Document 16056680
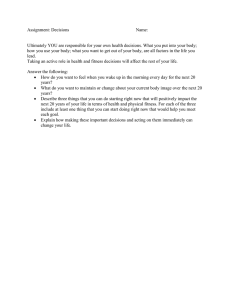
advertisement

RETROSPECTIVE EFFICACY STUDY ON A YOUTH HEALTH AND WELLNESS PROGRAM A Thesis Presented to the faculty of the Department of Kinesiology California State University, Sacramento Submitted in partial satisfaction of the requirements for the degree of MASTER OF SCIENCE in Kinesiology (Exercise Science) by Kevin Ngoc Pham FALL 2013 RETROSPECTIVE EFFICACY STUDY ON A YOUTH HEALTH AND WELLNESS PROGRAM A Thesis by Kevin Ngoc Pham Approved by: __________________________________, Committee Chair Roberto Quintana __________________________________, Second Reader Lindy Valdez ____________________________ Date ii Student: Kevin Pham I certify that this student has met the requirements for format contained in the University format manual, and that this thesis is suitable for shelving in the Library and credit is to be awarded for the thesis. __________________________, Graduate Coordinator Daryl Parker, PhD Department of Kinesiology and Health Science iii ___________________ Date Abstract of RETROSPECTIVE EFFICACY STUDY ON A YOUTH HEALTH AND WELLNESS PROGRAM by Kevin Pham Statement of Problem Obesity is a major issue in America’s society. As rates continue to climb, more and more preventative programs will arise in order to prevent the onset of this condition. However, the effectiveness of health and wellness programs for children have not been evaluated. Sources of Data Data was used from Project HYPE (Healthy Youth for Physical Excellence), an eightweek long youth health and wellness program for boys and girls ages eight to 15. Participants underwent an exercise testing protocol before the start of intervention, and after the eight-week intervention participants underwent the same protocol. Collected health and fitness variables include blood pressure, body mass index (BMI), maximal push-up score and Pacer (shuttle run) score for each participant. A paired t-test was used to analyze the data and p-value was set at <.05. iv Conclusions Reached In health outcomes, BMI slightly increased (P =.16, P =.10) for both boys and girls while systolic and diastolic blood pressure decreased for boys (P =.04, P =.06) and systolic and diastolic blood pressure increased for girls (P =.27, P =.03). In fitness outcomes, maximal push-up score increased significantly (P =.000001, P =.5.1 E-09) and Pacer Score increased significantly (P =.0068, P =.0013) for both boys and girls. This results of this study indicate that a youth health and wellness program can help its’ participants maintain a healthy BMI while significantly improving fitness outcomes in children ages eight to 15. _______________________, Committee Chair Roberto Quintana _______________________ Date v DEDICATION To my parents and the Boykins for always supporting me. vi ACKNOWLEDEGMENTS I would like to thank Mission Oaks Recreation and Park District for giving me the opportunity to coordinate and develop this program and allowing me to use Project HYPE’s data set. I would like to thank Dr. Quintana and Dr. Valdez for helping me complete this thesis as well. vii TABLE OF CONTENTS Page Dedication ................................................................................................................................ vi Acknowledgments.................................................................................................................. vii List of Tables ............................................................................................................................ x Chapter 1. INTRODUCTION .............................................................................................................. 1 Background ................................................................................................................. 1 Purpose of study .......................................................................................................... 5 Thesis hypothesis ........................................................................................................ 5 Assumptions ................................................................................................................ 6 Limitations and delimitations .................................................................................... 6 Significance of study ................................................................................................... 7 2. BACKGROUND OF THE STUDY ................................................................................... 9 Definition of obesity and associated diseases ............................................................ 9 Metabolic syndrome ................................................................................................ 14 Causes of obesity ....................................................................................................... 15 Decline in physical fitness......................................................................................... 18 Measures to prevent obesity ..................................................................................... 19 Improving physical fitness ....................................................................................... 21 Cooper institute and FITNESSGRAM® standards .............................................. 23 Conclusion ................................................................................................................. 24 3. METHODS ....................................................................................................................... 25 Summary of methods ................................................................................................ 25 Participants ............................................................................................................... 25 Instruments................................................................................................................ 26 Procedures ................................................................................................................. 27 Design and analysis ................................................................................................... 29 Pacer score values ..................................................................................................... 30 Ethical considerations .............................................................................................. 30 Internal validity......................................................................................................... 31 viii External validity ....................................................................................................... 32 4. RESULTS ......................................................................................................................... 33 Introduction............................................................................................................... 33 Summary of results .................................................................................................. 33 Statistical analysis ..................................................................................................... 33 5. DISCUSSION ................................................................................................................... 41 Introduction............................................................................................................... 41 Health outcomes ....................................................................................................... 41 Fitness outcomes ....................................................................................................... 46 Attendance and dropout ........................................................................................... 49 Recommendations ..................................................................................................... 50 Recommendations for program quality .................................................................. 52 Recommendations for data collection .................................................................... 53 Summary.................................................................................................................... 54 Appendix A. Nutrition Curriculum ........................................................................................ 55 Appendix B. Fitness Curriculum .......................................................................................... 57 Appendix C. Summary of Attendance .................................................................................. 62 Appendix D. Program Evaluation ......................................................................................... 64 References ............................................................................................................................... 68 ix LIST OF TABLES Tables Page 1. Table 1 Participant demographics………………………………………………..35 2. Table 2 Boys’ health outcomes: pre and post HYPE intervention………...........36 3. Table 3 Girls’ health outcomes: pre and post HYPE intervention…………...….37 4. Table 4 Boys’ fitness outcomes: pre and post HYPE intervention………………37 5. Table 5 Girls’ fitness outcomes: pre and post HYPE intervention……………...38 6. Table 6 Comparison of boys’ data with FITNESSGRAM®’s Healthy Fitness Zone criteria………………………………………………………………….……….38 7. Table 7 Comparison of girls’ data with FITNESSGRAM®’s Healthy Fitness Zone criteria………………………………………………………………….……….39 8. Table 8 Comparison of all participants’ data with FITNESSGRAM®’s Healthy Fitness Zone criteria…………………………………………………………….40 x 1 INTRODUCTION Since the 1970’s, the health and fitness of America’s youth has steadily declined. Presently the Center for Disease Control (CDC) estimates that two out of every three children ages five-18 are considered overweight or obese, conditions in which there is excess fat mass accumulated in the body caused by poor diet and lack of physical activity (CDC Childhood obesity facts, 2011). Research has shown that an excess of fat mass has harmful effects towards health when compared to children in a normal weight class (Mahshid, Noori, & Merchant, 2005). Obese children are more likely to develop chronic conditions such as high blood pressure, abnormal triglyceride levels, kidney failure and insulin resistance. Worse, if children have a combination of these risk factors they are classified as having metabolic syndrome. Children with metabolic syndrome have an increased risk of coronary heart disease, stroke, type II diabetes and a greatly reduced lifespan. Physical activity is difficult for children who have some form of these chronic conditions because these diseases place a heavy strain on the human body and therefore engaging in physical activity and exercise that is relatively easy for a healthy child will be tremendously harder for an unhealthy child. Consequently, children with chronic health issues are more likely to have a lower fitness level. If preventative measures are not implemented quickly to prevent these risk factors and chronic diseases, then the health and fitness of America’s youth will continue to spiral downwards without any signs of slowing. Although there are many factors that contribute to the decline in the health and fitness of America’s youth, the main culprits to this problem are poor diet and lack of 2 physical activity. America’s diet lacks in quality nutritional content due to the mass development of fast food chains and the abundance of processed foods in supermarkets (CDC Children’s food environment state indicator report, 2011). Currently the foods that Americans consume contain excess amounts of saturated and trans fat which contribute to weight gain. Worse, these foods often contain high levels of sodium, which will cause the body to retain more water and consequently lead to weight gain and the development of high blood pressure. Moreover, children are just eating more food in general. They are exceeding their daily caloric limit while reducing their daily caloric expenditure and in doing so the body will store extra nutrients as fat. Children are also less physically active due to the advancements of technology and entertainment as they are more likely to engage in video games and watch television instead of playing outside (Rideout, Voeer, & Roberts, 2010). Combined with an unhealthy diet and sedentary lifestyle, this will contribute to weight gain due to surplus of calories in and a decreased in calories expended. Thus, the combination of a poor diet and lack of physical activity are key factors in why youth in America are so unhealthy. Reducing the onset of obesity and other chronic conditions will help improve health and fitness outcomes in youth. One method of doing this is the implementation of primary prevention techniques to youth and their families. Primary prevention is described as the prevention of diseases before their biological onset can occur. Examples of these primary prevention techniques include educating the parents and children on the dangers of a sedentary lifestyle and having the participants engage in moderate to vigorous physical activity daily. If primary prevention is implemented early, the risk of 3 obesity and other chronic diseases will be reduced greatly and will consequently improve the health of America’s youth. An example of primary prevention to help improve health and fitness outcomes is Project HYPE (Healthy Youth for Physical Excellence), a free health and wellness program for kids ages eight to 15 and their families in the Arden and Arcade area of Sacramento. Mission Oaks Recreation and Park District (MORPD) has paid for and supported HYPE each year since its creation in 2008. Recently, community partners such as Health Net, Target, California Family Fitness, and Sacramento State Nursing and Kinesiology have supported and sponsored this program with financial support, gift cards and volunteers. HYPE operates out of the Swanston Community Center and each year the core of this program is an eight-week long health and wellness summer camp for kids ages eight to 15. HYPE started with only 20 participants its first year and each following year its registration numbers have doubled; in the summer of 2012, over 100 participants signed up for this program and 45 participants completed the eight-weeks. Recently in the summer of 2012, this health and wellness program educated children and their families on the importance of proper nutrition and provided the participants with structured exercise in order to improve their health and fitness outcomes. Structured exercise included recreational activities and resistance training that included body weight, resistance band and free weight dumbbell exercises. Aerobic activities such relays, obstacle courses, and active recreation games such capture the flag, tag games, and walking trips were also implemented along with the other exercises mentioned above. Sacramento State Nursing and Kinesiology students led the kids through these activities, 4 along with various local group fitness instructors who taught the kids yoga, kickboxing, boxing, martial arts, salsa and hip-hop classes. In the summer of 2012, Sacramento State Nursing and Kinesiology students administered exercise testing on boys and girls during the first week of the program. Anthropometric measurements before exercise testing included height, weight, hip to waist ratio, blood pressure and heart rate. After these measurements were taken, the interns performed various exercise testing measurements, which included the 20-meter shuttle (Pacer Test) and maximal push-up test on all participants. After eight-weeks HYPE-intervention, which consisted of nutrition education and structured physical activity mentioned earlier, the participants were re-tested again using the same procedures and the data was recorded in excel spreadsheets. The Cooper Institute is a nonprofit research and education organization, which aims to promote exercise in order to improve and maintain health and well-being. Recently, the Cooper Institute released fitness assessments and normative healthy values for youth called the FITNESSGRAM®. These assessments are designed to assess a child’s cardiovascular fitness, body composition, muscular strength, endurance and flexibility while comparing the obtained results to healthy standards (Cooper Institute, 2007). These standards are denoted as “Healthy Fitness Zone” and being categorized in this zone illustrates good health and well-being. The basis for the parameters of these zones are national fitness test data collected over several years which tested youth body composition and physical fitness. Out of all of the fitness standards, the Cooper Institute has the largest and most peer reviewed fitness data for youth. In summary, the Cooper 5 Institute and FITNESSGRAM® are useful tools in determining the overall health of youth. Purpose of Study Mentioned earlier the decline in health and fitness is a huge problem for America’s youth. Although primary prevention techniques like Project HYPE have been implemented for some time now to improve the health and wellbeing of America’s youth, the effectiveness of these programs have not been evaluated. Many programs may only benefit some populations and may be too costly to sustain for an extended period of time. Therefore, the purpose of this study is to compare the averaged exercise testing data of participants from pre-HYPE intervention to post-HYPE intervention and determine whether or not the participants improved significantly (P<.05) in their health and fitness outcomes after eight-weeks. If the participants from HYPE improve significantly, the Cooper Institute’s FITNESSGRAM® standards will be used to assess each child’s individual improvements and whether the participants meet the criteria for the Healthy Fitness Zone. Thesis Hypothesis The first hypothesis of this study was the participants will show a significant improvement (P<.05) in their health outcomes (BMI and blood pressure) after the eightweek HYPE intervention. The second hypothesis of this study was that the participants will show a significant improvement (P<.05) in physical fitness categories of muscular endurance cardiovascular and (Push-up Test and Pacer Test). 6 Assumptions The families were given handouts on what to eat and how often to exercise. This study assumed that the parents and children exercised and ate healthy outside their time in the intervention program. During exercise testing and exercise activities, the children were assumed to perform at a maximal effort. Limitations and Delimitations A limitation to this study is the fact that we are using data that already has been collected. The data only includes exercise testing values collected from boys and girls. The data does not include surveys from the youth or the parents which would help determine behavioral and attitude changes towards physical fitness and nutrition. The sample size for the data set includes 23 boys and 22 girls, which is a total of 45 participants. Ideally, a larger sample size will help contribute to significant relationships between the populations. Another limitation is that waist circumference, flexibility, and muscular endurance (abdominal) was not collected in this data set. If these values were collected, the analysis of the data would give a clearer and more precise picture of the improvements in health. Finally, outside physical activity that the youth participated in after the program was not accounted for. Many of these children engaged in afterschool and summer sports on their own. Delimitations to this study include using data from participants who finished the eight-week program. Some participants attended the program for a couple of weeks and dropped out due to school, vacation and a lack of interest. These participants’ data will be ignored during analysis of the data set. This study will focus solely on youth ages 7 eight to 15 that are mostly low income and from the Arden-Acade area, a district within Sacramento County. Heart rate and hip to waist ratio were collected as a health measurement during pre and post intervention, but, there is not sufficient literature on if these variables significantly affect youth. Therefore, BMI and blood pressure will be analyzed instead since there is an abundance of literature on these variables. This study focuses on quantitative data since qualitative data such as interviews and surveys were not collected. Literature that will be reviewed include obesity and related illnesses and youth health and wellness programs but, adult wellness programs will not be reviewed since this study primarily focuses on adolescents. Significance of study Among the various issues in America’s society, the decline in the health and fitness of America’s youth has tremendous consequences if left unresolved. Adolescents who are not physical fit will develop chronic health conditions, which will require lifelong treatment and places a huge burden on America’s taxpayers. The cost of treating these conditions amounts to billions annually and if trends continue, the life expectancy of America’s youth will decrease while health care costs will skyrocket to exponential proportions. If researchers can prove the effectiveness of primary prevention programs, then large-scale implementation to improve children’s fitness and health can occur. In the long run, the prevention of these chronic conditions will lead to healthier lives while simultaneously reducing the financial burden that is associated with treating these 8 conditions. In summary, this study can provide useful insight in assessing the effectiveness of improving health and fitness outcomes in children. 9 BACKGROUND OF STUDY It is no coincidence that the decline in the health and fitness of America’s youth coincides with the rise of obesity rates in children (CDC Overweight and obesity, 2011). Current statistics indicate that two out of three adolescents are overweight or obese (National center for disease statistics, 2011). Children that are overweight or obese have a higher chance of developing chronic diseases which leads to a lower quality of life. Consequently, the purpose of this review of literature is to: (1) describe obesity and diseases associated with this condition, (2) possible causes of obesity and its relationship to the decline in physical fitness, (3) measures to prevent obesity (4) improving U.S. children’s physical fitness and (5) research detailing how the Cooper Institute FITNESSGRAM® Standards were developed and associated assessments. Definition of obesity and associated diseases One of the most prominent health issues in America today is obesity. The CDC defines obesity as a condition where an individual accumulates excess body fat (CDC Halting the epidemic by making health easier at a glance, 2011). Obesity and overweight are sometimes used synonymously, but, these two terms have different meanings. Overweight is a condition where the body has excess body weight while obesity is a condition where the body has excess body fat. BMI is a useful tool in determining if an individual is normal, overweight, or obese. Individuals are considered normal if their BMI is between the values of 18.5 and 24.9 and a BMI of 25 to 29.9 is considered overweight. For BMI’s over 30, individuals are considered obese and the classification of obesity is divided into three classes. Obese Class I (moderately obese) pertains to a 10 BMI of 30-35, Obese Class II (severely obese) has BMI values from 35 to 40 and Obese Class III (very severely obese) is classified as a BMI of over 40. Obesity rates for Americans have reached epidemic proportions. In a recent study by the CDC, 58 million of American adults are overweight, 40 million are obese and 3 million are morbidly obese. Eight out of 10 Americans over 25 are overweight and 78% of Americans do not meet basic physical activity level recommendations, and 25% are completely sedentary (CDC Halting the epidemic by making health easier at a glance, 2011). Obesity rates for children have also quadrupled within the past 30 years. In 1980, approximately 7% of children were considered obese and currently over a third of American youth are overweight or obese (CDC Overweight and obesity, 2011). Obesity prevalence in both boys and girls is highest among American Indian/Alaska native, Hispanic and African American while Asian American/Pacific Islander and Caucasian have lower rates (CDC Overweight and obesity, 2011). Various diseases are associated with obesity. The first disease is high blood pressure or hypertension. Blood pressure is the amount of pressure in an artery at a given amount of time. Blood pressure is read with two numbers, systolic and diastolic. Systolic pressure represents the contraction while sending blood to the body and the normal value is 120mmHg. Diastolic is when the heart relaxes after contraction and the normal value is 80mmHg. An individual is classified as prehypertensive if one or both of their systolic and diastolic values are over the normal value of 120/80mmHg and if one or both of their readings exceeds 140/90mmHg this individual is classified as hypertensive (ACSM, 2009). Obese individuals tend to develop prehypertension or hypertension due 11 to the high concentration of adipocytes or fat cells in their body (Narkiewicz, 2005). High levels of adipocytes create a hormonal imbalance which can cause long-term activation of the sympathetic nervous system (our fight or flight nervous system) and this results in an increase in blood pressure (Narkiewicz, 2005). Individuals with high levels of adipocytes are also likely to be diagnosed with arteriosclerosis, a chronic condition in which their arterial walls are lined with plaque, which consists of fat deposits, cholesterol, and other substances. Plaque buildup causes narrowing of an artery that forces the heart to work harder to pump blood to muscles. This in turn causes an increase in systolic blood pressure and as a result, an individual is more susceptible to left ventricular hypertrophy, a condition in which the left ventricle thickens in response to the heart being overworked (Narkiewicz, 2005). It is very rare for healthy children to have a blood pressure reading of 140/90. However, obese children are more likely to develop prehypertension or hypertension in their future if they do not change their lifestyle. High salt diets also contribute to the increased chance of hypertension. The CDC recommends daily intake for salt at <2,300mg for adults and <1,500 for specific populations (2009). The average amount of sodium consumed daily by Americans exceeds 3,200mg and foods that contain high levels of sodium are listed as these categories: bread and rolls, cold cuts/cured meats, pizza, poultry, soups, sandwiches, cheese, pasta mixed dishes, meat mixed dishes, and savory snacks (CDC, 2012). Children consume these high salt foods at their school lunches, fast food restaurants, and store bought goods. Over time, the increased dietary sodium consumption causes the renal system to function improperly. The mechanism of sodium and high blood pressure 12 is described as followed: The role of the renal system is to filter out excess waste products in the blood and excrete this waste as urine. High levels of sodium in the blood cause the body to retain more water and also activates the renin-angiotensin system and as a result blood pressure increases (Narkiewicz, 2005). Obesity may also cause glomerular hyperfiltration, increased urinary albumin loss and progressive loss of renal function caused by focal segmental glomerulosclerosis; all of these conditions help accelerate kidney failure (Narkiewicz, 2005). Consequently, it is evident that a high sodium diet is potentially toxic and dangerous and contributes enormously to the development of hypertension. Secondly, obese children are more likely to have an impaired fasting glucose that can leads to diabetes. Since 1994, the prevalence of diabetes has tripled and as a result, boys and girls born in 2000 have an estimated risk of 30% and 40% in developing diabetes during their lifespan (Lytle, 2012). Diabetes is a condition where the body has a difficult time regulating blood sugar. A fasting blood glucose of 100mg/dL to 124mg/dL is considered prediabetic and a value of >125mg/dL is classified as diabetes. There are two types of diabetes, which are type I and type II. Type I diabetes is diagnosed at an early age in which the pancreas does not produce enough insulin, a hormone essential for glucose uptaking into the cell for energy. Type II diabetes is an over production of insulin which causes the body to become unresponsive to this hormone. Obesity is closely linked to type II diabetes because of consuming excess simple sugars. Many sugary drinks and snacks contain refined and simple sugars which can cause a spike in blood sugar if consumed on a regular basis. A spike in blood sugar will cause insulin to 13 release and if over time, the amount of insulin produced in the body will cause insulin resistance and the body will slowly stop responding to this hormone. As a result, youth who are diagnosed with type II diabetes will need to constantly monitor their blood glucose levels to determine if they are hypoglycemic (low blood sugar) or hyperglycemic (high blood sugar). Neglecting to manage blood sugar levels will result in blurred vision, frequent urination, dizzy spells, seizures, numbness, heart palpitations, and even death (Lytle, 2012). Children who are diagnosed with type II diabetes will have to take medication to control their glucose levels and exercise will be encouraged in order to help increase insulin sensitivity. The third disease associated with obesity is heart disease. Obese individuals tend to have more body fat and thus more body mass compared to a healthy weight individual. As a result, obese individuals have a higher metabolic demand due to more body mass and this will force the heart to pump more blood to working tissues. Consequently, cardiac output and workload is higher in an obese individual and this causes increased strain and stress on the heart. In addition, due to the increased venous return the ventricle’s chamber wall will become dilated which leads to increased wall stress and ultimately causes an increase in myocardial mass and left ventricular hypertrophy (Poirier et al., 2006). Moreover, an increase in left ventricular mass can contribute to the development of left atrial enlargement, a condition that increases the risk of sudden heart failure. In addition to chamber enlargement, high levels of adipose tissue can impair the heart’s ability to function properly in two ways: fat surrounding the heart increases and creates pressure and compression and fat can accumulate inside the heart muscle and 14 cause cardiac cell dysfunction and death, a phenomenon called lipotoxicity (Poirier et al., 2006). As a result, these conditions associated with obesity (increased cardiac output, left ventricular hypertrophy, left atrial enlargement, lipotoxicity) influences the development of heart disease and heart failure. If children are diagnosed with obesity at an early age, it is very likely that they will encounter one of these conditions in their lifetime, which will increases the risk of heart disease (Poirier et al., 2006). Metabolic syndrome The conditions mentioned above (obesity, hypertension, impaired fasting glucose) are all components of metabolic syndrome, a condition that is associated with overweight and obese children. Similar to the rise in obesity rates, the prevalence of metabolic syndrome has increased from 4% to 29% in the period of 30 years (Steinberger et al., 2009). Research indicates that children of parents with metabolic syndrome are at a higher risk of developing metabolic syndrome and cardiovascular risk factors due to shared genetics and environmental factors (Steinberger et al., 2009). Metabolic syndrome is also more likely to affect ethnic groups such as African Americans and Latinos while Caucasians and Asian Americans are less likely to have these risk factors (Steinberger et al., 2009). Children with risk factors of metabolic syndrome are also likely to live a sedentary lifestyle, engage in little to no physical activity, and consume unhealthy food. The criteria to classify metabolic syndrome focus on obesity (BMI and waist circumference), dyslipidemia (high LDL’s and low HDL’s), hyperglycemia (>100mg/dL), and hypertension (>140mmHg/90mmHg). If three or more of these factors 15 are present during childhood, there is an increased risk for developing type II diabetes, cardiovascular disease and higher mortality rate during adulthood (Cruz & Goran, 2004). Evidence of this phenomenon was demonstrated in a long-term study with overweight and non-overweight children. In this study, 16% of children with metabolic syndrome at the age of 13 had the syndrome later in their life at the mean age of 22 with significantly higher levels of BMI, waist circumference, body fat, and impaired triglycerides compared to their measurements at the age of 13 (Sinaiko, 2012). In addition, researchers in this study developed a metabolic factor cluster score by taking the average of the standardized deviates of the five metabolic syndrome criteria. The results indicated that the cluster score at age 22 was approximately eight times higher in the individuals with metabolic syndrome at age 13 than non-metabolic syndrome group (Sinaiko, 2012). Furthermore, there was a strong tracking effect for the cluster score that indicates that the relative rank of cluster score at age 13 predicted its rank at age 22 (Sinaiko, 2012). The findings from this study suggests that children who have risk factors of metabolic syndrome at an early age are more likely to display the same risk factors at an older age. Therefore children who are at risk for metabolic syndrome should be closely monitored by health professionals in order to prevent the onset of chronic diseases. Causes of obesity Many factors play a role in the development of childhood obesity. America’s middle and high schools provide sugary drinks and high calorie processed food that can attribute to weight gain. In a recent study by the CDC, more than half of middle schools and high schools in America sell these drinks and snacks in vending machines, at school 16 cafeterias and school sporting events (CDC Halting the epidemic by making health easier at a glance, 2011). Major fast food chains/restaurants are also culprits in the development of obesity. Statistics indicate that children obtain 29-38% of their daily food intake from these restaurants, which contain excess calories and can cause many youth to gradually gain weight (CDC Halting the epidemic by making health easier at a glance, 2011). Children who consume these foods daily can gain up to approximately 6 pounds a year and over a period of 10 years, a child can gain up to 60 lbs of fat, which equals 210,000 calories (CDC Overweight and obesity, 2011). As a result, the daily consumption of processed foods will eventually lead to unwanted weight gain. The lack of nutritious foods in low-income neighborhoods also contributes to the development of obesity. In many rural, low income and high minority neighborhoods there is a lack of access to supermarkets (Larson, Nelson & Story, 2009). Without supermarkets, many individuals in these communities lack nutritious foods like fresh fruits and vegetables while processed foods are the staple of their diet. Families who live in low-income neighborhoods also assume that healthy food is more expensive and will perish faster which results in their consumption of cheap and unhealthy food. Studies also indicate that minorities who live in rural and low-income neighborhoods are more likely to develop obesity, with adolescent Latino and African American girls at the highest risk while Caucasians and Asians are at a lower risk (Lytle, 2012). Another cause of obesity is the decrease in physical activity in schools. Statistics by the U.S. Department of Health and Human Services state that only 18% of high school students met the recommended minimum of 60 minutes of aerobic activity each day (U.S. 17 Department of Health and Human Services, 2008). Moreover, a similar suggests that the quality and quantity of physical education in elementary schools has decreased tremendously over the years. The California Endowment, a nonprofit organization aimed to improve the health and well-being of California, states that as only four minutes of every half hour of exercise is considered moderate to hard exercise intensity and less than a third of California schools meet the exercise duration requirement mandated by law (California Endowment, 2007). Children who live in areas of poverty are also at a higher risk of being overweight and obese. The study illustrated that schools in lower economic areas spend less time being active in physical education when compared to children in higher economic areas, which contributes to a higher prevalence of obesity rates (California Endowment, 2007). Without structured physical activity in the school system, youth will likely see a significant gain in weight because of a caloric imbalance. Contributing to the lack of physical activity is the advancement of technology. Children eight-18 years old spend an average of seven and a half hours a day using entertainment media, which include television, computers, video games and cell phones (Rideout, Voeer, & Roberts, 2010). This statistic suggests children are staying inside and accessing these media options instead of engaging in physical activity. Moreover, children are more likely to rely on automobile transportation to get to school as opposed to walking and biking. A recent study found that only 13 percent of U.S. schoolchildren walked or rode their bikes to school, compared to 40 percent in 1969 (Brownson, Boehmer, & Luke, 2005). Youth relying on high technological advances will equate to more calories in and less calories out which leads to weight gain. 18 The combination of a sedentary lifestyle along with a poor diet results in a caloric imbalance that shifts the body into a fat storing mode. Consequently, these variables listed above are the main culprits for the rise in obesity rates. Decline in Physical Fitness Obesity clearly increases the morbidity risks and mortality rates in children, but also can negatively affect physical fitness patterns as well. Researchers discovered this phenomenon in studying the physical activity patterns of children who were obese (BMI >30) and non-obese (BMI within 18-25). In this study, they observed 133 obese and nonobese children wearing accelerometers, devices that provide minute-to-minute quantification of intensity and duration of body movement. Physical activity such as walking, running and exercising while sedentary behavior such as watching TV and playing video games were recorded by the accelerometers. They were instructed to go about their regular daily activities while wearing the accelerometers for seven days. At the end of the seven days, researchers collected the data and discovered that obese boys were 15% less active on weekdays and 29% less active on weekends while obese girls 20% less active on weekday and 36% less active weekend (Page et al., 2005). Overall, obese children were less active on all hourly periods on both schooldays and weekends while non-obese children expended an estimated 296 kcal more per day when compared to obese children (Page et al., 2005). Moreover, in another similar study with obese and non-obese children wearing accelerometers for seven days, researchers found that obese children spent 80.4% of their monitored time in sedentary behavior and only 2.5% in moderate to vigorous physical activity (Hughes et al., 2006). This was equivalent to 551 19 minutes of sedentary activities and only 18 minutes of physical activity. The results of these studies indicate that obese children demonstrate low patterns of physical activity and physical fitness and are likely to sustain unless intervention is implemented. Measures to prevent obesity A combination of a healthy diet and active lifestyle is beneficial in preventing the onset of obesity and its associated diseases. Physical activity helps improve insulin sensitivity, improve HDL cholesterol, lower LDL cholesterol and reduce blood pressure (Steinberger et al., 2009). Physical activity also lowers BMI and changes body composition by reducing fat mass while increasing lean muscle mass (Steinberger et al., 2009). ACSM recommends at least 30 to 60 minutes of physical activity per day in order to maintain optimal health but a majority of Americans do not meet this recommendation (ACSM, 2009). Dietary recommendations by the American Heart Association consists of limiting red and processed meat, fried food, high-fat dairy foods, and sugar sweetening beverages while increasing the consumption of whole grains, fruits and vegetables (Gidding et al., 2009). A healthy dietary intake helps improve insulin sensitivity, reduces the risk of heart disease, and reduces both BMI and mortality rate (Gidding et al., 2009). Studies also show that a Mediterranean diet rich in fruits, vegetables, whole grains, and fish have beneficial effects on cardiovascular risk factors (Gidding et al., 2009). However, health professionals should focus on limiting total caloric intake and establishing healthy eating patterns as part of a comprehensive healthy lifestyle (ACSM, 2009). 20 In order to implement dietary changes and increase physical activity levels, the uses of primary prevention programs have seen an increase in recent years. Primary prevention has illustrated better outcomes in decreasing obesity in children when compared to other methods of prevention (Caterson & Gill 2002). Primary prevention is preventing the onset of the disease, which includes health education and environmental changes. Currently there are many private and community based health and wellness programs that have shown promising results in reducing the weight and improving children’s health. In 2002, the National Hypertension Association developed VITAL (Values Initiative Teaching About Healthy Lifestyle) which is a health and program aimed to combat childhood overweight and obesity. Recently, VITAL was implemented in 29 schools of the Catholic Diocese of Pittsburg for eight-weeks, which split up the schools into a control group and intervention group. The curriculum of VITAL included weekly lessons instructed by elementary school teachers that promoted healthy nutrition and physical activity. After the eight-week program, both control and intervention groups were monitored for two years to observe the changes in BMI. The results of the study indicated that the intervention group significantly decreased their BMI percentile (P=.015): the control group decreased their BMI percentile by 1.1 (66.1 to 65) while the intervention group reduced their BMI percentile by 3.9 (62.8 to 58.9) (Manger et al, 2012). The significant results of this program can be explained by the fact that parents enjoyed the VITAL program (78% indicated that program was good/excellent in influencing the families positively), children participated in physical activity more regularly (56% of children exercised frequently at first week while 76% exercised 21 frequently at 8th week) and children chose healthier food choices (60% of parents indicated children consumed healthy food at first week and 80% of parents indicated children consumed healthy food at 8th week) (Manger et al., 2012). However, the success of youth health and wellness programs is largely dependent on parental involvement. These researchers also suggest in their analysis of weight management programs that treatment for overweight and obesity should include family-based behavior change components under the supervision of a health professional in order to change the lifestyle of the whole family (Manger et al., 2012). Supervision after the end of the program is required as well in order to prevent the families from relapsing and reverting back to their previous lifestyle. In conclusion, primary prevention has demonstrated positive results in decreasing the prevalence of obesity in children. Improving physical fitness In addition to primary prevention programs such as VITAL, there are many other programs paid for by the U.S. federal government to promote physical activity and improve physical fitness. The President’s Council on Fitness, Sports and Nutrition has recently created a program called The President’s Challenge that aims to increase the health and physical fitness of youth and adults. Core components of this program include exercise-testing protocols for youth and adults, fitness and health assessments and incentives for participating in exercise and improving health (President’s Council on Fitness, Sports & Nutrition, 2013). The goal for participants who enroll in this program is to assess their health through and physical fitness through various tests and offer tips and guidance to improve upon their results (President’s Council on Fitness, Sports & 22 Nutrition, 2013). In addition, the President’s Challenge has been applied to schools during the academic year and provides financial assistance to institutions that lack the necessary funds needed to implement this program. Since its creation, this program helped improve the health fitness of over 50 million children and adults and has helped countless others in living a healthier and happier lifestyle (President’s Council on Fitness, Sports & Nutrition, 2013). The CDC and the U.S. Department of Health and Human Services also have implemented programs similar to The President’s Challenge. The CDC has created a free Youth Physical Activity Toolkit that is specifically made for Physical Education teachers to promote physical activity for schoolchildren (CDC, 2013). Other community organizations such as churches and community centers are also welcome to teach this program as it offers step-by-step instructions on how to facilitate fitness activities to youth (CDC, 2013). Materials that go along with the Toolkit include educational handouts, outlined lectures, and PowerPoint presentations (CDC, 2013). Similarly, the U.S. Department of Health and Human Services has established a 10-year agenda called Healthy People 2020 in order to improve health and fitness for adults and adolescents. The goals of this program are to increase public awareness and understanding of the determinants of health and disease, provide measurable objectives and goals that apply to national, state and local levels, and engage in multiple sectors to strengthen existing policies and practices in order to improve health (Healthy People, 2012). With regards to improving fitness, Healthy People 2020 has made significant structural improvements to areas to public fitness areas such as the availability of sidewalks, bike lanes, trails and 23 parks and enacted legislative polices in order to encourage physical activity in youth (Healthy People, 2012). This program also is in the process of enacting state and federal policies to promote physical activity in the childcare setting, recess and physical education in public and private schools and limiting the amount of television viewing and computer usage throughout the day (Healthy People, 2012). Improving fitness in adolescents is still an uphill battle, but these comprehensive programs have shown to improve the fitness outcomes of thousands of youth across America. Cooper Institute and FITNESSGRAM® Standards The Cooper Institute, a 501.c.3. nonprofit research and education organization, was established in 1970 by Kenneth H. Cooper. The mission of the Cooper Institute is to research the field of preventative medicine and public health while communicating this research to scientific communities as well as the public. FITNESSGRAM®, a program of the Cooper Institute, is a comprehensive assessment protocol for youth. This program assesses cardiovascular fitness, body composition, muscular strength, and flexibility by utilizing various field tests and comparing the results to established health standards. The criteria for the health standards associated with the FITNESSGRAM® include “Healthy Fitness Zone” which indicates good health and “Needs Improvement” which suggests that the participants need to increase their efforts in order to reach the Healthy Fitness Zone. The standards for FITNESS GRAM criteria are evaluated with a percentile table. Percentiles represent the percentage of people who score above or below at that value. The Cooper Institute has established these percentile standards by analyzing specific groups and norms and thus created standards for youth to achieve. Consequently, 24 colleting youth values and comparing them to FITNESSGRAM® standards is a fast and easy way to assess the health of the individual. Conclusion Obesity rates have continued to climb since the 1970’s while the fitness and physical activity levels of America’s youth has steadily declined during this period of time as well. Millions of children are affected and will consequently suffer detrimental health effects unless change is implemented. Although there is not a definite solution to this problem, modifications in diet and physical activity will likely decrease the occurrence in our youth. Therefore more primary preventative measures, community and private, need to implemented in order to reduce the prevalence of obesity and improve the health and fitness of America’s adolescents. 25 METHODS Summary of methods This study is a retrospective efficacy study that focused on children’s’ health and physical fitness outcomes after an eight-week health and wellness intervention. Participants Participants were recruited into this program through nurse/doctor referrals, fliers at schools, publications in newspapers, and word of mouth. Most importantly there was no cost associated with this program, which attracted many families to register. The children and their families were primarily from the Arden-Arcade area, a suburb of Sacramento. The majority of these families were low to middle class and qualify for free or reduced lunch. 100 boys and girls ages eight to 15 years old signed up for Project HYPE in the summer of 2012 but, only 45 (23 boys, 22 girls) participants completed the eight-weeks of HYPE-intervention. The high dropout rate was caused by family vacations, children going back to school, and a lack of interest in the program. Since this program was free, some families took advantage of this and decided to withdraw their children at their own convenience. The data used in this study will only include the 45 participants who finished the eight-weeks. The boys’ mean age was 10.9 ±2.39 while the girls’ mean age was 10.3 ±2.07. BMI was calculated using CDC’s (2002) Growth Charts for the United States: Methods and Development, which took into account each participant’s age, height and weight. BMI for the boys was 20.7±5.21 while the mean BMI for girls was 22.5±6.97. Out of all the participants, 19 boys and 14 girls were considered healthy weight (BMI ranging from 5th to 85th percentile) and four boys and six 26 girls were considered obese (BMI equal to or greater than 95th percentile). No children were classified as overweight (BMI ranging from 85th to 95th percentile), which indicates that the majority of the children generally had a normal BMI with some that were classified as obese. As for blood pressure, the children’s measurements were compared with the U.S. Department of Health and Human Services blood pressure normative values to determine their risk level (2005). 19 boys were classified as having a normal blood pressure and four boys were classified as prehypertensive, while 18 girls were classified as having a normal blood pressure and three girls were classified as prehypertensive. The children are also untrained at resistance training and are in good health with no serious contraindications to physical activity. Some children had chronic health conditions such as diabetes and high blood pressure and were required to obtain physician approval before starting the program. The participants also signed waivers, which detailed the risks and benefits of physical activity. There are four groups in this study: Pre-HYPE boys, Pre-HYPE girls, Post-HYPE boys and Post-HYPE girls. Instruments The exercise testing data was collected in the summer of 2012, and the instruments used to collect the data were correctly calibrated and functional. Calibrated weight scales, tape measures, blood pressure cuffs and height scales were used to record resting vitals. The Pacer Test to measure muscular endurance was administered with a Pacer Test CD, which contained predetermined beeps for the participants to follow and the 20 meters was measured with a measuring tape. Sacramento State Kinesiology and 27 Nursing interns were trained before exercise testing and followed the Cooper Institute’s Exercise Testing Procedures correctly. Procedures Sacramento State Kinesiology and Nursing interns collected the 2012 pre and post exercise testing data. The first Tuesday of the program and the last Tuesday of the program were the exercise testing dates (week one and week eight). Exercise testing lasted approximately two and a half hours for all participants. Participants were instructed to avoid strenuous activity the day before and to restrain from physical activity in the morning of exercise testing. Participants were encouraged by volunteers and staff to eat a healthy breakfast before the test. They were also instructed to follow the procedures and at any time; if they did not feel comfortable exercising they could withdraw from exercise and rest. On the day of exercise testing, participants’ resting vitals were collected and afterwards they were divided into groups of five to eight with seven interns monitoring each group. Before the start of each test, participants were given a familiarization trial so they could understand the procedures of each test. After the familiarization trials, the Pacer Test was administered first. The participants were instructed to keep with the pace with the calibrated beep. A completed stage was if the participant completed the 20 meters before the beep sounded and if a participant missed a beep, they had one chance to make the next beep or else the last beep would be recorded as their final score. After they completed the Pacer Test, the participants underwent maximal push-up test to determine their muscular endurance. Participants were instructed to perform as many push-ups with correct form (elbows at 90 degrees, knees 28 extended and off the ground, back straight and not arched). A push-up only counted if the participants followed the procedures and if the knees hit the ground or volitional fatigue, the test ended. Interns collected this data with pencils and paper and recorded the data on an excel spreadsheet. The eight-week HYPE-intervention consisted of structured exercises, nutritional education and mandatory family nights. Structured exercise included recreation activities such as capture the flag, dodge ball and various tag games, which lasted a total of two and a half hours per day. Participants were divided into smaller groups during these recreation games and were encouraged to participate with program leaders and interns. An incentive to exercise included raffle tickets which were handed out to participants who were actively engaged during the day. Raffle tickets were collected at the end of the day and prizes were handed out to participants with raffle tickets at family nights. Weekly field trips were also implemented which include walking field trips to farmers markets and a local high school gym. Resistance exercise was incorporated as the participants engaged in free weight exercises, dumbbell exercises and resistance band exercises. The guidelines for resistance training utilized from ACSM’s Guidelines for Exercise Testing and Prescription, 8th Edition (2009). Repetitions per exercise ranged from 10-15, two to three sets, and a total body training approach was implemented (See Appendix B for more information). Participants engaged in resistance exercise three times a week for one hour and participated in other exercises the remainder of the week. Group fitness classes such as boxing, kickboxing, salsa, and dance were also taught to the participants on an average of two hours per week. Children who participated in these 29 recreations activities are estimated to have MET (metabolic equivalent) values ranging from three to six, which indicates moderate exercise (ACSM, 2009). On some harder activities such as walking field trips, resistance training and exercise testing the METs value is estimated to be over six, which indicates strenuous physical activity (2009). Nutrition education consisted of splitting the kids into two groups; boys and girls ages six to 10 and boys and girls ages 10-15. Interns taught the two groups food categories, MyPyramid, MyPlate, and recommendations from the USDA on healthy food consumption. Nutrition education was twice a week for one and a half hour sessions. Cooking demonstrations and diet consultations were also implemented during the eightweeks. Finally, participants and their parents had to attend five mandatory family night sessions throughout the eight-weeks. The family nights lasted two hours long and consisted of nutrition education, physical activity, and cooking lessons. The goal of family nights were to keep the parents involved in the children’s’ daily curriculum and reinforce health and wellness ideas and concepts to the parents. If parents missed two or more family nights they and their children would be dismissed from the program. Incentives to attend family night included free food, prizes and other fun recreational activities. All interns were adequately trained and instructed on how to lead these exercise activities, nutrition lessons and family nights before the start of the program. Design and analysis The design of this study will look at a HYPE-intervention exercise testing data set from the summer of 2012 and to determine if participants improved significantly upon health related and physical fitness outcomes at the end of the eight-weeks. The health 30 related outcomes that we will be observing include pre/post BMI and blood pressure values. The fitness related outcomes that will be analyzed include pre/post push-up and Pacer Score values. In analyzing the pre-HYPE intervention and post-HYPE intervention values, a paired t-test will be used on the means of the boys and girls pre-summer and postsummer. A paired t-test determines the significance in the changes of the dependent variable. In this study, the independent variable is the health and wellness intervention and the dependent variable is the health and fitness outcomes after the intervention. If their health and fitness variables improve significantly (P<.05) then the Cooper Institute’s FITNESSGRAM® Standards will be used as a baseline to categorize their health. The FITNESSGRAM® Standards lists fitness norms for the Pacer Test, Push-up test and BMI and categorizes children as in the Healthy Fitness Zone or Not-Healthy Fitness Zone based on their performance. In analyzing blood pressure, the U.S. Department of Health and Human Services has established healthy blood pressure values for children ages one to 17 based on their age, height and weight. In order to determine if they have significantly improved their blood pressure, their pre-intervention values will be compared with their post-intervention values. However, if participants do not improve their health and fitness variables then there will be no need to use the FITNESSGRAM® Healthy Fitness Zone or U.S. Department of Health and Human Services standards. Ethical Considerations Participants in the HYPE program were informed of the exercise testing protocol during the orientation meeting before the start of the program and also were educated on 31 what the risks and benefits of exercise. The families and their children understood that participation in the program was voluntary and that they could withdraw from the program at any time. During exercise testing, participants were instructed to stop exercising if they felt overly exhausted, light headed, or nauseous. Participant’s data will remain confidential in which only the researchers in this study will have access to the data. In addition, the data being analyzed is past data from the Summer of 2012. This study is not currently looking at children at the present which causes no harm to others. IRB has been approved and this study is deemed as no risk. Internal Validity Internal validity represents to how well the study was run and how confident one can conclude that the change in the dependent variable was caused by the independent variable and not extraneous ones. In this study, the dependent variable is health and fitness outcomes and the independent variable is health and wellness intervention. To be sure that the potential health improvements were caused solely by the independent variable, some extraneous variables were controlled to protect this experiment’s internal validity. First, the length of the study was only eight-weeks. Longer studies usually take more repeated measurements over time and the participants are more likely to be affected by history variables as opposed to participants in a shorter study. Secondly, the interns who collected the data used the same instrumentation for the pre-test and post-test during exercise testing. The equipment was correctly calibrated and the interns were properly trained on how to collect the data. Thirdly, the subjects were divided into groups of boys 32 and girls. This allowed the groups to be functionally equivalent at the beginning and end of the study. Finally, this study will only use data from participants that completed the eight-week program and attended both pre/post exercise testing sessions. External Validity External validity is the extent to which a study’s results can be applied to other people or settings. In this study, randomization was not needed since there were two groups and all participants underwent the same treatment. Multiple treatments or interventions have a limited generalizability and can have an adverse effect on a subject’s performance. However, this study is exempt from this notion since there was only one intervention. 33 RESULTS Introduction The purpose of this study is to observe the changes in fitness and health outcomes in children ages eight to 15 after an eight-week long health and wellness intervention program. Exercise testing data was collected pre-intervention and post-intervention, which included Body Mass Index (BMI), systolic and diastolic blood pressure, cardiovascular and muscular endurance. A paired t-test was utilized to compare the changes in the adolescents’ health and fitness outcomes the after the intervention program (P<.05). Summary of Results In health outcomes, the boys’ BMI increased by 1.9kg/m2 (P =.16) and systolic blood pressure was lowered significantly by 3.4 mmHg (P =.04) while diastolic blood pressure decreased by 2.68mmHg (P =.06). The girls’ BMI increased by .2kg/m2 (P =.16) and their systolic blood pressure increased by 2.8mmHg (P =.27) while their diastolic blood pressure increased significantly by 5.91mmHg (P =.03). In fitness outcomes, the boys improved significantly on their muscular endurance by 12.8% (P =.00001) and cardiovascular endurance by 18.90% (P =.0068) while the girls improved significantly on their muscular endurance by 42.60% (P =5.1 E-09) and cardiovascular endurance by 24.50% (.P =0013). Statistical Analysis Paired t-tests were used to determine if significant changes in pre and post fitness and health outcomes occurred after a health and wellness program intervention. In this 34 study, the participants’ data (boys and girls exercise testing data) were tested twice with the same variable (health and fitness outcomes) in order to determine the change between the two sets. Paired t-test were used to determine if the changes observed in the exercise testing data were statistically significant for both girls and boys. This study utilized Microsoft Excel 2007 to record the data into spreadsheets and run the t-test calculations. In order to establish confidence in the statistical findings, P-value was set at <.05 for all tests. 35 Table 1 Participant demographics Gender Boys (N=23) Girls (N=22) Average BMI 20.7±5.21 21.3±6.97 Normal 19 (82.6%) 18 (81.8%) 0 0 4 (17.4%) 4 (18.2%) Systolic 111.4±14.0 mmHg 104.6±16.9 mmHg Diastolic 69.1±10.2 mmHg 60.1±11.5 mmHg Normal category** 16 (69.5%) 18 (81.8%) Prehypertensive category** 5 (21.7%) 2 (9.1%) Stage 1 hypertension category** 2 (.086%) 2 (9.1%) Average push-up score 18.4±12.2 8.36±5.31 Met Cooper Institute’s standards*** 19 (82.6%) 18 (81.8%) Did not meet standards*** 4 (17.4%) 4 (18.2%) Average shuttle run/pacer score 21.2±14.9 12.3±5.94 Met Cooper Institute’s standards*** 2 (8.70%) 3 (13.6%) Did not meet standards*** 21 (91.3%) 19 (86.4%) BMI* (kg/m2) Overweight Obese Resting blood pressure Cooper Institute push-up test Cooper Institute shuttle run/pacer score *CDC Growth Charts and Development for the United States, 2010 **The Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents, 2007 ***FITNESSGRAM® Healthy Fitness Zones, 2009 36 Table 1 presents the demographics of the participants who completed all eightweeks of the HYPE program. This table lists their BMI, resting blood pressure, maximal push-up score and pacer score. Table 2 Boys’ health outcomes: pre and post HYPE intervention Groups Pre-(n=23) Post-(n=23) P-value 20.7±5.21 22.6±6.70 .1606 Systolic 111.4±14.0 mmHg 108.0±13.0 mmHg .0468 Diastolic 69.13±10.2 mmHg 66.45±11.3 mmHg .0600 BMI (kg/m2) Blood Pressure Table 2 presents the boys’ change in BMI and blood pressure after the eight-week intervention. Their BMI increased but not significantly, while systolic blood pressure significantly decreased (p=.0468) and diastolic blood pressure decreased but, not significantly. 37 Table 3 Girls’ health outcomes: pre and post HYPE intervention Groups Pre-(n=22) Post-(n=22) P-value 21.3±6.97 21.5±6.93 .1013 Systolic 104.6±16.9 mmHg 107.4±15.0 mmHg .2738 Diastolic 60.09±11.5 mmHg 66.00±11.9 mmHg .0314 BMI (kg/m2) Blood Pressure Table 3 presents the girls’ change in BMI and blood pressure after the eight-week intervention. Their BMI slightly increased after the intervention, while systolic blood pressure increased but not significantly and diastolic blood pressure increased significantly (p=.0314). Table 4 Boys’ fitness outcomes: pre and post HYPE intervention Groups Pre-(n=23) Post-(n=23) P-value Cooper institute push-up test 18.4±12.2 reps 21.1±13.6 reps .0001 Cooper Institute shuttle run/pacer score 17.2±11.1 laps 21.2±14.9 laps .0068 Table 4 presents the boys’ change maximal push-up score and pacer score after the eight-week intervention. Their push-up scores increased significantly (p=.0001) by 12.8% and their pacer score increased significantly (p=.0068) by 18.9%. 38 Table 5 Girls’ fitness outcomes: pre and post HYPE intervention Groups Pre-(n=22) Post-(n=22) P-value Cooper Institute push-up test 8.36±5.31 reps 14.5±6.81 reps 5.11E-09 Cooper Institute shuttle run/pacer score 12.3±5.94 laps 16.3±6.44 laps .0013 Table 5 presents the girls’ change maximal push-up score and pacer score after the eight-week intervention. Their push-up scores increased significantly (p=.5.11 E-09) by 42.6% and their pacer score increased significantly (p=.0013) by 24.5%. Table 6 Comparison of boys’ data with FITNESSGRAM®’s Healthy Fitness Zone criteria Groups Pre-(n=23) Post-(n=23) Met standards* 19 22 Did not meet standards* 4 1 Met standards* 2 7 Did not meet standards* 21 16 2 7 Push-up test Pacer test Healthy Fitness Zone* (met pacer and push-up standards) *FITNESSGRAM® Healthy Fitness Zones, 2009 39 Table 6 compares the boys’ exercise testing results with FITNESSGRAM®’s Healthy Fitness Zone criteria. Two boys met the Healthy Fitness Zone criteria during pre-intervention testing and after the eight-weeks, seven boys met the Healthy Fitness Zone. This is an increase of five additional participants, or an increase of 250%. Table 7 Comparison of girls’ data with FITNESSGRAM®’s Healthy Fitness Zone criteria Groups Pre-(n=22) Post-(n=22) 18 22 4 0 Met standards* 3 11 Did not meet standards* 19 11 3 11 Push-up test Met standards* Did not meet standards* Pacer test Healthy Fitness Zone* (met both pacer and (push-up standards *FITNESSGRAM® Healthy Fitness Zones, 2009 Table 7 compares the girls’ exercise testing results with FITNESSGRAM®’s Healthy Fitness Zone criteria. Three girls met the Healthy Fitness Zone criteria during pre-intervention testing and after the eight-weeks, 11 girls met the Healthy Fitness Zone. This is an increase of eight additional participants, or an increase of 266%. 40 Table 8 Comparison of all participants’ data with FITNESSGRAM®’s Healthy Fitness Zone criteria Groups Healthy Fitness Zone* (met both pacer and push-up standards) Pre-(n=55) Post-(n=55) 5 18 *FITNESSGRAM® Healthy Fitness Zones, 2009 Table 8 summarizes all participants meeting the Healthy Fitness Zone during the pre-intervention and post-intervention testing. During the beginning of the program, only five participants met this criterion. After the intervention, 18 participants met these criteria. This is an increase of 13 participants, or an increase of 260%. The results indicate that the participants improved significantly on the fitness outcomes of muscular endurance and cardiovascular endurance while BMI remained the same and blood pressure changed significantly over the eight-week program. Further discussion of these results will be explored in the next section. 41 DISCUSSION Introduction Primary prevention programs have shown promise in decreasing the prevalence of obesity and improving physical fitness outcomes (Manger et al., 2012). Key components of these programs include diet analysis and counseling, structured exercise sessions and group therapy sessions with a trained professional. However, the effectiveness of these programs has not been studied in depth. Therefore, the purpose of this study is to investigate the effectiveness of Project HYPE, an eight-week long health and wellness program for children ages eight to 15. In this study, we have examined health and fitness outcomes of the participants before and after the intervention. Before the start of the program, 100 boys and girls participated in exercise testing which included obtaining BMI, resting blood pressure, and Pacer Test and Maximal push-up test scores. Afterwards, the eight-week intervention included structure exercise, recreation games and nutritional counseling for the children and their parents. After the intervention, exercise testing was implemented on the children that remained during the eight-weeks (n=55) and their data were analyzed for its effectiveness. The Cooper Institute’s Healthy Fitness Zone, a guideline of health and fitness norms for children, was used to analyze the results of the participant’s after the intervention to determine the extent of improvement. Health outcomes In health outcomes, this study’s hypothesis stated that there would be a significant reduction (P<.05) in the children’s BMI and systolic/diastolic blood pressure after the intervention. The results indicate that after the intervention there was a slight increase in 42 BMI for boys and girls (P=.10, P=.16) and divergent blood pressure responses with boys decreasing their systolic blood pressure by 3.05% and diastolic blood pressure by 3.88%, while girls increasing their systolic blood pressure by 2.67% and diastolic blood pressure by 9.84%. There are many interpretations to why BMI slightly increased even with the health and wellness intervention. First off, the pre-intervention BMI of the participants ranged from the 5th to 85th percentile with boys’ mean BMI = 20.7±5.21 and girls’ mean BMI = 21.3±6.93. This indicated that the children were at a healthy weight to start the program and consequently their risk level for developing chronic diseases such as type II diabetes, heart disease, and cancer was classified as low (CDC Overweight and obesity, 2011). After the eight-weeks, their BMI increased slightly, boys’ mean BMI = 22.6±6.70 and girls’ mean BMI = 21.5±6.93. However, their BMI still fell within the healthy percentile of 5th to 85th, indicating little to no risk as group post-intervention. Since their BMI did not significantly increase during the intervention period and their BMI remained in the classification of healthy weight, this program has shown effectiveness in maintaining BMI and preventing the onset of overweight and obesity in children. Secondly, a slight increase in BMI can be interpreted as a positive indication if the participants underwent pubertal growth during the eight-weeks. Studies indicate that maturation starts at the age of 11 years in girls and 13 years in boys (Clark, Roemmich, & Rogol, 2000). The girls’ age averaged 10.9 ±2.39 while the boys’ age averaged 10.3±2.07, which represents the early onset of puberty in many of the participants. During pubertal growth, youth can expect a drastic change in body composition; boys 43 increase lean muscle mass and decrease fat mass while girls increase lean muscle mass but also fat mass (Clark et al., 2000). Due to the change in body composition, it is estimated that puberty can cause significant weight gain; 50% of adult body weight is gained during adolescence (Clark et al., 2000). However, after the eight-weeks the boys only increased their BMI by 9.18% and girls increased by .939%. In comparison, peak growth for boys averages 9kg/year and 8.3kg/year for girls (Flegal, Wei, & Ogden, 2002). Consequently, the participants maintained a healthy weight during the eightweeks even when considering maturation as a cause of significant weight gain. Thirdly and lastly, BMI should not be the only factor in assessing if a child has underwent positive health changes. BMI is a useful tool to access the health of an individual, but it should not be the only factor in determining if an individual is healthy. In a recent health and wellness intervention study, researchers observed that children obtained significant benefits in health parameters such as waist circumference, cardiovascular endurance, physical activity, and self-esteem independent of the change in BMI (Kolotorou et al., 2013). This study illustrated that participants were more active and less sedentary, ate healthier and consumed less processed foods, and reduced their cardiovascular risk factors even though BMI stayed the same or did not significantly change (Kolotorou et al., 2013). Similarly, even though BMI stayed the same in this study, the participants’ muscular and cardiovascular endurance improved significantly, which indicates this program showed effectiveness in improving fitness outcomes in youth. Consequently, assessing the change in BMI alone is not sufficient in determining the success of a health and wellness intervention. 44 In analyzing the changes in blood pressure, the decrease in the boys’ systolic and diastolic blood pressure (3.05% and 3.88%) can be explained by the increase in physical activity and exercise during the eight-week intervention. The participants engaged in moderate (three to six METS) to intense (six METS and higher) physical activity daily during the intervention. Many studies illustrate that increasing physical activity improves cardiovascular health and fitness and if sustained for an extended duration can lead to a decrease in resting heart rate and blood pressure in adolescents and adults (Torrance, Mcguire, Lewanczuk, & McGavock, 2007). Studies also indicate that along with exercise, reducing the amount of sodium in the diet can lower blood pressure up to 10 mmHg (Ribeiro, Silva, & Santos, 2005). During the intervention, the participants were instructed to eat less processed foods and increase their consumption of whole grains, lean meats and vegetables (see Appendix A). The participants were also given educational handouts, which offered suggestions on healthy food to eat and food to avoid. In summary, the increased physical activity and nutritional education lessons can explain the decrease in blood pressure for boys. On the contrary, the increased systolic and diastolic blood pressure values for girls (2.67% and 9.84%) can be explained by girls’ maturation, exercise intensity and poor exercise testing procedures. In a recent study by Shankar et al, researchers discovered that pubertal growth increases females’ systolic blood pressure two to four times faster when compared to pre-pubertal growth (2005). The increase in blood pressure is associated with the rapid increase in physical growth due to puberty. Since a majority of the female participants were in the age range for pubertal growth, maturation 45 could be one explanation to the increase in blood pressure. Also during the program, the girls participated in exercise but it was not very vigorous when compared to boys. Since decreases in blood pressure are associated with exercise intensity, the girls’ increase in blood pressure can be explained by their low exercise intensity during active activities. Finally, poor exercise testing procedures can explain the increase in blood pressure. Due to a budget shortfall, this program did not have same models of blood pressure monitors—the blood pressure monitors were of different brand and different sizes. The interns who were collecting the blood pressure were instructed to use the same blood pressure monitors on the same participants’ pre and post intervention, but some interns did not follow this protocol. This resulted in different blood pressure monitors being on participants during pre and post exercise testing. The interns who collected the blood pressure pre-intervention were not the same for post-intervention, and this could have caused an error in data collection. In addition, some of the cuffs were too big for the children’s arms, which could cause variations in blood pressure readings. The boys and girls sometimes played games immediately before the exercise testing session and this could result in a fluctuation in blood pressure. It should be noted that the same errors during the collection of blood pressure for girls can be applied to the collection of boys’ blood pressure as well since inappropriate cuff size can cause under or over-reporting of measurements. Therefore, the reduced blood pressure for the boys should be taken with caution due to poor collection methods and procedures. 46 In summary, since there was not a significant decrease (P<.05) in the participants’ BMI or boys’ (increase of 3.05% and 3.88%) and girls’ (decrease of 2.67% and 9.84%) systolic and diastolic blood pressure, this study’s first hypothesis is rejected. Fitness outcomes In fitness outcomes, this study hypothesized that after the intervention cardiovascular and muscular endurance would improve significantly (P<.05). The results indicated that there was significant improvement in muscular endurance by 12.8% and 42.6% (P=.001, P=5.1 E-09) and cardiovascular endurance by 18.9% and 24.5% (P=.00001, P=.0006) in both boys and girls. These improvements have been compared to FITNESSGRAM®’s Healthy Fitness Zone. The drastic improvements in these fitness variables may be attributed to the increased physical activity during the intervention. The design of this intervention’s exercise program was modeled after ACSM’s “F.I.T.T. (frequency, intensity, type, time) Principle of Exercise” (2009). The type of physical activity included structured exercise that consisted of weightlifting with dumbbells and body bars, relays, and group fitness classes such as yoga, kickboxing, and dance. During resistance training, participants were instructed to perform a total body training approach two to three times a week with 10-15 repetitions, two to three reps per exercise and lifting at 50-65% of one repetition max (see Appendix B for more information). Recreation activities such as tag games, capture the flag, and kick the can were also implemented along with the structured activity. There were also special fitness field trips such as scavenger hunts, nature walks, bike riding, and swimming meets. The intensity of these exercises ranged from moderate 47 (three to six METS for recreational activity) to vigorous (six METS and higher for structured activity) (ACSM, 2009). Participants exercised daily and on average, the amount of physical activity totaled to over 150 minutes per day, exceeding ACSM’s recommended amount of 60 minutes (2009). During exercise sessions participants bonded with staff and other participants which made these sessions enjoyable and fun. Participants were also encouraged to exercise outside of the program with their families in activities such as walking and biking. Similarly, in a recent study that observed physical fitness outcomes after a health and wellness intervention, researchers discovered an increase in Pacer Test scores and Maximal Push-up scores after the intervention period (Reed, Maslow, Long, & Hughey, 2013). This study observed children from grades 2nd to 8th for eight months, with one control group and one exercise intervention group. The exercise intervention group participated in moderate to physical activity five days a week for 45 minutes over the eight-month period, while the control group participated in only one day of physical activity for 45 minutes. A pre-test and post-test was administered before and after the program and the results indicate that the exercise intervention group improved significantly by 12.5% (P=.01) in their push-up scores and 18.7% (P=.0001) in their pacer after eight-months while the control group showed little to no improvement (Reed et al., 2013). In comparison, this study’s’ participants improved their push-up repetitions and pacer score by an average of 27.7% and 21.7% in eight-weeks. Therefore, intervention programs that focus on increasing physical activity in youth can significantly improve fitness outcomes. 48 In addition to increasing their type, time, duration and intensity of physical activity, the participants were educated on the importance of exercise during weekly wellness education sessions. These sessions consisted of power point lectures and group discussions on the importance of exercise and its associated health benefits. Participants were encouraged to participate during these discussion and handouts summarizing the lectures were distributed after the hour-long session. The importance of exercise was also discussed during family nights and parents were given handouts after these sessions as well. Mustard Seed Spin, a non-profit organization that promotes total wellness for youth through safe cycling, held a two-day educational seminar and bike field trip day for the HYPE participants. The first day explained bike safety and bike maintenance, while the second day the participants rode to Sacramento State University and rode along the American River. At the end of the field trip, eight bikes were given to low-income children and all participants received free helmets to wear. The purpose of this two-day event was to encourage participants to exercise through participating in cycling activities outside of the intervention program. The Cooper Institute’s Healthy Fitness Zone sets standards of fitness and health for children. Before the intervention, five participants met both muscular and cardiovascular endurance standards and were classified in the Healthy Fitness Zone. After the intervention, 18 participants were classified in the Healthy Fitness Zone, an increase of 260%. In summary, the increased physical activity, structured exercise, and fitness education during the intervention period are the most likely factors to have caused the improvements in the participants’ physical fitness. 49 Since there was a significant increase (P<.05) in the fitness outcomes of muscular and cardiovascular endurance, this study’s second hypothesis is accepted. Attendance and dropout Before the start of intervention, over 100 participants registered for this program. However, after eight-weeks only 45 participants finished the program and this indicates a 55% dropout rate and a 45% completion rate (see Appendix C for attendance records). There were five family nights during the eight-weeks and attendance decreased from 80 families attending the first family night to 32 families attending the last family night, which indicates a 60% dropout rate and 40% completion rate (see Appendix C for attendance records). The participants informed staff that the reasons behind dropping out of the program included transportation, start of the school year, vacation, scheduling conflicts, and a lack of interest. Other similar health and wellness programs have shown retention rates of 60% and 62% after 12 months of intervention that included nutrition education, exercise prescription and counseling (Savoye, Nowicka, & Dziura, 2011). The most common reasoning behind the dropouts in these studies were the lack of interest from the participants. Methods to improve the completion rate and retention of the HYPE program include incentives and prizes for attending program and requiring the families to sign commitment pledges before the start of the intervention. In addition, the studies with the high retention rates utilized weekly telephonic counseling sessions and monetary incentives while this program did not (Savoye et al., 2011). 50 Recommendations One area that needed improvement was the nutrition education sessions for participants and their parents. Through antidotal observation by staff, interns and Program Coordinator, both children and parents were confused at the material which caused them to not take the sessions seriously (see Appendix D for more detail). The hour-long sessions included dietary analysis and guidelines for healthy eating but, both children and parents seemed disinterested and bored at what they were learning. Some of the children did not have the intellectual capacity to understand the nutritional terms and concepts during these sessions. One intern reported multiple participants struggling to read and write complete sentences when attempting to complete the nutritional worksheets. Due to the participants living in urban and rural areas, these children were reading and writing far below their grade level. Many times the interns who were leading these sessions had to stop and give these participants one on one attention that became time consuming. Some children also had problems sitting still and difficulty concentrating which caused distractions in the teaching environment since they wanted to go out and play rather than sit still and learn. Similarly, the parents mostly came from low-income neighborhoods, which suggest that their education level did not exceed more than a high school diploma. This resulted in the parents having little comprehension of the material and led to disinterest during the meetings—some parents were texting and playing games on their phones during these sessions. These nutritional meetings were also set at 6pm and parents appeared exhausted and drained since they had work before they arrived to these meetings. As a result, the dietary and nutritional counseling may not 51 have been very effective due to participants’ lack of understanding and disinterest of the material. There are various methods to increase comprehension and participation in the nutritional counseling sessions (see Appendix D for more information). One example to increase comprehension would be to divide these sessions into smaller segments with smaller groups. The sessions originally lasted one hour and the participants appeared exhausted and tired 30 minutes into the session. With such a large group of 20 participants, it was difficult to get through the lesson plan without distractions. Goldstone et al (2005) suggest small groups with peer interaction keeps participants focused and alert throughout the whole session and assists with retention and transfer of the material as well. A smaller group also allows for more one on one counseling with the instructors, which helps with clarifying the concepts and promotes discussion of the material. The interns who led these sessions had little to no experience in teaching this material which contributed to the lack of comprehension from the families. In order to facilitate group learning, Dunlosky et al (2013) recommend learning techniques such rereading, practice testing, highlighting, and using mnemonics to grasp the material effectively. In addition, participants should complete take home worksheets and homework so they are accountable for the material. These worksheets outside of class will help reinforce ideas and concepts and participants will improve on comprehension of the material since they are studying at their own time and pace. Finally, in order to promote interest parents and children who are involved in the program should receive 52 incentives such as prizes and gifts. This will help motivate participants to become an active learner and engage in these sessions rather than becoming disinterested and bored. Recommendations for program quality Participants asked for more field trips during the program. Due to lack of funds, the staff could only lead participants in field trips that were low to no cost that included walking field trips and scavenger hunts. Participants wanted to go camping, visit baseball games, training facilities, and Sacramento State’s fitness and recreation facility, The WELL. Although field trips do not directly affect health and wellness outcomes, more field trips that are exciting will help keep the participants interested, which in turn improve retention and completion rates. Unfortunately, this program did not have the financial means to pay for these trips. Suggestions to raise money for these field trips include fundraising events and applying for grants. Participants also wanted to try new exercise equipment. This program had resistance bands and free weight dumbbells, but the participants wanted to try new equipment. Participants mentioned to staff that they would like to try new equipment such as parachutes, plyometric boxes, and bosu balls. Due to a lack of funds, this program did not have the financial means to purchase this new equipment. Most of the participants in this program were of normal, healthy body mass index. This program was catered for overweight and obese children and their families, but unfortunately more normal weight children entered the program than overweight and obese children. In order to recruit more at risk youth, this program should coordinate 53 with local doctors and nurses to refer children who may be at risk for obesity and other chronic diseases into this intervention program. Recommendations for data collection To improve the accuracy of blood pressure readings, this program should purchase new blood pressure monitors of the same brand and model. These blood pressure models should be tailored towards children to ensure proper fitment of the cuff. In addition, interns who are collecting the blood pressure readings should make sure to use the same blood pressure monitor for each participant and the same intern should perform the reading pre and post intervention. The children should also rest before the readings to ensure accuracy. All of these recommendations should allow for better accuracy of blood pressure readings. In addition to collecting BMI, this program should perform a blood panel test on all participants pre and post intervention. A blood panel test measures fasting glucose and lipid profiles, which offer more insight on the health of the participant. These tests will also show the extent of change in a participant after health and wellness intervention. The Pacer Test and Maximal Push-up Test are good indicators of physical fitness, but flexibility, trunk endurance and pull-ups/dead hang from a pull-up bar were not measured in this study. The combination of these tests will provide a clear illustration on if the participant has improved upon their physical fitness. This study also did not measure body composition, which determines the change in fat mass or lean body mass. Determining if the participant has increased or decreased their body composition can analyze the program’s effectiveness in improving health outcomes. Suggested methods 54 of obtaining accurate body composition include hydrostatic weighing and DEXA full body scans. Summary The decline in the health and fitness of America’s youth will continue to be a huge problem for years to come. Primary prevention programs are one method to help combat this epidemic. The results of this study indicate that Project HYPE, a youth health and wellness intervention program, has shown promising results in helping its participants maintain a healthy weight and significantly improving fitness outcomes in low-income children ages eight to 15. 55 APPENDIX A: NUTRITION CURRICULUM 56 APPENDIX A: NUTRITION CURRICULUM 57 APPENDIX B: FITNESS CURRICULUM 58 APPENDIX B: FITNESS CURRICULUM 59 APPENDIX B: FITNESS CURRICULUM 60 APPENDIX B: FITNESS CURRICULUM 61 APPENDIX B: FITNESS CURRICULUM 62 APPENDIX C: SUMMARY OF ATTENDANCE 63 APPENDIX C: SUMMARY OF ATTENDANCE 64 APPENDIX D: PROGRAM EVALUATION 65 APPENDIX D: PROGRAM EVALUATION 66 APPENDIX D: PROGRAM EVALUATION 67 APPENDIX D: PROGRAM EVALUATION 68 REFERENCES ACSM. (2009). Acsm's guidelines for exercise testing and prescription. (8th ed.). Lippincott Williams & Wilkins. Brownson, R.C., Boehmer, T.K., & Luke, D.A. (2005). Declining rates of physical Activity in the United States: what are the contributors? Annual Review on Public Health,26, 41-43. California Endowment. (2007). Failing fitness: physical activity and physical education in schools. Retrieved from http://www.calendow.org/uploadedFiles/failing_fitness.pdf Caterson I.D., & Gill T.P. (2002). Obesity: epidemiology and possible prevention. Best Practices in Clinical Endocrinology Metabolism. 16, 595-610 CDC. (2002). CDC growth charts for the united states: Methods and development. Retrieved from http://www.cdc.gov/nchs/data/series/sr_11/sr11_246.pdf CDC, (2011). Children’s food environment state indicator report. CDC (2011). Childhood obesity facts. Retrieved from http://www.cdc.gov/healthyyouth/obesity/facts.htm CDC. (2011). Halting the epidemic by making health easier at a glance. Retrieved from http://www.cdc.gov/chronicdisease/resources/publications/AAG/obesity.htm CDC. (2011, April 26). Overweight and obesity. Retrieved from http://www.cdc.gov/obesity/childhood/basics.html 69 CDC. (2012). Vital signs: Food categories contributing the most to sodium consumption — united states, 2007–2008. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6105a3.htm CDC. (2013). Youth physical activity guidelines toolkit. Retrieved from http://www.cdc.gov/HealthyYouth/physicalactivity/guidelines.htm Clark, P., Roemmich, J., & Rogol, D. (2000) Growth and pubertal development in children and adolescents: effects of diet and physical activity. American Journal of Clinical Nutrition, 70(2) 521-528. Cooper Institute, (2007). FITNESSGRAM® Healthy Fitness Zones. Retrieved from http://cooperinstitute.org/fitnessgram Cruz ML, & Goran MI. (2004). The metabolic syndrome in children and adolescents. Current diabetes reports.. 4(1), 53-62 Dunlosky, J., Rawson, K., Marsh, E., Nathan M., & Willingham T., D. (2013). Improving students’ learning with effective learning techniques: promising directions from cognitive and educational psychology. Association for Psychological Science in the Public Interest. 14(1): 4-58. Flegal K.M., Wei R., & Ogden, C. (2002). Weight-for-stature compared with body mass index-for-age growth charts for the United States from the Centers for Disease Control and Prevention. American Journal of Clinical Nutrition, 75, 761-766 Gidding S., Lichtenstein, A., Faith, M., Karpyn, A., Mennella, J., Popkin B., Rowe J., Van Horn, L., & Whitsel, L. (2009). Implementing American heart association And pediatric adult nutrition guidelines. Circulation, 119, 1161-1175. 70 Goldstone, R.L., and Son, J.Y. (2005). The transfer of scientific principles using concrete and idealized simulations. The Journal of the Learning Sciences, 14, 69-110. Healthy People. (2012). Introducing healthy people 2020. Retrieved from http://www.healthypeople.gov/2020/default.aspx Hughes A. R., Henderson A., Ortiz-Rodriguez V., Artinou M.L., & Reilly J.J. (2006) Habitual physical activity and sedentary behavior in a clinical sample of obese children. International Journal of Obesity, 30, 1494–1500. Kolotorou, M., Radley D., Chadwick P., Smith L., Orfajos S., Venediktos K., Singhal A., Cole T., & Sacher P. (2013). Is BMI alone a sufficient outcome to evaluate interventions for child obesity? Childhood Obesity. 9(4), 350-356. Larson N., Story M., & Nelson M. (2009) Neighborhood environments: disparities in access to healthy foods in the U.S. American Journal of Preventative Medicine, 36(1):74-81. Lytle, L. (2012). Dealing with the childhood obesity epidemic: A public health approach. Abdominal Imaging, 37(5), 719-724. Mahshid, D., Noori, A., & Merchant, A. (2005). Childhood obesity, prevalence and prevention. Nutrition Journal, 4(24) Manger W., Manger, L., Minnko, A., Killmeyere, M., & Holzman, R. (2012). Obesity prevention in young schoolchildren: results of a pilot study. Journal of School Health, 82(10), 462-468. 71 National Center for Health Statistics. (2011). Special features on death and dying. U.S. Department of Health and Human Services. Narkiewicz, K. (2005). Obesity and hypertension—the issue is more complex than we thought. Nephrology Dialysis Transplantation, 21(2), 264-267. Retrieved from http://ndt.oxfordjournals.org/content/21/2/264.full Page A., Cooper A., Stamatakis E., Foster L., Crowne E., Sabin M., & Shield P.H. Physical activity patterns in nonobese and obese children assessed using minute-byminute accelerometry. International Journal of Obesity, 29, 1070–1076. doi:10.1038/sj.ijo.0802993. President's Council on Fitness, Sports & Nutrition. (2013). The nation's physical activity, fitness and nutrition program. Retrieved from https://www.presidentschallenge.org/ Poirier P., Giles T.D., Bray G.A., Hong Y., Stern J.S., Pi-Sunyer F.X., & Eckel R.H. (2006) Obesity and cardiovascular disease: pathophysiology, evaluation, and effects of weight loss: an update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity committee of the council on nutrition. Physical Activity and Metabolism,113, 898–918. Reed, J., Maslow, A., Long, S., & Hughey, M. (2013). Examining the impact of 45 minutes of daily physical education on cognitive ability, fitness performance, and body composition of African American youth. Journal of Physical Activity and Health, 10, 185-107. 72 Ribeiro M.M., Silva A.G., & Santos N.S. (2005) Diet and exercise training restore blood pressure and vasodilatory responses during physiological maneuvers in obese children. Circulation, 111, 1915–1923. Rideout V.J., Foehr U.G., & Roberts D.F. (2010) Generation of M2 Media in the Lives of 8-18 Year Olds. A Kaiser Family Foundation Study. Savoye, M. , Nowicka, P. , Shaw, M. , Yu, S. , & Dziura, J. (2011). Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics, 127(3), 402-410 Shannkar, R., Eckert, G., Saha, C., Tu, W., & Pratt, H. The change in blood pressure during pubertal growth. Journal of Clinical Endocrinology & Metabolism, 90 (1), 163-167. Sinaiko, A.R. (2012) Metabolic syndrome in children. Journal of Pediatrics. 88(4), 286288. Steinberger, J., Daniels, S., Eckel, R., Hayman, L., Lustig, R., McCrindle, B., & MietusSnyder, M. (2009). Progress and challenges in metabolic syndrome in children and adolescents. Circulation, 119, 628-647. Retrieved from http://circ.ahajournals.org/content/early/2009/01/12/CIRCULATIONAHA.108.19 1394 Torrance B, Mcguire K.A., Lewanczuk R., & McGavock, J. (2007). Overweight, physical activity and high blood pressure in children: a review of literature. Vascular Health and Risk Management, 3(1), 139-149. 73 U.S. Department of Health and Human Services. (2005). Diagnosis, treatment, and evaluation of high blood pressure in children and adolescents. Retrieved from http://www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.pdf U.S. Department of Health and Human Services. (2008). Physical Activity Guidelines for Americans. U.S. Department of Health and Human Services.