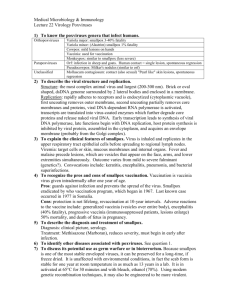
The History, Agents, and Potential Impact of Bioterrorism David Lakey, M. D.
advertisement

The History, Agents, and Potential Impact of Bioterrorism David Lakey, M. D. Associate Professor of Medicine Chief, Division of Infectious Disease Medical Director, CPIDC The University of Texas Health Center at Tyler The World Has Changed • • • • World Trade Center Anthrax We are at war Modern Molecular Biology Biological warfare vs. Bioterrorism • Biological warfare – Goal: – History: Kill a large number of soldiers Dates to the 6th Century BC • Bioterrorism – Goals • 1) kill a small number of people • 2) cause panic in the civilian population • 3) disrupt essential government agencies – History: the last 20 years Advantages of Biologics as Weapons • • • • • Infectious via aerosol Organisms fairly stable in environment Susceptible civilian populations High morbidity and mortality Person-to-person transmission (smallpox, plague, viral hemorrhagic fever) • Difficult to diagnose and/or treat • Previous development for BW Advantages of Biologics as Weapons • Easy to obtain • Inexpensive to produce • Potential for dissemination over large geographic area • Creates panic • Can overwhelm medical services • Perpetrators escape easily Vector, Russia – A large and sophisticated former bioweapons facility – In the early 1990s • 4,000-person • 30-building facility with ample biosafety level 4 laboratory facilities • Surrounded by electric fences • Protected by an elite guard • Housed the smallpox virus, Ebola, Marburg, and the hemorrhagic fever viruses – Autumn of 1997 • A half-empty facility • Protected by a handful of guards who had not been paid for months (P. Jahrling, pers. comm., 1998). • No one can say where the scientists have gone Henderson DA. Bioterrorism as a public health threat. Emerg Infect Dis 1998;4(3):488-92 Tokyo March 20 , 1995 • Two small bombs released the nerve gas Sarin in the subway during the morning rush hour • Tokyo fire department responded to a “bomb”. Many firemen were themselves harmed. • 5,510 people harmed, 12 die • Trial run by Aum Shinrikyo Aum Shinrikyo • Mission: End the world as we know it and place themselves in control • 40,000 devotees • Global (Japan, Russia, Europe and the United States) • Stockpile of Sarin enough kill 4.2 million people • Previous attacks included at least 2 prior gassings, several botulism toxin assaults, and attempts to kill Japan’s leader with anthrax • Attempted to acquire and develop Q fever and Ebola Salmonellosis Caused by Intentional Contamination The Dalles, Oregon in Fall of 1984 751 cases of Salmonella Eating at salad bars in 10 restaurants Criminal investigation identified perpetrators as followers of Bhagwan Shree Rajneesh SOURCE: Torok et al. JAMA 1997;278:389 Shigellosis Caused by Intentional Contamination Dallas, Texas in Fall of 1996 12 (27%) of 45 laboratory workers in a large medical center had severe diarrheal illness 8 (67%) had positive stool cultures for S. dysenteriae type 2 Risk Factor: Eating muffins or donuts in staff break room implicated DNA patterns indistinguishable for stool, muffin, and laboratory stock isolates SOURCE: Kolavic et al. JAMA 1997;278:396 Chemical & Biological Terrorism 1984: 1991: 1994: 1995: 1995: 1997: 1998: 1998: The Dalles, Oregon, Salmonella (salad bar) Minnesota, ricin toxin (hoax) Tokyo, Sarin and biological attacks Arkansas, ricin toxin (hoax) Ohio, Yersinia pestis (sent in mail) Washington DC, “Anthrax” (hoax) Nevada , non-lethal strain of B. anthracis Multiple “Anthrax” hoaxes 2001: Anthrax via mail CDC’s Category A Agents • • • • • • • High priority agents Pose a risk to national security Can be easily disseminated or transmitted Cause high mortality Major public health impact Public panic and social disruption Require special public health preparedness Category A Agents • • • • • • Anthrax Plague Smallpox Tularemia Botulinum toxin Viral Hemorrhagic Fevers Anthrax • Bacillus anthracis – A spore forming bacteria – Infects sheep, goats, and cattle – “woolsorter’s disease” • Three forms of Clinical Disease – Inhalational – Cutaneous – Gastrointestinal The Sverdlovsk Incident • 1979, Sverdlovsk, Soviet Union – City of 1 million people – Accidental aerosolization of anthrax spores from a microbiology facility – 79 cases of anthrax, 68 deaths • Lessons – – – – No deaths in patients with cutaneous anthrax Cases occurred 2 to 43 days after exposure No decontamination performed No further cases Cutaneous Anthrax • Deposition of spores on skin with previous cuts or abrasion • Initially local edema/swelling of infected area • Then an itchy bump, progressing to a blister • Finally a painless, depressed scab (eschar) • Untreated, mortality is 20% • Treated, mortality is about 0% Inhalation Anthrax • Initially non-specific “flulike” symptoms – Fever, fatigue, chest pain, muscle aches • Abrupt onset respiratory failure staring 2 to 4 days after presentation • Chest radiograph findings • Blood cultures are positive • Treatable in early stage Gastrointestinal Anthrax • Upper GI disease – – – – Oral or esophageal ulcer Regional enlargement of lymphnodes Edema Sepsis • Lower GI Disease – Nausea, vomiting, bloody diarrhea, acute abdomen Plague • Caused by the bacteria Yersinia pestis • About 10 cases of naturally occurring plague in US per year • Incubation period 2-3 days • Carried by fleas • Usually lymphnode or blood infection • Pneumonic plague if used by bioterrorist Plague Pneumonic Plague • Signs and symptoms – High fevers, chills, headache, coughing up blood, shortness of breath, toxic appearing • Diagnosis – Staining of sputum (safety pin Gram negative rod) • Isolation: Respiratory • Treatment: antibiotics (gentamicin, doxycyline, cipro) • Post exposure prophylaxis: antibiotics for 7 days Smallpox The History of Smallpox • Probably originated in agricultural settlements in NE Africa, China, or the Indus River Valley as early as 10,000 BC • Term “smallpox” was coined to differentiate the disease from the “Great Pox,” syphilis • Introduced in the New World by Spanish conquistadors, it decimated the local population, was instrumental in the fall of the Aztec and Inca empires • Boston (1901-03) epidemic, 1,596 cases and 270 deaths were reported Mummy of Pharaoh Ramesses V (d. 1157 BC) showing eruptions suggestive of smallpox The Global Eradication of Smallpox • Ali Maow Maalin, Somalia, 1977 • The world was declared free of smallpox in December 1979 • One of the greatest triumphs of public health • Routine vaccination stopped in the United States in 1972 Smallpox • Incubation period of 7 to 17 days • Clinical Presentation – Fatigue, headache, vomiting – Rash • Diagnosis: clinical • Isolation: Droplet and Airborne for 17 days • Treatment: ?cidofovir • Prognosis: 30 % mortality • Prophylaxis: – Vaccination within 7 days (live virus) – Vaccinia immune globulin Smallpox as a Biological Weapon • Smallpox was used as a biological weapon in 1763 during the Pontiac’s Rebellion in the FrenchIndian War • “You will do well to try to inoculate the Indians by means of [smallpox-infected] blankets, as well as to try every other method that can serve to extirpate this execrable race.” General Jeffrey Amherst in a letter to Colonel Henry Bouquet, July 1763 Smallpox as a Biological Weapon • Infectious, stable via aerosol • Small infectious dose, severe morbidity • Discontinuation of routine vaccination and large-scale vaccine production • Immunologically naïve population • Person-to-person transmission • Relatively simple production techniques • Recombinant technology: enhanced virulence Smallpox as a Biological Weapon 1972 Biological Weapons Convention Treaty: response to indiscriminate and unpredictable biological weapon research A signatory to the treaty, the Soviet Union conducted clandestine research for the next 20 years Kanatjan Alibekov, a Soviet biological weapons expert and defector, claimed that the Soviets manufactured 20 tons of smallpox Edward Jenner (1749-1823) • Jenner inoculated a boy with fluid taken from cowpox pustules and exposed him to smallpox several weeks later • “Vaccination,” the word Jenner coined (from the Latin vacca, for cow), was adopted by Pasteur for immunization against any disease Smallpox Vaccine Supply • 15.4 million doses of licensed vaccine • 85 million doses of frozen, not licensed • Total stockpile = 400 million doses • Frey SE, Couch RB, Tacket CO, et al. Clinical responses to undiluted and diluted smallpox vaccine. N Engl J Med 2002;346(17):1265-74 What is the Risk Benefit Ratio? Smallpox Vaccinia Botulinum Toxin • A protein produced by the bacteria Clostridium botulinum • Paralysis of facial muscles, and then respiratory muscles • Treatment – supportive care – antitoxin • No special isolation Laboratory Capacity for Botulinum Toxin Testing 1 1 1 1 2 2 1 1 1 11 1 1 1 1 1 1 Tularemia • • • • • • • Francisella tularensis Incubation period: 1 to 21 days Clinical: Skin, lymphnode or lung infections Diagnosis: blood tests (serology) Treatment (Gentamicin, Streptomycin) Standard isolation measures Mortality --- treated : low untreated: moderate • Persistence of organism ---months in moist soil Reported Cases of Tularemia - 1990-1998 Hemorrhagic Fever Viruses • Arenaviruses – – – – Argentine Hemorrhagic Fever Bolivian Hemorrhagic Fever Sabia Associated Hemorrhagic Fever Lassa Fever • Bunyaviruses – Crimean-Congo Hemorrhagic Fever – Rift Valley Fever – Hantavirus Pulmonary Syndrome Hemorrhagic Fever • Filoviruses – Ebola Hemorrhagic Fever – Marburg Hemorrhagic Fever • Flaviviruses – Tick-borne Encephalitis – Kyasanur Forest Disease – Omsk Hemorrhagic Fever Hemorrhagic Fever Viruses • Ebola, Marburg, Lassa fever, Dengue fever,etc • Produces microvascular damage • Fever, myalgia, hemorrhaging, shock • Mortality rate between 5 to 90%, depending on the virus • The antiviral medicine Ribavirin may be effective • No vaccine Ocular manifestations associated with hemorrhagic fever viruses range from conjunctival injection to subconjunctival hemorrhage, as seen in this patient. Reprinted with permission from Current Science/Current Medicine (Peters CJ, Zaki SR, Rollin PE. Viral hemorrhagic fevers. In: Fekety R, vol ed. Atlas of Infectious Diseases, Volume VIII. Philadelphia, Pa: Churchill, Livingstone; 1997:10.1-10.26). Modern Molecular Biology and Bioterrorism • Dual use technology – Aerosol technology that allows large insulin molecules to avoid the respiratory defense and be inhaled deep into lungs – Antibiotic resistance • Novel Pathogens • Synthetic viruses • Results are openly published with sufficient technical detail to allow duplication Cumulative Number of Reported Probable Cases of Severe Acute Respiratory Syndrome (SARS) Cases Deaths • • • • • • • • • China Hong Kong China, Tiawan Singapore Canada United States Vietnam Phillipines Total 5327 1755 671 206 250 75 63 14 8437 From: 1 Nov 20021 To: 11 July 2003, 17:00 GMT+2 348 298 84 32 38 0 5 2 813 Economic Consequences of SARS • Medical Costs • Affected tourism, entertainment, restaurant, and travel industries • Decreased exports • Hong Kong’s growth rate decreased from 7% to 6% • Hong Kong’s financial relief package totals $11.8 billion • Foreign spending in Canada for Jan-March 2003 is down 5.3% The Potential Impact of Bioterrorism • Martin Meltzer’s, CDC economists, model • Crop duster spreads anthrax over a city of 100,000 • If prophylaxis begins immediately: (Assumptions: physicians immediately recognized the problem and ideal treatments were administered) • Human cost • Medical care costs: • Cost including lost productivity: 5000 lives $128 million $3.6 billion • If prophylaxis begins on day 6: • Human cots • Medical care costs 35,000 lives $26.2 billion Factors not included in model • Drug resistant bacteria • Viruses – Most not treatable – They would spread, causing a man made epidemic – Note: Smallpox killed 500 million people during the last century. All the wars combined killed 320 million. Other Potential Cost of a Bioterrorism Attack • All out panic leading to collapse of the stock market • Example – Surat India, 1994 – Natural occurring plague epidemic following an earthquake – 56 deaths an approximately 6,500 cases – Mass fleeing by physicians and citizens, tourist cancelled trips, importers banned all flights/goods/ and citizens from India, and the Bombay Stock Market crashed – Cost $2 Billion Perspective 1) History repeats itself – – This is not the first new infectious disease to suddenly emerge This will not be the last new infectious disease to suddenly emerge 2) “He who does not learn from history is doomed to repeat it.” - The public health infrastructure is essential Infectious Diseases Identified last in 30 years (partial list) • • • • • • • • • • • Rotovirus Parvovirus B19 Cryptosporidium Ebola Legionella Hantaan virus Campylobacter HTLV I and II Staphylococcus toxin E. coli 0157 H7 Lyme • • • • • • • • • • • HIV H. pylori HHV-6 (roseola), HHV-7, HHV-8 Ehrlichia Hepatitis C Guanarito Bartonella Hantavirus Sabia virus BSE Metapneumovirus SARS Other Emerging/ Re-emerging Infectious Disease • West nile • Pertussis • Tuberculosis – Multidrug resistant tuberculosis • Drug resistant bacteria – – – – Pneumococcus Methicillin Resistant Staphylococcus aureus Gram negative bacteria (ESBLs) Vancomycin resistant Enterococcus • Malaria (Drug Resistant Strains) By Improving the Public Health Infrastructure You: • Prepare for man made bioterrorism – Smallpox – Plague – Anthrax • Prepare for nature made bioterrorism / epidemics – SARS – New influenza strains • Prepare for common infectious diseases – Tuberculosis – Meningococcus – AIDS • Improve the health of everyone Lessons Learned from Previous Epidemics (Dave’s top 10 list) 10)Microbes do not need passports to travel , and do not respect borders. – An infectious disease in any part of the world is of concern to the whole world. 9) Epidemics, and rumors of epidemics, have serious economic consequences – Decreased tourism – Animals may need to be sacrificed – This leads to decreased reporting. Lessons Learned from Previous Epidemics (Dave’s top 10 list) 8) People like to place blame for an epidemic – Political consequences 7) Epidemics frequently lead to discrimination against those in whom the disease began. 6) Many people will want to “Do something”, even if that “something” is unproven, and potentially dangerous. 5) Health care workers are at the frontlines of epidemics, and frequently have the highest casualties. Lessons Learned from Previous Epidemics (3) 4) Epidemics frequently start in a remote setting, spread to a large urban area, and then disseminate back to the rural areas as people travel. 3) Infection Control is essential 2)Public Health infrastructure is essential to diagnose and control infectious diseases/ epidemics, but is frequently under funded. 1)Predict the unpredictable. For More Information • World Health Organization http://www.who.int/en/ • Center for Disease Control http://www.cdc.gov • Texas Department of Health http://www.tdh.texas.gov • Public Health Education in Emerging Infectious Disease/ UTHCT – http://192.88.11.221:82/Links.htm • Betrayal of Trust: The Collapse of Global Public Health by Laurie Garrett Thank you Normal Reactions to Vaccinia Immunization • Soreness at vaccination site – Mild – Moderate – Severe 46% 27% 3% • Lymphadenopathy 25.0 - 50.0 % • Myalgia, headache, chills, nausea, fatigue • Fever > 37.7° C 0.3 - 37.0 % 2.0 - 16.0 % Generalized Vaccinia • Occurs 6 to 9 days after vaccination • Usually self limiting • Rates (per million vaccinations) – 241.5 for Primary Vaccinees – 9.0 for revaccinees Autoinoculation • Rates (per million Vaccinations) – 529.2 for primary vaccinees – 42.1 for revaccinees Autoinoculation Vaccinia keratitis • Implantation of virus into diseased or injured conjunctiva and cornea • Initially virus replicates causing ulceration • An antigen-antibody interaction follows leading to corneal cloudiness. • Results in scarring as the lesion heals with significant impairment of vision. • VIG is contraindicated • Topical antiviral agents are the treatment of choice. Erythema multiforme • Many vaccinees develop skin rashes after vaccination, almost all of which are benign. • Either toxic or allergic and require only symptomatic therapy. • Stevens Johnson Syndrome may rarely occur, requiring more aggressive steroid therapy. • Recent studies indicate that 5.614.3 percent of adult vaccinees develop rashes at sites other than the vaccination. Eczema vaccinatum • Dissemination of vaccinia in persons with preexisting eczema or other chronic or exfoliating skin conditions • Lesions cover all or most of the area once or currently afflicted by eczema • Usually mild or self limited, but occasionally severe or fatal • Rates (per million Vaccinations) – 38.5 for primary vaccinees – 3.0 for revaccinees Eczema vaccinatum in contact to recently vaccinated child Progressive vaccinia (vaccinia necrosum) (Patient with chronic granulocytic leukemia) • Vaccinia lesions fail to heal and progresses with associated tissue necrosis • Necrosis can spread to to bones and viscera • Frequently fatal in immunodeficient individuals • Rates (per million Vaccinations) – 1.5 for primary vaccinees – 3.0 for revaccinees Progressive vaccinia (vaccinia necrosum), which was fatal, in a child with an immunodeficiency. Congenital Vaccinia • Infection of the fetus in the last trimester with evidence of disease in the newborn infant. • No proven instance of congenital abnormalities has been attributed to vaccination during any stage of pregnancy. • Some have postulated that vaccination in the first trimester results in some fetal loss but this has not been substantiated. •Frey SE, Couch RB, Tacket CO, et al. Clinical responses to undiluted and diluted smallpox vaccine. N Engl J Med 2002;346(17):1265-74 Postexposure Prophylaxis with Vaccinia (Theoretical) • Immunity to smallpox develops 8 to 11 days after immunization with vaccinia • Incubation period of smallpox is 12 days for naturally occurring disease • Therefore vaccination within 4 days of exposure should confer some immunity and decrease likelihood of death • Most beneficial in those immunized sometime in past Postexposure Prophylaxis with Vaccinia (Clinical Experience) • Italy, 1946 – 21 contacts immunized within 5 days post exposure in whom smallpox developed all had mild disease – 31 contacts who were vaccinated 6 to 10 days after exposure had a case-fatality rate of 19% • India, 1973 – 34 patients vaccinated during the incubation period – 4 of 9 (44%) of those immunized 8 days or more before illness onset died – 10 of 25 (40%) vaccinated 7 or fewer days before illness onset died