piano), PR-6 (animal
puzzle), and PR-5 (ball spinner). All toys were selected during brief preference
assessments throughout sessions and used during the DRA treatment component when
rice was the target.
40
Percet Chosen
100
90
80
70
60
50
40
30
20
10
0
Figure 6. Vincent paired-choice preference assessment (Toys #2). Preference
assessment for toys to use as reinforcement during the DRA component for fried rice.
70
60
Frequency
50
Total # of
Trials
40
Amount of
Item
Presentations
PRBreak
30
20
10
0
Piano
Animal Puzzle
Ball Spinner
Figure 7. Vincent reinforcer assessment (Toys #2). Reinforcer assessment for toys used
as reinforcement during the DRA component for fried rice.
41
Treatment
The percentage of bites consumed without expulsion per session for Bastion and
Vincent are displayed in Figures 8 and 10, respectively. Data for both target foods are
presented in a multiple baseline format across foods. During baseline, Bastion did not
accept or consume any bites of his preferred foods/flavors when presented as nonpuree/unfamiliar textures; however, he did consume all 10 bites of both target foods
presented as the preferred/familiar texture (i.e., pureed/jarred food). Pureed sweet
potatoes were not introduced in treatment until session 33 when the intermediate
sequence for step 4 was also introduced for banana. Furthermore, when banana was the
only target food in treatment, as well as after sweet potato was introduced in treatment,
probes were conducted concurrently for sweet potato and banana throughout the study.
All sweet potato probes conducted prior to intervention remained at 0% consumption
until texture fading was introduced with sweet potato.
Bastion’s results observed for banana (see Figure 8) will be discussed first. When
pureed banana (i.e., step 1) was introduced as the beginning texture in the texture fading
sequence, Bastion consumed 100% of banana bites for three consecutive sessions.
During the first two probe sessions for banana during the fading only component, Bastion
consumed 100% of step 2 bites (i.e., wet ground) and refused all step 6 bites (i.e., final
step/table-top form), however, he did accept and expel one bite of step 6. Consequently,
step 2 of the fading sequence was introduced and criteria for advancement from step 2
were met after five sessions. For the second set of probe sessions, Bastion did not meet
criteria to move onto main fading steps 3 (30% of bites consumed) or 6 (no bites
42
consumed), thus the phase 3 intermediate steps (mixture of ground/wet ground textures)
were introduced as the next step in the fading progressions. Following the introduction
of the intermediate fading sequence for step 3, Bastion immediately consumed all bites
for three consecutive sessions across all intermediate steps and the main step for fading
step 3 (i.e., ground). All bites during steps 4 and 6 probe sessions were refused and the
intermediate sequence for step 4 was introduced. Similar to step 3 intermediate steps, the
step 4 intermediate sequence was effective in increasing bites consumed to 100% and
transitioning to main fading step 4. The same results occurred for steps 5 and 6, in which
the intermediate phase was necessary and effective in increasing consumption of
previously rejected textures. It is worth noting that during the fourth and fifth set of
probes, Bastion consumed 20% and 30% of bites for the next step probes (i.e., steps 5 and
6), respectively, thus not meeting criteria for the main steps to be introduced without first
introducing the intermediate steps, however, demonstrating an increase in consumption
during probes.
Corresponding to results observed for Bastion with banana, the fading only
treatment component was successful in increasing consumption of previously rejected
textures for sweet potato. Prior to the introduction of treatment, all baseline and probe
sessions for sweet potato remained at 0% consumption except for step 1 (i.e., puree)
during which all bites were consumed. Since step 1 was consumed during baseline, it
was introduced as the first fading phase during treatment and all bites presented were
consumed for 5 sessions. Probes following successful sessions for fading step 1 did not
meet mastery criteria for introduction of main fading step 2, thus the intermediate
Figure 8. Bastion percentage of bites consumed without expulsions. Results for banana (tier 1) and sweet potato (tier 2) during
texture fading. Closed data points indicate main fading steps and open data points indicate intermediate fading steps.
43
44
sequence for step 2 was introduced as the next fading progression. Responding was
variable for the first 3 sessions of the step 2 intermediate sequence phase 1 which
increased and stabilized over the following 3 sessions. Step 2 intermediate phase 2 was
introduced with perfect responding and when step 2 intermediate phase 3 was introduced,
Bastion’s consumption dropped to 0% for one session, then immediately increased to
meet criteria for advancement passed step 2 and onto the next set of probes for step 3 and
step 6. Bastion did not probe into main fading step 3 or step 6, thus the intermediate
sequence was introduced and a similar pattern observed for the step 2 intermediate fading
sequence occurred during the intermediate sequence for step 3. After meeting criteria for
advancement passed step 3, Bastion’s consumption during probe step 4 was 100%,
therefore main fading step 4 was introduced and mastered within four sessions. Once
again, Bastion’s responding during the next probe session was favorable and resulted in
the introduction of the final target form (i.e., step 6) and skipping step 5. Bastion
mastered step 6 within 3 sessions and consumption of the table-top texture of banana
generalized across people (i.e., consumed with mom).
Inappropriate mealtime behaviors for Bastion are shown in Figure 9. Bastion’s
inappropriate mealtime behaviors included vocalizations and disruptions, although at
times his refusal was passive (i.e., trials were terminated after a duration of nonresponsiveness). Bastion’s inappropriate mealtime behaviors generally corresponded to
refusal to accept and consume bites; however, during some instances in which a gestural
and/or vocal prompt was used, it was sufficient in getting Bastion to accept and consume
the bite. Bastion’s inappropriate mealtime behaviors were most often low in intensity
Figure 9. Bastion Percentage of Inappropriate Mealtime Behaviors (IMBs) per session.
45
46
and duration, as well as occurred more frequently during presentations of sweet potato
bites than when banana was targeted.
Results for Vincent (see Figure 10) varied from those of Bastion in that fading
alone was not successful in increasing consumption of non-preferred foods and a DRA
component was necessary to treat Vincent’s refusal of targeted foods. During baseline
sessions Vincent did not consume any of the non-preferred foods and only consumed
30% of trials for water (preferred item). For the tier 1 target (Pediasure), the fading
steps began with water (parental report indicated that Vincent drank water everyday)
since water was consumed the most during baseline. Responding was variable without
programmed consequences other than praise (i.e., fading and praise did not maintain
water drinking) and the most Vincent consumed during all water only (step 1) sessions
was 60% and the lowest was 0%. Even when variations in presentation method and
prompting were modified consumption remained low and below criteria for
advancement. In order to demonstrate whether Vincent would consume a mixture of
water and Pediasure, prior to the introduction of the next treatment component (i.e.,
DRA), the intermediate fading sequence for step 2 was attempted by itself with little
success. Following a paired-choice preference assessment and reinforcer assessment the
DRA component was introduced and responding remained at zero for 5 sessions until the
introduction of a measuring spoon as the presentation method and demand fading
(amount of drink required per trial decreased from 10ml to 1ml). Consumption
immediately increased to 70% without expulsions and 90% when expulsions were
excluded and continued to increase to 100% when the spoon was used to present the
Figure 10. Vincent percentage of bites consumed without expulsions. Closed data points indicate main fading steps and open
data points indicate intermediate fading steps. Results for Pediasure during liquid fading (tier 1) and fried rice during
demand fading (tier 2).
47
48
drink and 1ml of liquid was the response requirement. Following 3 successful sessions
with 1ml as the response requirement, the amount per trial was quickly increased to 5 ml
within the same day. However, after 3 sessions with the 5ml requirement, responding
decreased to 70% and 3ml of liquid presented per trial was continued for the remainder of
the study. Vincent quickly progressed through the step 2 intermediate sequence and
probed into step 3. Step 3 was introduced and after 4 sessions with step 3, Vincent met
criteria for the next probing sessions (steps 4 and 6). Vincent consumed all 10 drinks
during both fading steps 4 and 6, thus step 6 (final) was introduced as the new target.
During the first 2 sessions with step 6, Vincent consumed during all trials; however, for
the third session responding dropped to 50% (note: given this was the third session of the
day, it is possible that either Pediasure satiation or toy habituation occurred).
Afterward, Vincent met criteria for completion of intervention for Pediasure by
consuming 100% for 4 consecutive sessions. Vincent refused to consume Pediasure
from any other apparatus (even those from which he consumed water). Maintenance
sessions occurred during the completion of treatment for rice and Vincent continued to
consume the Pediasure from the blue measuring spoon only.
Baseline and probe sessions for rice remained at zero throughout the intervention
of Pediasure. When demand fading (bolus/bite size fading) was implemented
acceptance and consumption continued to remain at zero even when the intermediate
fading sequence was used. The first DRA session with rice resulted in no acceptance or
consumption. Due to ineffectiveness of the DRA procedure during the first session, a
49
second preference and reinforcer assessment was conducted with new toys which
Vincent’s mother reported to be preferred. During the next rice session following the
second preference/reinforcer assessment the new toys were utilized and Vincent
consumed all 10 bites of the first phase of the intermediate sequence for step 1 (i.e., a half
grain of rice). Subsequently, Vincent consumed all bites presented for the remaining
intermediate steps and the main fading step 1. The next probe sessions were highly
successful, having Vincent consume all bites for both step 2 and step 6 (final), therefore,
step 6 was introduced in treatment. Vincent quickly mastered criteria for step 6 and thus
completing the study. Finally, inappropriate mealtime behaviors for Vincent are shown
in Figure 11. Unlike some instances of IMBs for Bastion, all of the IMBs for Vincent
were directly associated with the refusal to accept or consumed the bite/drink whether or
not an additional vocal or gestural prompt were provided.
Figure 11. Vincent Percentage of Inappropriate Mealtime Behaviors (IMBs) per session.
50
51
Chapter 4
DISCUSSION
Previous research has shown that stimulus fading procedures when used in
combination with positive reinforcement are effective in treating behavior maintained by
negative reinforcement (e.g., McCord et al., 2001; Babbit et al., 2001). However,
previous research has reported varied results regarding the effectiveness of differential
positive reinforcement and/or fading procedures without the use of EE in the efficacy of
treating feeding disorders. For instance, Patel et al. (2002) demonstrated that positive
reinforcement alone (without EE) was not effective, while Luiselli (2000) and Hagopian
et al. (1996) both demonstrated that treatment packages containing fading and positive
reinforcement were effective in increasing food consumption. It is important to note that
the participants in the Patel et al. study displayed total food refusal, while participants in
the Luiselli and Hagopian et al. studies consumed foods orally prior to treatment, which
may be responsible for the differing outcomes. Perhaps, individuals that have not had
any or limited previous oral feeding experience may require a more intensive and
intrusive intervention. Based on previous findings, it was expected that either one or all
treatment components would be successful in increasing participants’ repertoire of foods;
in other words, results were expected to be idiosyncratic with some participants requiring
more treatment components to be successful. Results of this study support previous
research, as well as add to the growing body of literature which suggests that antecedent
interventions with or without a positive reinforcement component can be successful in the
52
treatment of food refusal (e.g., Hagopian et al. 1996; Luiselli, 2000; Luiselli, 2005;
Mueller et al., 2004; Tiger & Hanley, 2006). Moreover, data from both participants meet
the expectations of the researchers in that Bastion only required the fading component
and Vincent needed the addition of the reinforcement component in order to increase
consumption of previously rejected foods.
Bastion’s results were particularly interesting since fading alone was all that was
necessary to treat his texture selectivity, most notably because previous studies
examining texture fading required differential reinforcement and EE (e.g., Sharp and
Jacquess, 2009; Shore et al., 1998). There are several plausible explanations for results
observed for Bastion. First, since the foods used for texture fading were preferred flavors
and consumed on a regular basis, the familiarity and preference may have served as a
motivating operation for the consumption of the foods even when the texture was altered.
Additionally, the use of the intermediate phases seemed to contribute to Bastion’s success
during treatment possibly due to the gradual change and similarity to the previous texture.
The change in texture may have been less salient or unnoticeable to Bastion with the
intermediate fading steps. Perhaps, the necessity of positive reinforcement and EE for
prior studies evaluating texture fading, as well as the use of additional treatment
components with other types of fading is due to more drastic and noticeable changes in
the target item (i.e., fading steps were advanced too quickly).
Another contributing factor to Bastion’s results could be related to deficits in
chewing skills and an increased response effort to manage higher texture foods. It may
be possible that chewing deficits decreased motivation to eat higher texture foods as
53
opposed to food selectivity in general. Bastion’s chewing skills appeared to improve
throughout the course of treatment. At first, Bastion was swallowing almost immediately
after the bite was accepted; he then appeared to be mashing/moving the food with his
tongue prior to swallowing, and finally he began to use an up and down jaw motion
which approximated a mature chewing pattern. Improvements in chewing could be
supported by data for banana compared to sweet potato. Specifically, sweet potato (the
food targeted in tier two) required fewer sessions and amount of intermediate and main
fading steps than banana (tier one food) to reach criterion with the terminal texture. That
is, as the texture increased from wet ground (step 2) to ground (step 3) for banana all
subsequent progressions required the use of intermediate steps; however, for sweet potato
only wet ground and ground textures necessitated intermediate steps prior to their
introduction and chopped (step 5) was not introduced due to consumption of the final
form (step 6) during the last set of probes. Furthermore, consumption during probes
towards the end of treatment for banana (i.e., fourth and fifth set) increased, although
probe scores were lower than actual consumption of the bites because data are reported as
bites consumed without expulsion. That is, Bastion accepted some bites, expelled them,
and independently initiated additional accepts followed by swallowing. The expulsions
in those cases may have been attributed to deficits in chewing.
One limitation in regards to Bastion’s treatment is that his chewing skills were not
systematically evaluated and measured throughout the course of treatment. Assessment
of his chewing skills would have been informative regarding the efficacy of texture
fading as a treatment to remediate chewing deficits. A related outcome to the
54
development of chewing, as well as a potential limitation to texture fading, was the
amount of sessions and time required to reach criterion. For banana, treatment was in
place for about 4 months and the total number of sessions to reach criterion was 82. On
the contrary, sweet potato, which was introduced at the same time as finely chopped
banana (session 32), required about 2 months and 55 sessions to reach criterion. In
support of extended treatment for texture fading, due to Bastion’s chewing deficits, the
duration of the treatment and gradual exposure to higher textures may have contributed to
the acquisition of more advanced oral motor skills. Hence, sweet potato may have
necessitated fewer sessions due to exposure to higher textures with banana preceding the
introduction of sweet potato. However, if the duration of treatment is considered a
limitation, it would be interesting to know whether with the addition of a reinforcement
component, success for Bastion may have been demonstrated more rapidly and whether
his chewing skills would have improved as they did with the gradual exposure to higher
textures. More research is needed to determine if the gradual exposure during texture
fading, with or without intermediate steps and with or without reinforcement, is necessary
for the development of oral motor skills. Moreover, future research should examine the
use of texture fading along with oral motor exercises to teach chewing and whether the
combination of treatments could decrease the number of sessions while improving
chewing. Future research could also evaluate chewing skills in relation to texture
selectivity by examining whether selectivity by texture is more prevalent in children with
chewing deficits compared to children without chewing deficits.
55
Further, future research could examine which characteristics (e.g., chewing skills,
current food repertoire, etc.) of an individual who displays texture selectivity may
indicate their feeding difficulties to be appropriate to treat using a texture fading
procedure. Texture fading alone, without directly teaching chewing skills, may not be
sufficient in ensuring the development of chewing for some individuals; the effectiveness
of texture fading alone could depend on what level (e.g., none, minimal, advanced) of
chewing skills the individual displays prior to treatment. With that question in mind, a
study could compare two different groups of participants (e.g., those for whom no
chewing is evident prior to treatment and those who demonstrate some chewing skills) to
determine the further efficacy of texture fading. Possible results could provide evidence
as to whether the individual displaying texture selectivity does so because of an increased
response effort or because of a skill deficit. Although Bastion did not consume foods that
required advanced chewing skills prior to treatment, his mother reported that he chewed
on bottle nipples so much that she had to purchase them frequently (i.e., at least 1 per
day). Due to results observed for Bastian, it would be logical that texture fading alone
may be more effective in the treatment of selectivity due to an increase in response effort
as opposed to skill deficits. More research in this area could contribute to the
development of criteria to use during a skills assessment prior to selecting texture fading
as an intervention.
Vincent’s results were different from Bastion in that the fading component
seemed to be a less active contributor in the treatment of his food refusal and the most
effective component for Vincent was positive reinforcement (i.e., DRA). Even though
56
consumption didn’t increase for both foods until the introduction of differential positive
reinforcement, the fading component appeared to play a role in increasing consumption
of Pediasure. Specifically, following the implementation of demand fading after the
DRA component was introduced, consumption of Pediasure increased. However, it is
not entirely clear whether the initial increase observed was due to the combination of
changing the apparatus (i.e., from a cup to a spoon) and demand fading or if demanding
fading itself was responsible for the increase. On the other hand, for rice, fading may not
have been necessary in increasing consumption since during the first probe session
following the introduction of differential reinforcement, Vincent consumed all bites of
the final step and skipped fading steps 2-5. Nonetheless, it is possible that demand fading
was a necessary component for the initial increase in consumption.
Results for Vincent during liquid fading (water to Pediasure) were somewhat
different from those of previous research. For instance, Vincent’s results show that liquid
fading with differential reinforcement can be successful without the use of EE, contrary
to results from Patel et al. (2001) where a treatment package consisting of fading, DRA,
and EE was used. However, in the Patel et al. study, the treatment package was
implemented at the start of treatment, therefore it is unknown whether the EE procedure
was a necessary component for increasing consumption. In another study conducted by
Luiselli (2005), liquid fading alone was successful in contrast to the necessity of
reinforcement to increase Pediasure consumption for Vincent. Results obtained by
Luiselli may have been due to the similarity (i.e., visual and density) of the two liquids
57
(i.e., milk and Pediasure mixture), whereas for Vincent the two liquids were very
distinct, thus fading alone was successful for that participant and not for Vincent.
Another consideration regarding Vincent’s results when compared to those from the
Luiselli study is that Vincent only consumed 0-60% of presentations of his preferred
liquid (i.e., water) during baseline and fading only sessions. Vincent was less likely to
follow an instruction from the researcher to take a drink when compared to allowing free
access to water or when water was presented contingent upon a vocal mand (e.g., “I want
water, please”). For instance, Vincent would ask for water prior to the session beginning
and would be instructed to wait, while he refused subsequent presentations of water
during sessions both when a small amount (10ml) was present in the cup and when a full
cup of water was given. It appeared that Vincent preferred to eat on his own terms unless
contrived reinforcement was provided as indicated by the increase in consumption
following the addition of differential reinforcement with toys.
A limitation of Vincent’s treatment was that the amount of Pediasure consumed
per day was not increased to an appropriate volume. In addition, Vincent refused to
consume the original targeted amount (i.e., 10ml per trial) and the amount that was
accepted and used throughout the study following the implementation of demand fading
was 3ml per trial. Each day that treatment was conducted, only 3sessions (i.e., 30 trials
total with each trial consisting of 3ml of Pediasure or Pediasure/water mixture) were
conducted (equivalent to about a third of the Pediasure bottle). The restricted number
of sessions and consumption per day may have been due to either satiation with
58
Pediasure or the reinforcing effectiveness of the tangible items no longer competed
with the motivation to escape. For Vincent, EE may be necessary to increase Pediasure
consumption to a more nutritionally viable amount.
Another limitation for Vincent was that it was not determined which procedural
modification(s) were responsible for the initial increase in consumption of Pediasure.
Prior to consumption increasing, the apparatus used for presentation was modified (i.e.,
from cup to spoon) and when it was determined that the change in the presentation
method was not effective, the demand fading was implemented. Demand fading could
have been implemented with the cup prior to the spoon to determine which modification
or combination of modifications was responsible for the initial increase in consumption.
In addition, following meeting criterion for Pediasure consumption, Vincent would not
accept any drinks from an apparatus besides the measuring spoon which was the
presentation method used throughout the study. Many presentation methods were tried
(e.g., straw, Pediasure bottle, different cups, different color measuring spoon), as well
as manipulating reinforcer magnitude in a concurrent chains arrangement. It is important
to note that Vincent would accept and consume water from all the various presentation
methods that were tried with Pediasure so the refusal cannot be attributed to a skill
deficit. Finally, due to a clinical error during the treatment of Pediasure, probe 6 was
not conducted along with probe 2 and if probe 6 was conducted Vincent may have
skipped steps 2-5 as he did for rice. However, since the session with step 2 following the
59
missed probe, decreased below criterion, Vincent may not have passed the step 6 probe at
that time.
One limitation to this study in general was that only a few types of fading (i.e.,
texture, liquid, and demand [bite size] fading) were evaluated out of many possible
variations (e.g., apparatus, distance, etc). Therefore, these results cannot be generalized to
all types of fading strategies. Additionally, since it is unknown whether demand fading
or liquid fading were active or contributing treatment components for Vincent, future
research could examine the advantageousness of fading with and without a DRA
component.
An interesting finding is that texture fading was effective by itself, however,
demand fading (Vincent and rice) was not effective. This result raises the question of
whether demand fading in this context is truly a fading procedure since there is no
previously demonstrated response to start fading (i.e., the targeted food has never been
accepted and/or consumed). Conversely, with texture fading, Bastion had consumed the
target food as a puree prior to increasing the texture, so there was a point at which to
begin fading. That is, there was an opportunity to transfer stimulus control from puree
foods to table-top texture by the use of fading for Bastion and there was no established
control for rice prior to the intervention for Vincent.
Future research could evaluate whether fading may decrease the amount of
exposure to EE when EE is necessary, as well as whether fading has an effect on the
frequency and/or intensity of inappropriate mealtime behaviors during EE. The duration
of sessions, or number of sessions requiring EE could be evaluated with and without
60
fading. Since it is unknown whether fading was an active treatment component for
Vincent, future research could examine the advantages of fading with and without a DRA
component by using a multielement design. In addition, future research could attempt to
identify behavioral indicators and individual characteristics, histories, skill levels, verbal
abilities, and/or diagnoses that may predict the type and intensity of interventions
(packages or individual treatment components) needed for successful treatment.
Lastly, since fading alone and fading plus DRA were successful in the treatment
of food refusal for these participants, it lends to the recommendation for clinicians to start
with less intrusive interventions before moving to EE procedures and that EE is not
always a necessary treatment component for food refusal. In addition, parents may be
more likely to adhere to treatment procedures with this type of treatment given that some
parents are averse to using extinction procedures. Moreover, other disciplines may be
more likely to learn about and adopt procedures based on the principles of behavior
analysis when less invasive or intrusive procedures can be implemented successfully.
61
APPENDIX
Data Sheets
62
Dependent Measures Data Sheet
Participant______ Phase/Step/Session#/Target_______________________
Session Time__________
Date _____________
Data Collector: Primary/Secondary
Trial
1
2
3
4
5
6
7
8
9
10
Prompt
Accept
Expel
MClean
Therapist______________
Gag Inappropriate Mealtime Behavior
Agg
Vocals
Disrupt
SIB
63
Treatment Integrity Data Sheet
Participant______ Phase/Step/Session#/Target_______________________
Session Time__________
Date _____________
Data Collector: Primary/Secondary
Trial
Prescoop
Present
Bite
Accept
V/G
after 15s
1
2
3
4
5
6
7
8
9
10
End
trial if
expel
Therapist______________
Swallow
MC
15s
MC
10s
End
trial if
Refusal
Bx
After
Swallow
Praise Sr+
64
References
Ahearn (2002). Effect of two methods of introducing foods during feeding treatment on
acceptance of previously rejected items. Behavioral Interventions, 17, 111-127.
Ahearn, W., Castine, T., Nault, K., & Green, G. (2001). An assessment of food
acceptance in children with autism or pervasive developmental disorder-not
otherwise specified. Journal of Autism and Developmental Disorders, 31, 505511.
Ahearn, W. H., Kerwin, M. E., Eicher, P. S., & Lukens, C. T. (2001). An ABAC
comparison of two intensive interventions for food refusal. Behavior
Modification, 25, 385-405.
Babbitt, R. L., Shore, B. A., Smith, M., Williams, K. E., & Coe, D. A. (2001). Stimulus
fading in the treatment of adipsia. Behavioral Interventions, 16, 197-207.
Bandini, L. G., Anderson, S. E., Curtin, C., Cermak, S., Evans, E. W., Scampini, R., &
Maslin, M., Must, A. (2010). Food selectivity in children with autism spectrum
disorders and typically developing children. The Journal of Pediatrics, 157, 259264.
Bryan, J., Osendarp, S., Hughes, D., Calvaresi, E., Baghurst, K., & van Klinken, J.
(2004). Nutrients of Cognitive Development in School-aged Children. Nutrition
Reviews, 62(8), 295-306.
Dykman, R. A., Casey, P. H., Ackerman, P. T., & McPherson, W. B. (2001). Behavioral
and cognitive status in school-aged children with a history of failure to thrive
during early childhood. Clinical Pediatrics, 40(2), 63-70.
65
Fisher, W., Piazza, C. C., Bowman, L. G., Hagopian, L. P., Owens, J. C., & Slevin, I.
(1992). A comparison of two approaches for identifying reinforcers for persons
with severe and profound disabilities. Journal of Applied Behavior Analysis, 25,
491-498.
Freeman, K. A., & Piazza, C. C. (1998). Combining stimulus fading, reinforcement, and
extinction to treat food refusal. Journal of Applied Behavior Analysis, 31, 691–
694.
Gal, E., Hardal-Nasser, R., Engel-Yeger, B. (2011). The relationship between the severity
of eating problems and intellectual developmental deficit level. Research in
Developmental Disabilities, 32, 1464-1469.
Galensky, T. L., Miltenberger, R. G., Stricker, J. M., Garlinghouse, M. A. (2001).
Functional assessment and treatment of mealtime behavior problems. Journal of
Positive Behavioral Interventions, 3(4), 211-224.
Hagopian, L. P., Farrell, D. A., & Amari, A. (1996). Treating total liquid refusal with
backward chaining and fading. Journal of Applied Behavior Analysis, 29, 573–
575.
Luiselli, J. K. (2000). Cueing, demand fading, and positive reinforcement to establish
self-feeding and oral consumption in a child with chronic food refusal. Behavior
Modification, 24, 348-358.
Luiselli, J. K., Ricciardi, J. N., & Gilligan, K. (2005). Liquid fading to establish milk
consumption by a child with autism. Behavioral Interventions, 20, 155-163.
66
McCord, B. E., Iwata, B. A., Galensky, T. L., Ellingson, S. A., & Thomson, R. J. (2001).
Functional analysis and treatment of problem behavior evoked by noise. Journal
of Applied Behavior Analysis, 34, 447–462.
Miltenberger, R. G. (2012). Behavior modification: Principles and procedures, fifth
edition. Belmont, CA: Wadsworth/Cengage Learning.
Nicklas, T. A. (2003). Calcium intake trends and health consequences from childhood
through adulthood. Journal of the American College of Nutrition, 22, 340–356.
Patel, M. R., Piazza, C. C., Kelley, M. L., Ochsner, C. A., & Santana, C. M. (2001).
Using a fading procedure to increase fluid consumption in a child with feeding
problems. Journal of Applied Behavior Analysis, 34, 357–360.
Patel, M. R., Piazza, C. C., Layer, S. A., Coleman, R., & Swartzwelder, D. M. (2005). A
systematic evaluation of food textures to decrease packing and increase oral
intake in children with pediatric feeding disorders. Journal of Applied Behavior
Analysis, 38, 89–100.
Patel, M. R., Piazza, C. C., Martinez, C. J., Volkert, V. M., & Santana, C. M. (2002). An
evaluation of two differential reinforcement procedures with escape extinction to
treat food refusal. Journal of Applied Behavior Analysis, 35, 363–374.
Patel, M. R., Piazza, C. C., Santana, C. M., & Volkert, V. M. (2002). An evaluation of
food type and texture in the treatment of a feeding problem. Journal of Applied
Reitman, D. & Passeri, C. (2008). Use of stimulus fading and functional assessment to
treat pill refusal with an 8-year-old boy diagnosed with ADHD. Clinical Case
Studies, 7, 224-237.
67
Reynolds, K. D., Baranowski, T., Bishop, D. B., Farris, R. P., Binkley, D., Nicklas, T. A.,
Elmer, P. J. (1999). Patterns in child and adolescent consumption of fruits and
vegetables: Effects of gender and ethnicity across four sites. Journal of the
American College of Nutrition, 18 (3), 248-254.
Ringdahl, J. E., Kitsukawa, K., Andelman, M. S., Call, N., Winborn, L., Barretto, A., &
Reed, G. K. (2002). Differential reinforcement with and without instructional
fading. Journal of Applied Behavior Analysis, 35, 291–294.
Roane, H. S., Lerman, D. C., & Vorndran, C. M. (2001). Assessing reinforcers under
progressive schedule requirements. Journal of Applied Behavior Analysis, 34,
145–167.
Schreck, K. A., Williams, K., & Smith A. F (2004). A comparison of eating behaviors
between children with and without autism. Journal of Autism and Developmental
Disorders, 34, 433-438.
Shabani, D. B. & Fisher, W. W. (2006). Stimulus fading and differential reinforcement
for the treatment of needle phobia in a youth with autism. Journal of Applied
Behavior Analysis, 39, 449–452.
Sharp, W. G. & Jaquess, D. L. (2009). Bite size and texture assessments to prescribe
treatment for severe food selectivity in autism. Behavioral Interventions, 24, 157170.
Shore, B. A., Babbitt, R. L., Williams, K. E., Coe, D. A., & Snyder, A. (1998). Use of
texture fading in the treatment of food selectivity. Journal of Applied Behavior
Analysis, 31, 621–633.
68
Southall, A. & Martin, C. (2010). Feeding problems in children: A practical guide.
United Kingdom: Radcliffe Publishing.
Tiger, J. H. & Hanley, G. P. (2006). Using reinforcer pairing and fading to increase the
milk consumption of a preschool child. Journal of Applied Behavior Analysis, 39,
399-403.
Valdimassdottir, H., Halldorsdottir, L. Y., & Sigurdardottir, Z. G., (2010). Increasing the
variety of foods consumed by a picky eater: generalization of effects across
caregivers and settings. Journal of Applied Behavior Analysis, 43, 101-105.
Volkert, V. M. & Vaz, P. C. M. (2010). Recent studies on feeding problems in children
with autism. Journal of Applied Behavior Analysis, 43, 155-159.
Williams, K. E., Gibbons, B. G., & Schreck, K. A. (2005). Comparing selective eaters
with and without developmental disabilities. Journal of Developmental and
Physical Disabilities, 17, 299-309.
Zarcone, J. R., Iwata, B. A., Smith, R. G., Mazaleski, J. L., & Lerman, D. C. (1994).
Reemergence and extinction of self-injurious escape behavior during stimulus
(instructional) fading. Journal of Applied Behavior Analysis, 27, 307–316.
Zarcone, J. R., Iwata, B. A., Vollmer, T. R., Jagtiani, S., Smith, R. G., & Mazaleski, J. L.
(1993). Extinction of self-injurious escape behavior with and without instructional
fading. Journal of Applied Behavior Analysis, 26, 353–360.