General Heme Update Tom DeLoughery, MD FACP FAWM
advertisement

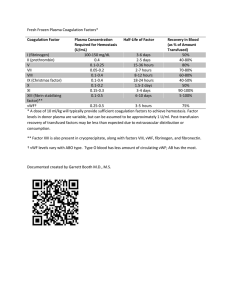
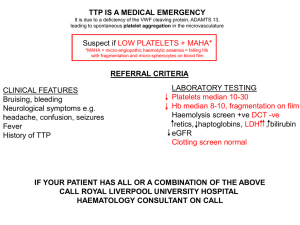
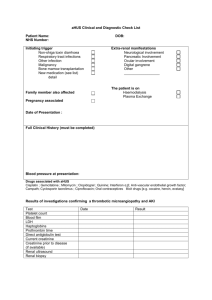
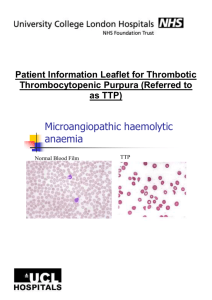
General Heme Update Tom DeLoughery, MD FACP FAWM Oregon Health and Sciences University DISCLOSURE Relevant Financial Relationship(s) Speaker Bureau - None Consultant – Amgen Grants - Alexion Topics • Thrombotic microangiopathies • Bridging therapy • Quick hits Thrombotic Microangiopathy • Key diagnostic features – Microangiopathic hemolytic anemia • Schistocytes • Hemolysis – Thrombocytopenia – End organ damage Classification • TTP – Classic – Relapsing – Chronic • HUS – Typical – Atypical • Other thrombotic microangiopathies – Pregnancy • HELLP syndrome • Post-partum HUS • TTP – Chemotherapy related – Transplant related – Cancer related The Pentad of TTP: Dead, Dead, Dead • Thrombocytopenia • MAHA • Mental status changes: only seen in 40-50% • Renal insufficiency: most often mild – Proteinuria most common • Fevers: 20% Other Abnormalities • • • • LDH elevations (>2-3x nl) Myocardial involvement Pulmonary involvement Gastrointestinal involvement – Pancreatitis Pitfalls in Diagnosis • Classic pentad most often not present • Thrombocytopenia may be mild (20-60,000/ul) • Neurological defects vague • Diagnosis not thought of TTP: Role of Von Willebrand's Factor • VWF synthesized as huge molecules and is cleaved to large molecular • Ability of VWF to bind to platelets varies in proportions to size • Largest VWF can bind spontaneously to platelets • Metaloprotease is responsible for cleaving VWF – ADAMTS13 VWF GPIb GPIb VWF GPIb GPIb GPIb VWF VWF VWF VWF VWF GPIb GPIb GPIb GPIb GPIb VWF ADAMTS13 VWF VWF VWF VWF VWF VWF VWF VWF VWF ADAMTS13 GPIb GPIb GPIb GPIb GPIb ADAMTS13 ADAMTS13 Shiga VWF ADAMTS13 Y ADAMTS13 in TTP • Papers have demonstrated lack of ADAMTS13 activity in TTP patients – IgG inhibitory antibody found in many patients – ADAMTS13 activity increased with exchange • Usually decreased in classic TTP • Usually normal in classic HUS • Mutations seen in hereditary TTP/HUS ADAMTS 13 Levels • Levels may guide therapy • <5% and inhibitor – More severe disease but lesser risk of death – Strong role for immunosuppression esp if relapses • <5% and no inhibitors – Congenital? • 5-50% – Many diseases • Normal – Still can be TTP – May do worse? Therapy • • • • • • Steroids Plasma exchange Immune globulin (??) Vincristine Rituximab Splenectomy Steroids • Seems to play a role in TTP therapy • Usually 60-120 mg prednisone • Slow taper when patients responds • Some patients steroid sensitive Plasma Exchange • Key factor in outcome – 2 RCT • Start with 1.5 plasma volume exchange for at least 5 days • Follow LDH • Taper when LDH normal • Plasma infusion until exchange – 1 unit/4-6 hours Other Therapies • IVIG: not effective • Vincristine: classic drug for resistance disease – 2 mg day 1, 4, 7, 10 • Splenectomy: very controversial Rituximab • Appears to be useful for TTP • No great RCT but abundant anecdotes – Faster remissions – Less relapses • Give after exchange Phase II Study • 40 patients with acute TTP – 34 de novo, 6 relapse • Rituximab within 3 days • Compared to historical controls • Blood 118:1746, 2011 Results • No difference in number of exchanges • No difference in hospital days – Was decreased in non-ICU patients • Marked decrease in relapses – 10% from 57% ADAMTS13 Levels Bottom Line • Rituximab useful in preventing relapses in antibody positive patients • Acute role is undefined – Refractory cases? If ADAMTS ab + Transfusion 50, 2010,: 2753–2760 Problem Patients • Getting worse on therapy – Increase pheresis to 1 vol BID – Vincristine – Rituximab – Splenectomy? – Look for infection Problem Patients • Slow responders – Patience • Slow tapers – Rituximab Relapsing TTP • Relapses common 30-60% – Most ADAMTS13 inhibitors • Can be fatal • Early - inadequate therapy • Late – inhibitor, congenital • Tx: – + Inhibitor – rituximab, splenectomy – No inhibitor • + ADAMTS13 – aHUS • - ADAMTS13 - congenital TTP Oddball Presentations • Severe thrombocytopenia but not much else – Platelets <10,000/ul but with mild hemolysis and neuro symptoms – Most with <5% ADAMTS13 • Thrombosis w/o TTP – 3 cases reported in patients with history of TTP Congenital TTP • Common? • Appears at any age – Pregnancy, etc – Relapsing TTP – Plasma responsive Congenital TTP • Very low ADAMTS 13 but no inhibitor • Can do DNA studies now – Wisconsin blood center Congenital TTP • Management – Plasma infusions 2 units 2-4 weeks – rADAMTS13 • Trial to start soon at OHSU HUS • MAHA, thrombocytopenia and renal failure • Classic (e coli) – Treat uremia • Adults – Plasma exchange may help • Reportable disease!! aHUS • Disease of uncontrolled complement activation leading to renal failure • Difficult to diagnoses • Course in past usual terminated in renal failure/death Complement and Atypical HUS Protein Gene Source Location % of aHUS Factor H CFH Liver circulates ~ 15-30% Factor I CFI Liver circulates ~ 5-10% Membrane Cofactor Protein MCP Widespread Membrane bound ~ 10-15% Factor B CFB Liver, ? circulates <5% C3 Liver, ? circulates ~ 5-10% CFHR1/ CFHR3 Lymphocyte circulates ~ 10% C3 Anti-FH-Ab Unknown ~ 40-50% Jozsi et al. Blood 2008, Frémeaux-Bacchi V et al. Blood 2008, Goicoechea de Jorge 2007, Caprioli, et al Blood 2006, Kavanagh Curr Opin Nephrol Hypertens, 2007 C3 Levels By Mutation Sellier-Leclerc, A.-L. et al. J Am Soc Nephrol 2007;18:2392-2400 Diagnosis • Thrombotic microangiopathy with: – Normal ADAMT13 – Predominant renal involvement – Gradually progressive with therapy • Specific diagnosis – Some with low C3 – Genetic testing - Iowa • http://www.healthcare.uiowa.edu/labs/ morl/index_CDS.htm – Remember many patients will NOT have defects! Eculizumab • Effective in PNH • Known to shut down complement after C5 • Now approved for aHUS Eculizumab in Plasma Resistant aHUS • Greenbaum #193 • Phase II trial 26 weeks – Progressive disease despite plasma – 13/15 patients with increased platelets – 15/17 no need for plasma or plasma exchange – 4/5 patients stopped dialysis Eculizumab in Plasma Resistant aHUS • Extension study • Dosing – 900mg wks 1-4 – 1200mg biweekly Eculizumab in Plasma Resistant aHUS • Patients characteristics – Median age 28 – Time from diagnosis 10 month – Mean plasma tx – 17 – 24% with no complement mutations Eculizumab in Plasma Resistant aHUS • Results – 17/17 patients event free by end of study – 65% with improvement in renal function by one CKD state Eculizumab in Plasma Sensitive aHUS • Licht #3303 • 20 patients “controlled” on plasma therapy • At 60 weeks – Improved GFR – No need for therapy Eculizumab in aHUS • Controlls disease and prevents end organ damage • Need to recognized patients before severe renal disease occurs Work-Up of TM • Pre-treatment – ADAMTS13 levels and inhibitors – C3 and C4 • Consider aHUS – ADAMTS13 normal – Family history of aHUS – Progressive disease Antithrombotics and Surgery • When to stop before surgery • When to bridge Antiplatelet Agents • Aspirin – Stop 5 days before • Clopidogrel, Prasugrel – Stop 5-7 days before • Ticagrelor – 5 days before Ticagrelor Time of Offset of Action http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022433s000lbl.pdf Drug Eluting Stents • Drug eluting stents require long term dual antiplatelet therapy • Increasing reports of fatal MI long after stent placement if antiplatelet agent stopped • Patients should stay on one agent for procedures Cardiac Stents • Bare metal – < 4 weeks: need combined therapy – > 4 weeks: aspirin • Drug eluting stents – < 12 months: need combined therapy – > 12 months: shortest possible duration of stopping clopidogrel The Future? • Cangrelor is intravenous reversal ADP receptor antagonist with short half-life • Recent study using it as bridging • JAMA online first Cangrelor • • • • No increase risk of bleeding Small study but promising May be good option for stents Needs more studies! Approaches to Anticoagulation and Procedures • Continue agents • Stop drug • Bridging therapy Continue Warfarin • Recommended approach for low risk procedures – Dental extractions – Cataracts – Simple endoscopy/colonoscopy – Pacemaker/ICD placement – Hip arthroplasty • Works best if INR < 3.0 Stop all Drugs • Approach associated with least risk of bleeding but (in theory) highest risk of thrombosis • Warfarin and antiplatelet agents must be stopped 5-7 days before procedure • Can take 2-5 days to get INR back up • Best approach for patients not at high risk of thrombosis Bridging • Covering the patient with LMWH while off warfarin • Increasing data – Increases risk of bleeding – No substantial decrease in thrombosis • Shift away from aggressive bridging Mechanical Heart Valve Patients Author n Aortic Mitral Both Clot Bleed Douketis (04) 215 143 46 26 0.9% 0.5% Pengo (09) 190 114 76 ? 1.6% 1.2% Kovacs (04) 112 ? ? ? 4.5% 7.1% Hammerstingl (07) 116 76 31 9 0% 0.9% Mayo (2007) 372 136 48 0.7% 3.6% Total 556 1189 Courtesy Robert D. McBane, M.D 1.2% 2.7% Bridging - Canada • Skieth #546 • Venous thrombosis reviewed – Excluded if • Other indications for bridging • VTE < 90 days • 613 procedures/413 patients Results • 4 DVTs (0.63%) • 1.58% incidence bleeding – 13.6 patients with bleeding and 30% with major bleeding developed DVT • Conservative approach is best Factors Which Increase Risk for Bleeding • Pre-procedure – Trough LMWH level too high • Need to stop q12 LMWH 24 hours before and q24 maybe 36-48% • Too aggressive LMWH in patients with renal disease • Post-procedure – Starting therapeutic LMWH too soon!! • Need 48 hours or more Start LMWH Stop LMWH ~24 hour before Stop Warfarin -5 -4 -3 -2 -1 0 1 2 3 Restart Warfarin Restarting LMWH Simple procedure – after procedure Complex – Prophylactic 24-48 hrs - Therapeutic 48 hrs or more Who We Bridge • Valves – Mitral valve replacement – Multiple valves – Non-bileaflet aortic valve – Bileaflet AVR with other risk factors Who We Bridge • Atrial fibrillation – History of stroke – CHADS2 > 4 – Cardiac thrombus Who We Bridge • Venous Thrombosis – Thrombus within 3 months • One month IVC filter? – Cancer and thrombosis – Virulent thrombophilia ITP • Some new data on TPO agonists • No major trials Eltrombopag and Fibrosis • Brynes #528 • Fibrosis concern with TPO agents • Long term study of eltrombopag with annual bone marrows performed • N = 156 Results • No pattern of increasing reticulin with long use of agent • 2.6% with increase reticulin • Increase reticulin is rare and associated with TPO is uncertain Safety of TPO agonists • May be thrombotic risk with very high platelets counts – Don’t be greedy! >50,000 goal • Reticulin risk is low • In MDS will increase blasts so contraindicated My Current Approach • Dexamethasone 40mg x 4 repeat q14 x 4 – Only dexamethasone exposure – Saves other agents for later • Uncertainties – Some data adding rituximab upfront may increase remission – Not clear if dex is better than standard prednisone – RCT planned Multicenter Study: Response to HighDose Dexamethasone 100 CR: n = 58 Relapse-Free Survival 87% 75 PR/MR: n = 19 65% NR: n = 13 50 25 CR: n = 58 (64%) PR or MR: n =19 (21%) NR: n =13 (14%) P =.05 0 0 5 10 15 20 25 Mos • At 15 mos of follow-up, 5 relapses each among subjects who achieved CR or PR/MR This research was originally published in Blood. Mazzucconi M, et al. Blood. 2007;109:1401-1407. © the American Society of Hematology. nd 2 Line • Splenectomy – Oldest and most effective therapy • Rituximab – 60-70% response – Only 20% “cure” rate • TPO agonist – 90% response – Need for chronic therapy Eltrombopag in Marrow Failure • MPL signaling can influence expansion and growth of stem cells and progenitor cells • Is this clinical relevant? Eltrombopag in Marrow Failure • • • • Olnes #54 Phase II severe aplastic anemia Median age = 45 Dose escalation – 50mg -> 150mg – N = 25 (22 evaluable) Eltrombopag in Marrow Failure • 41% with some response • 32% platelet transfusion independent • 6 with red cell improve – 4 transfusion independent • 5 patients with neutrophil response • Marrows show improvement Eltrombopag in Marrow Failure • Promising results • Needs long term follow-up • Option for severe aplastic anemia? Aspirin for Venous Disease! • Becattini #543 • First idiopathic DVT N = 403 • Randomized after 6-18 months – Most ~ 1 year • Aspirin 100mg daily vs placebo One patient in each group had major bleeding Aspirin • Provocative trial! • Need to replicate and compare to warfarin • An options for patients who refuse/ineligible for warfarin?