Osteoporosis: Definitions, Risk, and Treatment "It's better for people to do the wrong
advertisement

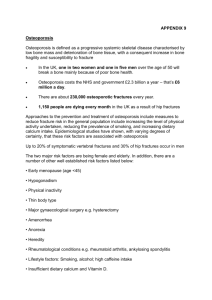
Osteoporosis: Definitions, Risk, and Treatment "It's better for people to do the wrong thing or not optimal thing than to do nothing.” -Dennis Black, statistician, principal investigator for FIT: alendronate trials, defending use of t-scores in defining osteoporosis What is Osteoporosis? “Osteoporosis is a systemic skeletal disorder characterized by decreased bone mass and deterioration of bony microarchitecture.” www.mrc-hnr.cam.ac.uk Primary and Secondary Osteoporosis • Primary • Type 1: Postmenopausal women – Thought to be due to estrogen or testosterone deficiency – Estrogen increasing sensitivity to PTH? • Type 2: Older men and women – Due to decreased vitamin D3? • Secondary – Chronic thyrotoxicosis – Hyperparathyroidism – Malabsorption/Calcium/Vitam in D deficiency – Alcohol/Smoking – Medications • • • • • Glucocorticoids Anticonvulsants Heparin Chemotherapy agents Antacids with aluminum Importance of Osteoporosis • The theoretical concern regarding decreased bone mass is the increased risk of fracture with minimal trauma. • Fractures: 1.5 million “osteoporotic” fractures in US per year. – 700,000 vertebral – 300,000 hip fractures, over 37,000 patients die per year due to complications. • Often associated with high morbidity and mortality with only 1/3 of patients with hip fractures returning to their prior level of functioning,. Prevalence of Osteoporosis • Silent Disease or Normal Aging? • “Osteoporosis is a major public health threat for an estimated 44 million Americans, or 55 percent of the people 50 years of age and older. 10 Million people in the U.S. already have the disease” – National Osteoporosis Foundation • How to create criteria to give the majority of women age 50 and older a disease… Clinical Criteria for Osteoporosis: What is a T score? The Definition • The diagnostic criteria of osteoporosis is based on measurements of bone mineral density (BMD). • A T-score is derived using a frequency distribution curve created with a population of healthy premenopausal young women at peak of bone mass. The t score is the number of standard deviations the patient is from the mean of this “healthy normal” young population. • A T-score of -1 to -2.5 SD = osteopenia • A T-score of less than -2.5 SD = osteoporosis Why use -2.5 standard deviations? • Criteria developed by the World Health Organization and partner, the International Osteoporosis Foundation in 1992 • The committee cited studies indicating that 16% of women in Rochester, MN would experience a hip fracture in their lifetime. They also noted that when pooling several years of BMD data, 16% of postmenopausal women were at -2.5 sd below the mean BMD of a healthy young woman. There was no concrete data to link the 16% at -2.5 SD and the 16% with hip fractures. (We won’t even go into osteopenia) • Incidentally, the IOF’s board is composed of 30+ drug and medical equipment companies. Bone Mineral Density and t-scores and the DEXA scan Using DEXA for t-scores • Not all machines use same standard healthy patient • Variations in calibration depending on manufacturer • More than just bone mineral density can be used to predict future risk of fractures. • BUT the controversy surrounding T-scores and bone mineral density scans could take up several presentations….so onto prevention of fractures. Finding the population at risk of fracture? Does the current osteoporosis criteria really identify those at risk for fracture or should treatment be based on other risk factors? – Other studies have found risks such as family history of fracture, lower weight, greater height, hyperthyroidism history, and inability to rise from a chair were more predictive of future fracture than bone mineral density (Cummings). Goals of Treatment • Because fractures are the main cause of the morbidity and mortality associated with “osteoporosis”, the goal of therapies should be directed towards prevention of a fracture. • Warning: Increases in bone mineral density are not directly correlated with decreases in fractures • Treatments should be assessed and compared based on a decrease in fracture rate. Watch for studies that discusses changes in BMD and do not mention fracture rate. Prevention of Fractures • A balanced diet rich in calcium and vitamin D • Weight-bearing and resistance-training exercises • A healthy lifestyle with no smoking or excessive alcohol intake • Bone density testing and medication when appropriate – National Foundation of Osteoporosis Reporting Relative Risk • Can often make treatment seem more beneficial • Example: A medication decreased the harmful outcome from 1% in the control group to 0.5% in the treatment group. The relative risk reduction is 50% but the absolute risk reduction is only 0.5%. • RRR=relative risk reduction • ARR=absolute risk reduction • NNT=Number needed to treat Comparing treatment options Examined randomized controlled trials comparing 1) Vitamin D and calcium to placebo 2) Alendronate to placebo – Trials involving alendronate were selected due to the large number of trials and apparently most beneficial compared to newer/other bisphosphonates 3) Weight bearing exercise to placebo There were few RCTs on weight bearing exercise and fractures. The benefit of exercise depended on the type of exercise. No RCTs compare exercise to bisphosphonates or other medical treatment in reducing fractures The following slides examine the results of several trials for 1 and 2 above. Calcium and Vitamin D Study Population Outcomes RRR/ARR P-value Chapuy 92 Women in nursing homes with osteoporosis Hip fractures 1.5 yr Nonvertebral fx 1.5 ARR: 2.0% RRR: 25% NNT: 50 ARR: 4% RRR: 24% NNT: 26 .004 Dawson-Hughes 1997 Men and women with osteoporosis > age 65 Nonvertebral fx (3 years) ARR of 7% RRR of 54% NNT: 14 .02 Record 2005 Men and women >70 with low trauma fractures New fracture (2 years) Not significant Porthouse 2005 Age > 70 with 1 risk factor for hip fx Hip fractures (2 years) Not significant: hip fracture rate was very low in this group, even the controls at 1.4% <.001 14 NNT, relatively inexpensiv e Patients had fracture Bisphosphonates • Inhibitors of Bone resorption. May disrupt the mevalonate pathway leading to decreased osteoclast activity but mechanism is not clearly understood. Maybe we can use statins for osteoporosis?? Site of Bisphosphonate action Proteins which increase osteoclastic activity are reduced. Prevention with Alendronate Study Population-all postmenopausal women Outcomes RRR/ARR P-value Liberman 1995, Sponsored by Merck Women with osteoporosis. Separate analysis in pt with previous fracture Vertebral fx RRR: 48% ARR: 3.0% NNT: 33 -NS .03 Low BMD and previous fracture Vertebral fracture RRR: 50% ARR: 7.0% NNT 14 RRR: 49% ARR: 1.1% NNT: 100 <.001 Black, 1996 FIT1 Sponsored by Merck Nonvertebral fx Hip Cummings, 1998 FIT2 Sponsored by Merck Femoral neck t score < -2.1 and no hx of fracture Vertebral (4 yr) Pols 1999 FOSIT Sponsored by Merck Lumbar spine t score < -2.0 Nonvertebral Hip/other (4yr) RRR: 44% ARR: 1.7% NNT: 59 -NS RRR: 45% ARR: 2.0% NNT: 50 Mostly beneficial in patients with previous fracture Large NNT for hip fractures .002 .021 No statistically significant benefit on hip fractures Cochrane Review of 11 trials of alendronate • Once daily dose in primary prevention – RRR 45% ARR 2% NNT 50 for vertebral fractures - No significant difference in primary prevention of hip fractures • Once daily dose in secondary prevention, slightly more effective – RRR 45%, ARR 6%, NNT 16 for vertebral fractures – RRR 53%, ARR 1% NNT 100 for hip fractures Conclusion: Alendronate may be beneficial and cost effective in preventing vertebral fractures in patients who have already experienced an osteoporotic fracture. Their benefit in preventing hip fractures is minimal and limited to patients who have already experienced a fracture. -Cochrane Review And in the media… • Sounds much more effective and promising!! At least these women look older. Most advertisement s show women in their late 40s/early 50s Other Bisphosphonates • Most trials with alendronate. • Similar results (or less effective) have been found in studies of other bisphosphonates and reduction of fractures. • Side effect profiles vary based on type of bisphosphonate. Side Effects • Esophageal Ulceration • GI Perforations, ulcerations and bleeds (depending on type of bisphosphonates) • Musculoskeletal pain • Renal Function disorders • Hypocalcaemia • Some reports of Atrial Fibrillation GENERALIZAITON!!! CAUTION in generalizing the results of studies to larger populations. • Most of the studies of bisphosphonates and fractures were done in: – Older women (mostly over age 65, some over age 80 most benefit) – Women withOUT GI problems – Patients who had already experience a fracture Conclusions on bisphosphonates…. • No benefit on hip fracture in patients whose bone mineral density is close to “normal” • Some benefit in patients in preventing second vertebral fracture if already have a fracture. Could benefit patients on chronic steroids and those with increased risk of falling from another disease (although Vitamin D was similarly effective in these “fallrisk” populations) • Cannot be generalized to patients with GERD, history of ulcers because risks may not outweigh benefits and studies have not been done in this population. • Cannot be generalized to younger patients with osteopenia. Most studies focus on patients over 60, some with patients over 50. General Conclusions The measurement of osteoporosis should be redefined to identify patients at highest risk of future fracture. Decreasing bone mineral density with age is normal. Calcium, vitamin D (in patients who are deficient) and weight-bearing exercise will help prevent fractures (among other benefits) Bisphosphonate research indicates modest reductions in fractures and have mostly been studied in patients who are -older, post menopausal women, many with previous fractures, and without any GI problems. References • • • • • • • • Hamdy, R. et al. Review of Treatment Modalities for Postmenopausal Osteoporosis. Southern Medical Journal. 98(10) Oct 2005. National Osteoporosis Foundation. Disease statistics. Http://www.nof.org/osteoporosis/ Accessed February 15, 2008. Chapuy MC et al. Vitamin D3 and calcium to prevent hip fractures in elderly women. N England Journal of Medicine 1992; 327: 1637-1642. Dawson-Hughes, B. et al. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older N Engl J Med 1997; 10: 670-676 Grant et al. Oral Vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (RECORD) Lancet 2005: 365 1621-1628 Porthouse J, et al. Randomised controlled trial of calcium and supplementation with cholecalciferol for prevention of fractures in primary care. BMJ 2005:; 330: 1003. Susan Kelleher. Disease expands through marriage of marketing and machines. The Seattle Times June 2005. Moynihan, R et al. Selling sickness: the pharmaceutical industry and disease mongering. BMJ 2002; 324: 886-891. References • Black DM et al. Fracture risk reduction with alendronate in women with osteoporosis: Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab 2000; 85: 4118-4124 • Pols et al. Multinational, placebo controlled, randomized trial of the effects of alendronate on bone density and fracture risk in postmenopausal women with low bone mass results of the ROSIT study. Fosamax International Trial Study Group. Osteoporosis International. 1999;9 461-468. • Liberman, UA et al. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study. N ENgl J Med 1995; 333: 14371443 • Black, DM et al Randomized trial of effect of alendronate on risk of fractures in women with existing vertebral fractures. FIT Lancet 12996 348: 1535-1541. • Cummings, SR et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from FIT. JAMA 1998; 280: 2077-2082. References • • • • • • Johnell O, Gullberg B, Kanis JA, Allander E, Elffors L, Dequeker J, Dilsen G, Gennari C, Lopes Vas A, Lyritis G, Mazzuoli G, Miravet L, Passeri M, Cano RP, Rapado A, Ribot C 1995 Risk factors for hip fracture in European Women: The MEDOS Study. J Bone Miner Res 10:18021815. Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM 1995 Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767773. Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM 1995 Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332. Kenny AM, Prestwood KM: Osteoporosis. Pathogenesis, diagnosis, and treatment in older adults. Rheum Dis Clin North Am 2000 Aug; 26(3): 569-91 Bock O, Boerst H, Thomasius FE, Degner C, Stephan-Oelkers M, et al. Common musculoskeletal adverse effects of oral treatment with once weekly alendronate and risedronate in patients with osteoporosis and ways for their prevention. Journal of Musculoskeletal and Neuronal Interactions 2007;7:144-148. Wysowski DK, Chang JT. Alendronate and risedronate: reports of severe bone, joint, and muscle pain. Archives of Internal Medicine 2005;165: 346-347.