PREMATURITY
advertisement

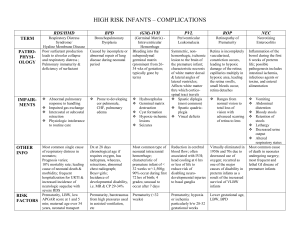
PREMATURITY Sue Omel RN, MS, MPH Nursing Program Supervisor; Washington County DHHS; Public Health Division; Field Team PREMATURITY Why Prematurity is an Important Public Health Issue PREMATURITY Public Health focuses on promoting health and preventing disease Primary Prevention Secondary Prevention Tertiary Prevention PREMATURITY Primary Prevention Decreasing the Rate of Preterm Births Determining the Factors that Impact Preterm Birth Social Biologic Environmental PREMATURITY At Risk Populations Low income women Women of color Women younger than 20 and older than 40 Women who were born preterm Women with a history of previous preterm delivery Women with multiple pregnancy Women with uterine/cervical abnormalities PREMATURITY Other Risk Factors Smoking, use of alcohol, other substance use Infection Stress Trauma Unintended pregnancy Chronic health conditions like diabetes or high blood pressure In-vitro conception History of repeated miscarriages or spontaneous abortions PREMATURITY Despite a good understanding of risks, there has been little reduction in the rate of prematurity in the US PREMATURITY Secondary Prevention Improving the Outcome of Premature Infants PREMATURITY Preterm infants are at higher risk for poor health outcomes than infants born at term PREMATURITY Increased Mortality Preterm birth and low birth weight are the leading cause of death in infants younger than one year. PREMATURITY Infants born before 34 weeks are at greatest risk of death and long term morbidities PREMATURITY Increased Morbidity • • • • • • • • • • • • Respiratory distress and long term respiratory issues; asthma Delayed brain development/developmental delay Cerebral palsy Epilepsy Cognitive delay SIDS/SUIDS Feeding problems NICU admission and re-hospitalization Vision and hearing problems Autism Behavior and learning problems Depression, anxiety, and other mental health issues PREMATURITY Late Preterm Infants Mortality Late preterm infants (34-37) weeks are 6 X more likely to die in the first week of life and 3X more likely to die in the first year Prematurity Late Preterm Infants Morbidity • • • • • • • • Respiratory distress Hypothermia Sepsis Hypoglycemia Inadequate feeding/dehydration Hyperbilirubinemia Growth and developmental issues Immature brain Prematurity The fetal brain at 34 weeks weighs only about 65% of that of a full term infant brain PREMATURITY The Costs of Prematurity • • • • • • Physical/Medical Developmental Emotional Financial Psychosocial Educational PREMATURITY Costs According to the Institute of Medicine The annual costs to society are $26.2 billion dollars $51,600 per infant $49,033 to employer The costs are 11 X greater than those of a normal newborn PREMATURITY The average 1st year costs for a preterm infant are 10X than that of a term infant ($32,325 vs $3,235) The average hospital stay is 9 X longer if the infant is born preterm PREMATURITY What is the Role of the Public Health Nurse? • Improve the health and developmental outcomes of the premature infant by identifying the physical, developmental and social/emotional risks • Implement nursing interventions to reduce the risks PREMATURITY • Reduce costs • Reduce disparities The differences in the rates of disease; incidence, prevalence, morbidity, mortality, or survival rates in one population compared to the health of the general population. The CaCoon Nurse’s Role in Providing Services to Preterm Infants Screening Assessment Education/Information Case Management Care Coordination Support/Advocacy Monitoring PREMATURITY What skills do you need to provide services to premature infants and their families? • Know how to adjust for prematurity • An understanding of the growth and development of the pre-term infant • Understand common medical issues and treatments • Understanding of normal vs abnormal course • Understand infant states, cues, and behaviors • Knowledge of community resources • Ability to provide family centered approach to care PREMATURITY Adjusting for Prematurity Determine gestational age in weeks Subtract the gestational age from 40 weeks Subtract the weeks of prematurity from the chronological age Example: JA was born at 32 weeks gestation. Subtract 40-32= 8 weeks premature Today JA is 12 weeks old chronologically 12 weeks (actual age) -8 weeks = 4 weeks adjusted age Adjustment for prematurity should be done until at least 24 months of age PREMATURITY Growth, Nutrition, Feeding The CaCoon Nurse’s Role in Screening, Assessment and Intervention to Identify Risks and Improve Infant Outcomes PREMATURITY Screening Growth Height, weight, head circumference, and height/weight ratio Development Use standardized tools Other standardized screening PREMATURITY Nursing Systems ASSESSMENT • • • • • Cardiovascular Respiratory Gastrointestinal Urinary Neuro-motor PREMATURITY Risk Assessment • • • • • • • • • • Feeding and Nutrition Infection Unintentional Injury Intentional Injury Exposure to toxins (second hand smoke) Dental Attachment and Bonding Parenting Coping Basic Needs PREMATURITY Case management Helping the family access and utilize other services PREMATURITY Referral and Follow Up • • • • • • • • • • Well Child Care and Immunizations Early Intervention Head Start/Early Head Start Healthy Start WIC Speciality Services ie, OT, PT, Developmental Clinics Community Services to meet basic needs Services for family ie, counseling, primary care, etc Services to provide financial support, ie SSI Respite care PREMATURITY Care Coordination • • • • • • • • • Primary care provider Vision-ophthalmologist Hearing-audiologist/ENT Cardiologist Pulmonologist Gastroenterologist Neurologist Home Health Equipment supplier PREMATURITY Family Support • • • • • Understanding family’s experience and needs Provide opportunity for family to share feelings Identification of support systems Role model and support advocacy efforts Encourage healthy coping strategies PREMATURITY Monitoring Constantly re-evaluating • Repeating screening and assessment • Trying new interventions • Gathering outcome data PREMATURITY Development The Cacoon Nurse’s Role in Screening, Assessment and Intervention to Identify Risks and Improve Infant Outcomes PREMATURITY Screening for Physical Development Standardized screening tools—must look at all areas of development RDSI ASQ CAT/CLAMS Adjust for Prematurity! PREMATURITY Gross motor risks in early screening Looking at more than milestones Use the Infant Motor Screen • Symmetry • Presence or absence of reflexes • Tone • Protective responses • Vestibular responses PREMATURITY Interventions Education/Information Case Management Care Coordination Support Monitoring PREMATURITY Education and Information Current development and what to expect next –normal progression of development Activities to foster development Modifying activities based on infants needs, behaviors, and cues PREMATURITY Case Management Identify and remove barriers Referrals to EI, SSI, OT/PT, Speech, Developmental clinics or pediatricians Community services Infant massage, infant sign language, library programs, swimming classes PREMATURITY Care Coordination Educational staff, medical, neurologist, ophthalmologist, audiologist, developmental disabilities PREMATURITY Support Family’s understanding of developmental issues Family resources and strengths PREMATURITY Social Emotional Development Preterm infants are at significant risk for later relationship issues. These risks are related to: Maternal/family experience Infant’s experience in the NICU Financial impact Infant cues and behaviors Ongoing stress when infant transitions to the home PREMATURITY Maternal Experience Interrupted pregnancy leads to crisis birth Crisis leads to anxiety and fear May also experience feelings of guilt, grief or loss Attachment behaviors are developed in a technical environment that doesn’t foster nurturing Infant is probably less socially responsive and harder to soothe PREMATURITY Maternal outcomes • • • • Depression Disengagement Symptoms similar to PTSD Over-involved and protective PREMATURITY Infant’s Experience Immature brain and nervous system NICU environment Unusual stimulation and pain Cues and behavior patterns may be difficult for caregiver to understand PREMATURITY Infant Outcomes Insecure attachment Anxiety Internalizing problems Difficulty developing social relationships Increased risk for abuse and neglect PREMATURITY The longer the NICU stay, the higher the likelihood of issues related to maternal infant interaction PREMATURITY Interverventions Screening ASQ-SE; screening for maternal depression; screening for attachment issues Assessment Maternal infant interaction; parents knowledge of cues, behaviors, infant state PREMATURITY Education Improve Parent Understanding • Cues • Behaviors • Infant states • Temperament PREMATURITY Variations in behavior, sleep states, and cues should guide all parent interactions. The parent’s role is to meet the infant’s needs. Parents who are empathetic and responsive foster a sense of trust which strengthens the infant’s attachment and sense of security. PREMATURITY Modifying the Environment Help the parent learn to respond sensitively to the infant’s ability to handle various levels of light, noise, and activity and adjust the infant’s environment as needed for the infant PREMATURITY Providing Appropriate Timing Foster positive interactions by helping the parent learn to adjust to the infant’s needs by pacing interactions and avoiding activity that overwhelms the infant PREMATURITY Maintaining and Ensuring Continuity and Predictability Support the parents in their efforts to maintain consistency in the in infant’s routine and daily activities. PREMATURITY Supporting the Infant’s Attempts at Self Regulation Help the parent learn to recognize the infant’s fatigue levels. Assist parent to develop skills that support and facilitates the infant’s ability to calm itself. PREMATURITY Supporting Movement and Positioning and Providing Appropriate Support During All Handling Assist the parent to learn how to provide smooth, gentle, slow handling, how to move in rhythm with the infant, and how to effectively position the infant PREMATURITY Supporting the Infant’s Management of Sleep Wake Cycles Teach normal sleep wake cycles and help the parent develop positive behaviors that facilitate the infant’s level of alertness, smooth state changes, engagement opportunities, and opportunities for selfcalming PREMATURITY Case Management Referral for maternal mental health support Referral to programs that support positive attachment-mother baby group Infant mental heath programs ??? Referrals to services to reduce stressors Financial referrals SSI/DD programs Parenting support programs Respite PREMATURITY Care Coordination Care conferences with other in home programs, services, child care provider to explore ways to foster and support attachment PREMATURITY Support Help family identify support systems Assist family to find other community supportschurch, work, school Empathy for the family’s situation/beliefs Active listening to the parent Activities to support attachment, ie, kangaroo care, infant massage, breastfeeding PREMATURITY Monitoring Repeat screenings and assessments Follow up with referrals Skills building behaviors PREMATURITY Nursing Systems ASSESSMENT • • • • • • Cardiovascular Respiratory Gastrointestinal Elimination Vision and Hearing Neuromuscular PREMATURITY Risk Assessment • • • • • • • • • • Feeding and Nutrition Infection Unintentional Injury Intentional Injury Exposure to toxins (second hand smoke) Dental Attachment and Bonding Parenting Coping Basic Needs PREMATURITY Resources for Interventions Premature Infant Standards Multidisciplinary Guidelines for the Care of the Late Preterm Infant Getting to Know Your Baby Infant Cues and Infant States Coming Home from the NICU Understanding My Signals PREMATURITY Prematurity is a public health issue Public health nurses understand prematurity at both the level of individual and community How do the services provided through the Cacoon program and targeted toward preterm infants integrate with health care transformation efforts in your community? PREMATURITY The Triple Aim of your Local CCO Better Health Better Health Care Lower Costs PREMATURITY When you, as the Cacoon nurse, targets premature infants, how are your services contributing to the Triple Aim. Are you improving the health outcomes of a disparate population? How? Are you improving health care to this population of vulnerable infants? How? Are you lowering costs? How? PREMATURITY How will CaCoon services to premature infants fit into your Early Learning Hub? What are you doing to improve kindergarten readiness? Prematurity References Coming Home from the NICU. A Guide for Supporting Families in Early Infant Care and Development. VandenBerg, K.A.; Hanson, Marci. Paul.H.Brookes Publishing. 2013. Understanding My Signals. Help for Parents of Premature Infants. Hussey-Gardner, Brenda. Vort Corporation. 2013. March of Dimes. www.marchofdimes.com American Academy of Pediatrics: Modified Recommendations for Use of Palivizumab for Prevention of Respiratory Syncytial Virus Infections. Committee on Infectious Diseases. Pediatrics. 2009 Perinatal Origins of First-Grade Academic Failure: Role of Prematurity an Maternal Factors. Pediatrics. 2013 Early Childhood Development of Late Preterm Infants. A Systematic Review. Pediatrics. 2011. PREMATURITY References American Academy of Pediatrics Persistence of Morbidity and Cost Differences Between Late-Preterm and Term Infants During the First Year of Life. Pediatrics. 2009. Safe Transportation of Preterm and Low Birth Weight Infants at Hospital Discharge. Bull, Marilyn J. and Engle, William A. Pediatrics. 2009. “Late Preterm “ Infants. A Population at Risk. Engel, William A., Tomashek, Kay M., and Wallman, Carol. Pediatrics. 2007. Use of Soy Protein-Based Formulas in Infant Feeding. Bhatia, Jatinder, and Greer, Frank. Pediatrics. 2008. PREMATURITY References Getting to Know Your Baby. A Developmental Guide for Community Service Providers and Parents of NICU Graduates. VandenBerg, K.; Browne, J.;Perez, L. 2003. www.wonderbabies.org Multidisciplinary Guidelines for the Care of Late Preterm Infants. National Perinatal Association.2012. www.nationalperinatal.org/lptguidelines.php Infant Cues. Infant States. WIC California Baby Behavior Campaign. California WIC Program. www.cdph.ca.gov/programs/wicworks/Pages/WICCaliforniaBabyBehaviorCampaign.aspx Your Premature Baby. Volume 1, 2, 3. Injoy Videos. www.injoyvideos.com The Effects of Prematurity on Development. Bell, M. www.prematurity.org