Safe and Effective Care Environment: 13-19%

Content of Test Plan structure for NCLEX-PN Exam
Safe and Effective Care Environment: 13-19%
The Practical nurse provides nursing care that contributes to the enhancement of the health care delivery setting and protects clients and health care personnel
Coordinated Care: related content includes but is not limited to the following:
“Advance directives “
Living wills :
1.legal document signed by competent individual indicates treatment /life support measures
2.Indicates who is authorized to make health care decisions for those who cannot
3. Legally binding in most states
Durable Power of Attorney:
1.
Permits a competent adult to appoint someone on their behalf in the event that the adult becomes incompetent
2.
Health care provider must follow this decision
3.
In most states the Durable POA can perform all legal actions needed to fulfill the person’s wishes.
“Advocacy”
Nurse as client advocate should :
1.
Support client’s rights
2.
Defend clients participation in decision making
3.
Safeguard client autonomy
4.
Provide client with information about needs and their options.
“Client care assignments”
“Client Rights”
1.
Privacy includes: Right to make personal choices without interference
Right to have personal info kept confidential & given to only authorized
Personnel
2.
Respectful care
3.
Informed consent requirements:
Must be adult/Voluntary/info given in understandable form/Cannot sign if ddrinking
alcohol or premedicated/ MAY NOT be required in an emergency
Exception to being Adult is:
Married minors/Over age 12 for STD’s, HIV testing, AIDS Rx. Drug & Alcohol RX.
Emanicipated minor & mature minor
Minor seeking outpt. Psychiatric Rx.
Pregnant minor
4.
Confidentiality
5.
Refusal of treatment: self determination act/Advanced directives
6.
Reasonable response to a request for Rx.
7.
Right to know hospital/clinical regulations
8.
Restraints: A. mechanical=May be need for patient safety , must be least restrictive and
documented properly
B. Chemical restraints: Psychotropic drugs CANNOT be used to cintrok behavior
but can be used diagnosis related conditions.
C. Need informed consent unless pt. is unable then you need proxy consent.
D. nursing considerations:
1. assess and document need
2. Consider use of alternative
3. MD’s order is required (cannot order PRN)
4. monitor pt. closely
5. Remove for skin care
9. Legal issues:
Negligence- Unintentional failure to perform an act that a reasonable person would do.
Malpractice-PROFESSIONAL negligence involving misconduct
Required elements:
Duty=legal relationship between nurse and pt.
Breach of duty
Causation=nurse conduct causes injury
Legal issues (con’t)
Invasion of privacy: release of info.
Assault: intentional threat
Battery
False imprisonment: (i.e. restraints/ denied dicharg from hospital)
Laws-Rules of conduct established and enforced by authority
Accountability- reasonable for reasonable care
State Laws: 1.Nurse Practice act-Defines reasonable care in each state ; scope of nsg,=.
Practice.
2. Good Samaritan laws- limits the liability of professionals in emergency
Situations
3.Licensure requirements differs in different states
“Collaboration with interdisciplinary team”
Care team consists of : RN’s, LPN’s, Unlicensed assistive personnel, MD’s, dieticians, PTs/
OTs social workers
Work together as a team and the priority is the PATIENT
“Concepts of management and supervision”
Managed care : goal is to reduce health care costs
Focuses on client outcomes
Emphasizes on costs
Continuous quality improvement:
Involves organized incident reporting
Prevention-focused approach
Change of shift report: Focuses on need of pt./Enables workers to organize care
Types: face to face/taped/
To deliver properly include the following; Pt info( Room # name etc)/Medical plan(i.e.
Diagnosis) /nursing plan(ie special equipment, nursing concerns, referrals etc.)
The reporting nurse describes (Client needs/ How the needs were addressed/info about lab studies, Rxs., Diagnostic tests/Info. Must be pertinent, current
& accurate)
Change of shift report should NOT include: rumors or gossip/Descriptions of routines (i.e. AM or PM care)/Opinons about pts. Lifestyle/Pt. info that does not relate to health condition etc.
For coordinated care to be successful;
1.
Need support from MD’s, Qualified nurse managers/collaborative practice teams/ quality management system
“Confidentiality/information security”
“Continuity of Care”
“Establishing Priorities”
Utilize Maslow’s Hieracrcy of needs
“Ethical practice”
Principles of right and wrong/ ANA Code of Ethics =framework for solving ethical issues
Informed Consent: Requirements (age=adult/married minors/pregnant minor)
Ethical principles of nursing:
1.Autonomy-support of pts. Independence to make decisions and take actions for themselves.
2. Beneficence-duty to help others by doing what is best for them. For refusal of care
(autonomy overrides)
3.Nonmaleficence-“do not harm” Act with empathy toward pt. and staff/it is violated by acts
performed in bad faith
4.Justice-use available resources fairly and reasonably
5.Veracity-communicate truthfully and accurately
6.Confidentiality –safeguard the pts. Privacy
7. Fidelity-Following thru on what the nurse says will be done; carefully attending to the details of the patient.
Ethical reasoning process includes:
1.recognize a moral issue
2.analyze facts and idendify dilemma
3.decide on alternative actions
4.select specific action
5.evaluate the effectiveness of the pt.
“Information technology”
“Legal responsibilities”
Practice within your scope and according to the Laws of the state “Nurse Practice Act”
“Performance Improvement Resource management”
Safety and Infection Control = 11-17%
“Infection and Infection Control”
1.
Data Collection includes: a.
Local (heat, redness, blood, pus etc.) b.
Systematic (fever, weakness) c.
WBC= N.5000-10,000 (elevates with disease or injury) d.
Erythrocye sedimentation rate (ESR) elevations >1-20mm/h indicates inflammation e.
Cultures (Obtain BEFORE starting antibiotic) f.
Highly sensitive C-reactive protein marker of inflammation
2.
Diagnose: a.inflammationn b. disease process c.Hospital acquired (Staphylococcus)
3. Plan/Implement ((Rx. /Reduce transmission(Good handwasing, gloves, masks,
gowns/environmental control/ transmission –based precautions) a.
Airborne precautions: examples (rubeola/TB/Shingles (Herpes Zoster/varicella
(chickenpox)
Private room/ door closed /mask on pt. for transport b.
Droplet precautions: (Strep throat/pneumonia/meningitis caused by H. influenza
Type b mumps)
Happen during coughing sneezing , talking/ requires private room Door
MAY REMAIN OPEN/mask on pt. for transport
C. Contact Precautions; examples((MSR,and Vancomycin resistant organism/herpes
simplex/GI wound/UTIs/clostridium/respiratory virus/pediculosis/scabies)
Needed with pt. activites that require physical skin-to-skin contact
Private room or with pt. with same infection
Gowns (remove before leaving room)
Gloves clean, nonsterile
Diseases: Tuberculosis/Hepatitis A, B, C/Lymes Disease/STD”s (AIDS, Syphilis, Gonorrhea, Genital
Herpes, Chlamydia, Genital warts)
Tuberculosis:
S/S: fatigue, nausea, anorexia, wgt loss/night sweats/irritability/Cough with muco-
purulent sputum SOMETIMES BLOOD-TINGED)/dyspnea/chest tightness
Diagnostic Tests:
Skin testing : (Mantoux test/tine test):
sputum smear
Chest x-ray:
Nursing intervention:
1.
Report to state health dept.
2.
Meds: (INH; rifampin ;Myambutol/Chemotherapy)
3.
Isolation
4.
4. Patient teaching
Hepatitis:
S/S: fatigue/jaundice/anorexia, RUQ pain,and tenderness/malaise/CLAY-COLORED stools/tea-colored urine/pruritus (caused by bile salts under the skin)Elevated Liver enzymes (SGPT) (SGOT)alkaline Phosphatase (ALP)/prolongrd PT/antibodies to specific virus
Nursing interventions:
1.
Frequent rest periods
2.
Contact precautions
3.
Diet low in fat, Hi in calories, carbs, and proteins, NO ALCOHOL
4.
Rx. Pruritis- short nails, calamine lotion antihistamines
5.
Meds: Vitamin K/antiviral drugs: Inteferon and lamivudine
6.
Post-exposure Hepatitis B vaccine
7.
CANNOT DONATE BLOOD
8.
AVOID ALCOHOL and OTC drugs (ASA/ Tylenol/sedatives)
Lyme Disease:
S/S: Rash at the site of the tick bite&concentric lesionwithin2-30 days/regional
lymphadenopathy/flulike symptoms (malaise, fever, H/A, conjunctivtus etc.)
Nursing intervention:
1.
Pt. teaching(cover exposed areas when in wooded area)
2.
Administer Antibiotics (Doxycycline early stages/ later stages IV (Penicillin G)
Sexually Transmitted Disease: (see Handout)
Aids: S/S: HIV Positive in blood/opportunistic infections such as:
1.
Pneumocystis Pneumonia:
S/S: chest tightness, and SOB/persistent dry, nonproductive cough/
rales/dyspnea/tachypnea/lograde to high temp/progressive hypoxemia and
cyanosis
2.
Albicans stomatitis or esophagitis:
S/S: changes in taste sensation/
3.
Neoformans-severe debilitating meningitis: S/S: Fever, H/A, blurred vision, N/V/ stiff
neck/mental status changes/ seizure
4.
Cytomegalovirus: ( CMV) S/S: fever, mailaise, wgt. Loss, Lymnpadenopathy/visual impairment/pneumonia/colitis/encephalitis/adrenalist/hepatitis/disseminated infection
5.
Kaposi’s Sarcoma: S/S: small purpulish brown lesions on any part of the body/diagnosed by biopsy
Diagnostic Tests: Positive HIV on ELISA test/ CBC reveals leucopenia with serious lymphopenia, anemia, thrombocytopenia
AT RISK GROUP;
1. Homosexuals/bisexual men
3.
IV Drug users
4.
Hemophiliacs via contaminated blood
5.
Blood transfusion recipients before 985
6.
Children of infected moms
7.
Heterosexual partners
Transmission: Contaminated blood or body fluids / sharing IV drug needles/sexual contact/transplacental or thru breast milk
Nursing measure:
1. Best is prevention
2.Antiviral meds: (Acyclovir,Zidovudine)
3. Contact precautions
4. Hi protein diet
5. Maintain confidentiality
6. provide support
Poison control:
Data collection:
1.
Airway, breathing, circulation (ABC) FIRST
2.
ID poison
3.
Diagnostic: U/A and serum analysis
Long bone x rays if LEAD
CAT Scan: EEG
Plan/Implement:
1.
Child-proof ing
2.
Initiate steps to stop exposure;
3.
Call Poison control provide info such as : Substance, Child condition, age and wgt.
4.
Poison Control center will advise
5.
Syrup o Ipecac is NO LONGER RECOMMENDED
6.
Save any vomitu,s stool, or urine
7.
Contraindicated to induse VOMIT: a.
When child in danger of aspiration b.
When substance is petroleum distillate(Kerosene, lighter fluid, paint remover) c.
MILK WILL DELAY d.
Don’t attempt to neutralize e.
Only a few antidotes and NO universal antidote
Emergency RX:
1.
Respiratory (intubate if comatose)
2.
Circulation (IV fluid & electrolye balance) cardiac monitoring
3.
Gastric lavage: Large oro/nasal tube inserted and irrigated with NSS until clear
4.
Activated charcoal-Absorbs compounds forming a non-absorable complex a.
Give within 30 minutes of ingestion and after emetic b.
Mix with water to make a syrup: given PO or via gastric tube
How to hasten elimination:
1.
Cathartic to speed substance thru lower GI tract
2.
Diuretics-for substance eliminated by kidney
3.
Chelation-Heavy metals (ie mercury, lead arsenic) metal binds with chelating agent
(deferoxamine, dimercaptrol, calcium EDTA)and forms a complex to be eliminated by kidney
Aspirin Poisoning:
Data collection: S/S/ Tnnnitus, N/V/dizziness/ H/A/ change in mental status/ elevated Temp/hyperventilation (RESP> ALKALOSIS)
Later, Metaboloc acidosia, bleeding, Hypovolemia
Nursing Intervention:
1.
Induce vomiting, initiate gastric lavage with activated charcoal
2.
Monitor VS and Lab values (altered acid-base balance)
3.
Maintain Iv hydration and electrolye balnce
4.
Reduce temp.
5.
Vtamin K (IF BLEEDING)
6.
IV NA bicarbonate enhances excretion
Lead Poisoning:
S/S: irritability, sleepiness, N/V/abdominal pain/Constipation or diarrhea/dec. activity/increased intracranial pressure
Diagnostic Test:
1.
Monitor blood levels
2.
Erythrocyte protoporphyrin level
3.
CBC-anemia
4.
X-Rays Long bone will show “Lead lines”
Plan/implement:
1.
Give Chelating agent =promotes lead excretion in the urine
2.
Maintain hydration
3.
ID source of lead
4.
parents teaching for supervision for PICA
Safety Includes Accident Prevention
1.
Infants until 1 year (car seats, Don’t smoke around infants, don’t leave unattended furniture free of lead base/ be careful with water heaters, small objects , don’t use teething biscuits, child-proof home, safety gates, keep wastebaskets covered, No electrical appliances near water/ pad sharp edges of furniture
2.
1year to 3 years: ( watch toys with small pieces/encourage to sit while eating/turn pot handles toward back of stove/when 20 lbs. car seat could face front back facing car seats before that)
3.
3-6 years: bicycle helmets/make sure bicycle is right size (feet touch the ground when sitting on bike)/look both ways before crossing etc.
4.
6-11years: (obey traffic signs/use protective equipment when playing sports)
5.
Adolescent: (teach appropriate ways to deal with anger/teach hazards of drinking and smoking/seat belts/
6.
Adult: (encourage seat belts/responsible behavior to prevent STDS/ suicide precautions/handgun control and safety/motorcycle helmet use/smoke detectors
7.
Elderly: (Remove throw rugs/make sure floors are nonslip/clear pathways of furniture/use solid chairs with armrest/good lighting/cordless phones/handrails/wear comfortable nonskid shoes/maintain mobility thru exercise ans assistive devices.
Disaster Planning:
Prioritze (TRIAGE) with massive casualities :
Color code:
1.
Red:unstable pts. Require immediate Rx.
2.
Yellow: Stable pts who can wait 30-60 minutes for rx.
3.
Green-Stable pts. Who can wait longer to be trate
4.
Black: unstable pts that have massive injuries that will probably prove fatal
5.
DOA (dead on arrival)
TRIAGE:
1. emergent=immediate threat to life:
2.Urgent=major injuries requiring immediate Rx.
3. Nonurgent=minor injuries that don’t require immediate Rx.
HEALTH Promotion and Maintenance: 7-13%
Includes:
1.
Growth and development
2.
Childbearing-Normal
3.
Childbearing –maternal complications
4.
Childbearing-Neonatal – Normal
5.
Neonatal Complications
6.
Reproduction
7.
Prevention and early detection of diseases
Basic care and Comfort: 9-15%
Mobility:
Assessment:
1.
Body built
2.
Posture
3.
Gait
4.
Joints (flexion, extension, pronation, dorsiflexion, abduction, adduction, hyperextension, rotation, inversion, eversion, supination)
5.
movements:
6.
Skin integrity
7.
Muscle tone
8.
Exercise level
9.
Rest & sleep
10.
Sexual activity
11.
Job-related activity
12.
Developmental mobility
Immobility:
Assess:
1.Gait, muscle tone, joint movement, skin integrity
2. exercise: Passive ROM/active ROM/Isometric
Assistive devices:
1.
Tilt Table: use for wgt bearing on long bones/stimulates circulation to lower circulation
2.
Crutches: measure hgt= 2 fingers below axilla/ support wgt on hand piece NOT ON
AXILLA prevents “CRUTCH PALSY”/crutches kept 8-10 inches out to side/elbows flexed20-
30” angle /stop & rest if diaphoretic or SOB
4-point : RT crutch- Lt. foot; Lt. crutch-RT. crutch
2-pont: RT. Crutch LT> foot advance together : Lt crutch and Rt. Foot advance
Together
3-point: Advance weaker leg and both crutches simultaneously; then advance good
Leg
Swing-to-swing through: Advance both crutches followed by both legs
3.
Walker: Elbows flexed at 20 degree angle/ lift and move walker forward 8-10 inches/with partial or non-wgt-bearing put wgt on wrists and arms and step forward with affected legs/Nurse should be behind pt. hold onto gait belt at wrist.
4.
Cane: Straight cane/ Quad cane
5.
Lift: Hoyer
6.
Sliding Board:
7.
Adaptive devices: (ei extended shoe horn)
Herniated Intervertebral DisK
S/S: Low back pain/Lack of muscle tone/poor posture or body mechanics/sensory changes
Diagnosis: Ct scan, MRI, myelography, diskogram
Surgical: Laminectomy/ Laminectomy with fusion/
Plan/ Implement; preop teaching/ postop teaching/ pt. teaching
Developmental dysplagia of the Hip:
S/S: Uneven gluetal folds and thigh crease/limited abduction of the I with pain/
****Positive ORTOLANI’s Sign – clicking sound heard when when affected hip is abducted/ shortened limb on affected side/delays in iwalking/ limp,lordosis, waddling gait WHEN OLDER
Predisposition:
1.
Intrauterine position
2.
Gender (F)
3.
Hormonal imbalance (estrogrn
4.
Cultural influence (Some culture carry child straddled against hip)
Diagnostic: X-rays
RX:
1.
Reduce by manipulation
2.
Splinted with proximal femur centered in the acetabulum
3.
Pavlik harness-worn full time for 3-6 monthsuntil hip is stable
Scoliosis: Lateral curvature of the spine
S/S: Poor posture/uneven hips and shoulders/kyphosis (lump on back)/ uneven waistline
2 types:
1.
Functional-flexible deviation that corrects by bending
2.
Structural- permanent, hereditary deviation
Functional RX: sit-ups/ pelvic tilt/ push-ups with pelvic tilt
Structural RX:
1.
Spinal fusion with Harrington Rod insertion
2.
thoracolumbosacral orthotic brace (effective for 30-40 degree curves) a.
wear 23 hrs./day b.
wear protective undershirt c.
skin care to pressure areas d.
isometric exercises
Club Foot (Talipes Equinovarus)
S/S: Plantar flexion or dorsiflexion/inversion/adduction of forepart of foot
Diagnostic :
Rigid abnormality of talus bone @ birth/ DOES NOT involve muscles, nerves, blood vessels
RX: 1. Foot exercices- Manipulation of foot q4hrs. to correct position
2Casts and splint application
Joint Disorders:
3.
Denis-Browne- horizontal abduction bar
1.
Osteoarthritis: DJD Trauma to joint due to repetitive use NONSYSTEMATIC
Risk factors: increased age, obesity, trauma to joints due to repetitive use
S/S: Joint pain & swelling and limitation of movement / joint stiffness/ contracture
Herberden ‘s Nodes of fingers and Bouchard’s nodes of hands
Diagnostic: X-rays of joints show narrowing of joint space
RX: Pain management/wgt. Control/ NSAIDS
2.
Rheumatoid Arthritis/ SYSTEMIC
S/S: Joint pain & swelling and limitation of movement / joint stiffness/ contracture deformities/Nodules/Ulnar deviation/Hi fever and rheumatoid rash
Diagnostic: Rheumatoid factor may be negative/ C-reactive Protein/ESR/ANA
X-Rays/ Aspiration of synovial fluid
RX: Pain management/ wgt reduction/rest, activity, exercise/ Heat/splints for joints/Analgesics such as NSAIDS/antirheumatic drugs/Immunosuppressive drugs/antitumor
Necrosis drugs
3.
Gout:NONSYSTEMIC
S/S: joint pain, swelling, limitation of movement, contracture deformities
Diagnostic: X-rays
Blood test: WBC/ESR/Uric Acid Level/synovial aspiration
RX: Pain Management (ASA)
Avoid meats rich in PURINES (organ meats, sardines, fish)
Meds for gout: Benemid/Allopurinol
Paget’s Disease:
S/S: pain/ bowed legs/eenlarged skull/kyphosis/ pathological fractures
Diagnostic: Unknown Etiology/ occurs in OLDER adults
RX: analgesics/enc. Rest/safety precauctions because of pathological fractures/Meds include:
Calcitonian/Fosamx/Aredia
Bursitis:
S/S: pain due to inflammation/ dec. mobility especially on abduction
RX: Rest/immobilize effected joint/pain meds/muscle relaxants/steroids( Cortisone injections intrarticular/ apply heat/cold/promote ROM /
Osteoporosis:
S/S: decreased hgt./lo back pain/kyphosis
Diagnosis: Decrease bone mass determined by bone density test
Risk factors:
POSTMENopausal/ age 60 or >/immobility/HX. Of smoking/small framed lean body/hi alcohol intake/prolonged use of steroids
RX: Diet hi in Calcium, Protein, Vit. D
Encourage walking/ROM exercises/ Meds include: Calcitonian, replacement therapy (Estrogen)
Osteomyletis: Infection of the bone caused by Staph
S/S: pain/ swelling/redness/fever/leukocytosis/elevated sedimentation rate/Positive C/S
Risk Factors:
Poorly nourished/elderly/obesity/impaired immune system/long tern corticosteroid therapy
RX: Meds. Analgesics,/antibiotics/antipyretics
AVOID HEAT APPLICATIONS /asepsis with wound care/Hi protein diet/ support extremity
Osteomalacia: decalcification of bone due to inadequate intake of Vitamin D
S/S: Bone pain & tenderness/bowed legs/kyphosis/muscle weakness
Diagnosis: X-ray
RX: Pain management / increase exposure to SUNLIGHT/VITAMIN D/ CALCIUM
Spina Bifida (Neural Tube defect) Cogential anomoly
S/S: bulging/saclike lesion filled with spinal fluid/hydrocephalus risk increased/paralysis of lower extremities/neurogenic bladder& bowel, prolapsed rectum
RX: occulta (NO Rx)/ observe for leakage of CSF/ maintain asepsis/position on abdomen or semiprone with pillows/Observe for inc. intracranial pressure
Hydrocephalus:
S/S: Increase in fronto-occipital circumference/sunset eyes/nystagmus/split suture/widened fontanelles/hi-pitched cry/prominent forehead, dilated scalp veins/
Diagnostic: Increased in CSF
Causes: Neoplasm/spina bifida/comgenital cysts
RX: Ventriculoperitoneal shunt/ Ventricular atrial shunt/ventricular drainage
Contusions:
injury of soft tissue RX: COLD 1 st . 24 hrs followed by HEAT (Ace Bandage)
Strain:
MUSCLE pull and or/TENDON pull or Tear
RX: REST & ELEVATION intermittent Ice for 24 hrs. followed by HEAT (ace pressure bandage)
Sprain:
Torn and stretched LIGAMENT RX:
RX: REST & ELEVATION intermittent Ice for 24 hrs. followed by HEAT (ace pressure bandage)
Dislocation:
Displacement of joint bones so their articulating surfaces lose contact.
RX: ORTHOPEDIC Emergency : immobilization & reduction. The dislocated bone is brought back to
its normal position. (bandages and spints to immobilize part
Fracture:
break in continuity
of the bone
S/S: Swelling/pain/lossof sensation/deformity/muscle spasms/loss of function/crepitus (Grating sound on movement of ends of broken bones)decreased or absent pulses distal to injury/affected extremity COLD.
Complications of fractures:
1.
Fat embolism
2.
Hemmorrage
3.
Delayed union
4.
Malunion
5.
Sepsis
6.
Compartment syndrome
7.
Peripheral nerve damage
RX of fractures:
Splinting/internal fixation (metal, screws, pins)/open reduction (ORIF) surgical dissection to reduce fracture/Closed reduction manual manipulation with traction/Cast application
TYPES of traction:
Purpose: reduce fracture/eliminate pain/prevent deform./promote healing
1.
Skin- (Buck’s extension/ Russell’s, pelvic traction) pulling force applied to SKIN
2.
Skeletal: (Halo, Crutchfield Tongs) Pulling force applied to BONE
Care:
1.
Straight Alignment
2.
Wgts. Hang freely
3.
Inspect skin for breakdown
4.
Maintain position for countertraction
5.
Enc. Movement of UnAFFECTED part
6.
Maintain continuous pull
7.
Clean pins (hydrogen peroxide ½ strength or NSS and sterile swabs
CAST APPLICATION:
Provides immobility of the affected part
Immediate care of cast:
1.avoid covering until DRY 48 HOURS
2.Avoid resting cast on hard surfaces
3.Keep affected limb elevated above the level of the heart
4.DANGER SIGNS: blueness or pallor/pain/numbness/tingling sensations/
IF PERSISTS CALL MD
Complications: Impaired circulation/peripheral nerve damage/pressure necrosis
Fractured Hip: Commonly seen in elderly
S/S:
1.
Leg shortened , ADDUCTED, EXTERNALLY rotated
2.
Pain
3.
Hematoma
RX: Total Hip replacement or ORIF (Repair with screws, pins etc.)
Total Hip Replacement:
Postop:
1.
ABDUCTION with pillow and later soft pillows between legs while OOB
2.
Good alignment important
3.
DON’t turn on affected side
4.
Don’t flex hip more than 45-60 degrees
5.
PREVENT THROMBOEMBOLISM: patients on Lovenox or Coumadin to prevent
6.
Chair with arms while OOB (STRAIGHT BACKED not soft sofa type)
7.
Initially ambulated by PT
Complications:
1.
Dislocation of prosthesis
2.
Excessive wound drainage
3.
Throboembolism
4.
Infection
Amputation:
AKA= above the knee/ BKA+ below the knee
Nursing intervention:
1.
Delay prosthesis fitting: Cover limb with elastic bandage to shrink (Penrose drain in place)
2.
Immediate prosthesis: Cover limb with dsg. And rigid plastic dressing for pressure to
prevent bleeding (NO Penrose in place)
3.
Phantom pain: experienced immediately and up to 3 mons. Postop
Occurs more frequently with AKA Feelings of crushing/cramping/twisting pain
RX: Beta Blockers: for dull, burning sensation
Anticonvulsants: for stabbing & cramping sensation
Antispasmodic: for muscle spasms or cramping
Neuromuscular Disorders:
Parkinson’s: DEFICIENCY OF DOPAMINE IN THE BRAIN
S/S: Tremors(pill-rolling motion) akinesia(Loss of automation) rididity, weakness, “Motorized propulsive gait, slurred monotonous speech, dysphagia, salivation, maskline symptoms, drooling, constipation, depression, dementia
RX: MEDS: Sinemet, pramipexole, benztropine, amantadine
Myasthenia Gravis: DEFICIENCY of acetycholine at myoneural junction
S/S: muscular weakness, Diplopia, PTOSIS, impaired speech, Dysphagia, resp. Distress/Periods of remission and exacerbation
MEDS: Anticholinesterase/Corticosteroids/Immunosuppressants/ prostigman /TENSILON
Multiple Sclerosis: Demyelination of white matter in the brain & spinal cord
S/S: Early: Vision and motor sensation changes LATER: Cognitive and bowel changes, muscular incoordination, ataxia, spasticity, intention tremors, nystagmus, chewing & swallowing difficulties, impaired speech,Incontinence emotional instability, sexual dysfunction
Meds: Immunosuppressants/corticosteroids, antispasmodics,
Amylotropic Lateral Sclerosis: (ALS) (Lou Gehrig’s Disease): progressive degeneration involving the
lower motor neurons of the spinal cord and cerebral cortex.
S/S: Tongue fatigue/ atrophy with fasciculations (Brief muscle twitching)/ nasal quality to speech,
Dysarthia/dysphagia, aspiration, Progressive muscular wasting , atrophy, spasticity, weakness, cognitive dysfunction/ Resp. insufficiency (usually cause of death)
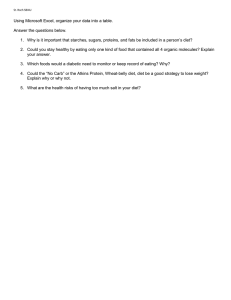
Physiological Integrity: Nutrition
Caloric intake: average adult need 1000-3000 calories /day
Fluid intake= 1800-2500cc/day
Nutrient requirement;
1.
Carbohydrates= 1 st . source of energy
2.
Fats=2 nd source of energy used by the body (waste products =ketones)
3.
Proteins: last source of energy (depletion of protein leads to muscle wasting)
4.
Vitamins-= organic substances found in foods a.
Fat soluble= A-D-E-K b.
Water soluble: Thiamine B1, Riboflavin B2,Niacin, PyridoxineB6, Folic Acid,
CyanocobalaminB12, Ascorbic Acid
5.
Minerals: Calcium, Phosphorous, Fluoride, Iodine, NA. K, Iron
6.
Food Pyramid: Grains: (6-7 oz)
Veggies (2 1/2 – 3 cups)
Fruits 1 ½ -2 cups)
Oils (5-6 tsps)
Milk (3 Cups)
Meat and beans (5-6 oz.)
General Diet: Eat a variety of foods:
Grains: Bread cereal, pasta, popcorn, rice, tortillas (Know recommended daily requirements)
Veggies: Dark green includes: ( broccoli, spinach, greens, leafy veggies)
Orange Veggies: (carrots pumpkin, sweet potatoes)
Dried beans and peas (split peas, pinto , kidney, black, soy (tofu),
Starchy veggies: (Corn peas white potatoes
Oils: (nuts,, butter, margarine, cooking, oils, salad dressings)
Milk: (Milk yogurt, cheese, puddings)
Meat and beans; ( Meat, poultry, dry beans, eggs, peanut butter, nuts, seeds)
Diets: Types (VEGETARIAN DIETS)
Analysis: Due to Religion (7 th Day Adventists) / Health reasons/ economic reasons
At Risk for: deficiency of vitamin B12 associated with megoblastic Anemia
Toxic levels of Vitamin A: causing Anorexia, irritability, dry skin and hair loss
1.
Vegan Diet; fruits, veggies, nuts, beans, and seeds (ixclude: all sources of animal protein, fortified foods, and nutritional supplements
2.
Lactovegetarian diet: All foods on vegan diet but also includes: milk, cheese, yogurt, other milk products as the only sources of animal protein.
3.
Ovovegetarian Diet includes all foods on a vegan diet, along with EGGS, as the only source of animal protein
4.
Lactovegetarian Diet: includes all foods on a vegan diet, along with milk, cheese, yogurt, other milk products and eggs as only source of animal protein.
5.
“Red-meat abstainers” consider themselves vegetarians and eat animal products with the exception of red meat
Common Therapeutic Diets: (see handout)
1.
Clear Liquid : (Gelatin, popsicle, tea with lemon,, gingerale, bouillon, fruit juice, without
pulp)
Common: Postop, acute vomiting/diarrhea)
2.
Full Liquid: ( Milkshakes, soups, custard, All clear liquid)
Common: GI Upset (Diet progression after surgery)
3.
Lo-Fat, Cholesterol Restriction: ( Fruit, veggies, cereals, lean meat )
Common: Atherosclerosis, Cystic Fibrosis
4.
NA restricted: (cold baked chicken, lettuce with sliced tomatoes
Common: Heart failure, hypertension, cirrhosis
5.
Hi Roughage, Hi fiber: (Cracked wheat bread, minestrone soup,
Common: constipation, large bowel disorders
6.
Low residue(Roast Lamb, buttered rice, sponge cake, “white processed foods”)
Common: Temporary GI/elimination problems (lower bowel surgery)
7.
Hi Protein (30 grams powdered skim milk and 1 egg in 100 cc water , Roast beef sandwich and skim milk)
Common: Burns, infection, hyperthroidism
8.
Renal Diet Unsalted veggies, white rice, canned fruits, sweets
Common: Chronic renal fairure
9.
Low Phenylalanine Diet: fats, fruits, jams, low-phenylaline milk
Common: phenylketonuria (PKU)
Cultural food Patterns:
Orthodox Jewish: Laws:
1. Milk/milk products never eaten at same meal as meat (Milk may not be
taken until 6 hrs. after eating meat)
2.2meals dairy products 1 meal meat
3. Separate utensils used for meat and milk dishes
Meat must be kosher (Drained of blood
Prohibited: Pork/ diseased animals or animals that die a natural death/ birds of prey/Fish without
fins or scales (shellfish, oysters, crab, lobster)
Muslim: Dietary laws on muslim teaching in KORAN
1.
Fermented fruits/veggies PHOHIBITED
2.
PORK PROHIBITED
3.
Alcohol Prohibited
4.
Foods with special value: Figs, Olives, dates, honey, milk, buttermilk
5.
Meat must be Halal (drained of blood)
6.
30 day period of daylight fasting required during Ramadan
Hispanic:
Basic foods: dried beans, chili peppers, corn
Use small amounts of meat and eggs
Puerto Rican:
Main type of food is viandos-Starch veggies and fruits (Plantain & green bananas)
Diet includes: lg. amounts of rice and beans
Coffee main beverage
Native American:
Food has religious and social significance
Diet includes: meat, breads, (tortillas, blue corn bread) eggs, veggies(corn, potatoes, green beans, tomatoes) fruit
Fryng is common method of food preparation
African Americans:
Minimal use of milk in diets
Frequent use of leafy greens
Pork commin in diet
French American:
Foods strong flavored & spicy
Frequently contains seafood
Food preparation begins with a roux made from heated oil and flour, veggies and seafood dded.
Chinese:
Uses freshest food available cooked in a wok using a small amt. of fat & liquid
Meat used in small amts.
Eggs & soy products used for protein
Japanese;
Rice is basic food
Soy sauce used for seasoning
Tea is main beverage
Seafood frequently used (Raw fish-sushi)
Southeast Asian:
Rice is basic food eaten in separate rice bowls
Soups frequently used
Fresh fruits & veggies frequently part of diet
Stir fry in wok common
Italian:
Bread & pasta are basic foods
Cheese frequently used in cooking
Food seasoned with spices, wine, garlic, herbs and olive oil
Greek:
Bread is served with q meal
Cheese (feta) frequently used for cooking
Lamb and fish frequently used
Eggs used in main dish, but not breakfast food
Fruit used for dessert
Diet premature Infants:
Nutrition requirements:
100-200 Cal/k/day
Higher NA, Calcim, An Protein Requirements than full term infant
Parenteral Nutrition/ gavage feedings/ soft (premie) nipples
Diet full term Infants:
Breast feeding:
Human Milk is ideal food; RECOMMENED FOR 1 st . 6-12 Months
Colostrum is secreted at first
1.
Clear and colorless
2.
Contains protective antibodies
3.
High in protein and minerals
Milk is secreted after day 2 to 4
Milky white appearance
Contains MORE fat and lactose than colostrum
Formula feedings is alternative to breast feeding
Intro to solid foods:
1-4 months Liquid vitamins only A-D_C fluoride
4-5 months: cereal Usually RICE 1 st ., strained fruit
5-6 months: Strained veggies; strained meat
7-9 months: chopped meat; hard breads and “finger foods” , potato baked, mashed
Toddlers:
Needs fewer calories in diet but more protein and calcium than infants
Preschool age:
Protein and calcium needs remain high
Adolescent :
Caloric, calcium, and protein needs are high
Females experience loss of iron through menstruation
Mineral and vitamin needs are high
Hi calorie, Hi protein, Hi- iron intake, Hi minerals and vitamins
Adult and elderly:
Balanced diet is important
Calorie LIMITATIOn with DECREASEd activity levels
Declined ability to chew and changing taste buds can cause impaired nutrition in elderly
Need same level of vitamins and minerals
Nutrition during pregnancy:
Protein: (meat, 1 egg, cheese) Pregnancy 3 servings Lactation: 4 servings
Veggies: (Yellow or green) 5 5-6
Bread and cereal :whole grain or enriched 5 5
Milk products(cheese, ice cream, cottage 4 Cups 5 Cups
Cheese)
Calories over maintenance: Plus 300 plus 500
Folic acid: 400 mcg 280 mcg
Enteral Nutrition:
Alternative feeding
Liquid food delivered to the stomach, Distal duodenum Via NG tube, PEG tube or PEJ tube
Conditions that warrant enteral feedings: Preoperative: GI Problems: S/E of oncology therapy
(CHemotheraphy)Alcoholism, chronic depression, eating disorders, head & neck disorders or surgery.
TPN: Method of supplying nutrients by IV route
Contains; Amino acids-dextrose formula 10%-50% fat emulsions;
Nursing intervention: Monitor blood glucose levels for (hyperglycemia) and monitor blood for
serum osmolality
Methods of administration:
Peripheral: should not use > 10% dextrose (Used for < 2 wks)
Central: PICC Line: dextrose solution > 10% usually < 4 weeks administration
Triple Lumen central catheter administration:
Single Lumen central catheter
Atrial: Rt. Atrial (Hickman/ Broviac)
Subcutaneous port: Huber needle needed
Plan for TPN:
1.
initial rate 50cc/hr and gradually increase to 100-125cc/hr.
2.
Infuse solution by PUMP ADMINISTRATION
3.
Infusion Rate:
Increased rate results in hyperosmolar state( headache/nausea/fever/chills and malaise)
Slowed rate results in “REBOUND” hypoglycemia caused by delayed pancreatic reaction to change in insulin requirements, DO NOT DISCONTINUE SUDDENLY
Complications of TPN include:
1.
Infection/sepsis
2.
Pneumothorax because of line placement
3.
Hyperglycemia/ hyperosmolar coma
4.
Hypoglycemia: If 10% solution is discontinued suddenly
5.
Fluid Overload: “DON’t PLAY “Catch-up” may cause
6.
Air embolism: Monitor for respiratory distress