On the CUSP: STOP BSI Identifying Barriers to Evidence-based Guideline Compliance © 2009
advertisement

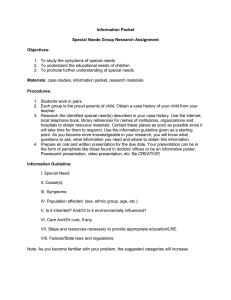
On the CUSP: STOP BSI Identifying Barriers to Evidence-based Guideline Compliance © 2009 Learning Objectives • To learn about the different types of barriers to guideline compliance • To learn how to identify the barriers to guideline compliance • To understand how to develop a process to eliminate or reduce the effects of these barriers © 2009 Evidence-based Behaviors to Prevent CLABSI • Remove unnecessary lines • Wash hands prior to procedure • Use maximal barrier precautions • Clean skin with chlorhexidine • Avoid femoral lines © 2009 Ask Front-line Staff • What are some of the leading problems and barriers encountered in your unit that may hinder compliance with this guideline? • Does the front-line staff know what is expected from them regarding guideline compliance? Do they agree with the guideline? • What are some of the strategies and tools you have implemented to improve compliance with this guideline in your unit? © 2009 Specific Items • Who are the care providers responsible for ensuring compliance with this guideline? Can you describe their roles with regards to complying with this guideline? • What information do you need to be able to follow this guideline? • How do you find out the date that a central venous catheter was inserted to a patient? • What are your practices to reduce central venous catheterrelated bloodstream infections? What are the common lapses in compliance? © 2009 Observe • Shadow a care provider while following a guideline (multiple times, multiple providers) − Include different lenses – nurse, infection control, human factors/ QI expert shadowing physician − Focus on system characteristics rather than the individual physician © 2009 Try out the Guideline • Triability of a guideline increase guideline compliance • Usability testing of a technology (guideline) – Walkthrough: Walk the process of inserting and maintaining a central line – Scenario-based testing – How easy is it to comply with the guideline? © 2009 Types of Barriers (4As) • Awareness → Implement education • Agreement → Group discussion • Ambiguity → Clarify any type of ambiguity • Ability → Identify any impeding system factors and eliminate them or reduce their impact © 2009 Beliefs of a Clinician • Behavioral beliefs: Does complying with a guideline lead to positive outcome(s)? • Normative beliefs: What are the expectations of my colleagues regarding complying with a particular guideline? • Control beliefs: What are the factors that may impede or facilitate guideline compliance and how much I can control these? © 2009 Ambiguities • Task ambiguity • Expectation ambiguity • Responsibility ambiguity • Method ambiguity • Exception ambiguity © 2009 Examples to Barriers • Unclear feedback (expectation ambiguity): Presenting bloodstream infection rates in the format of 4.6 per 1000 line days is not perceived by nurses as directly relevant to their practice • Forgetting to review line necessity daily due to inadequate reminder mechanism • High workload negatively affecting hand washing compliance • Central line cart is not stocked regularly © 2009 Identifying Barriers • Conduct preliminary interviews to understand causes of noncompliance. Is guideline compliance intentional or nonintentional? − Non-intentional: Interview care provider − Intentional: Conduct observations and interviews • Include different types of care providers in the process of identifying barriers (physicians, nurses, respiratory therapists, infection control, human factors expert) © 2009 Reporting Findings Reporting framework – Provider: job category, skills, beliefs – Tasks: Ambiguities (role, task, exception), guideline – Environment – Tools – Organization Interdisciplinary meeting – Discuss findings – Prioritize barriers and develop action plans © 2009 Action Plan • Form an interdisciplinary group of people (physician, nurse, inf control, resp therapy, human factors/QI expert, other) responsible with identifying barriers • Each one conducts at least one observation and one interview. • One clinician and one non-clinician walks through the process together. • Summarize findings using the barrier reporting framework • Discuss findings in an interdisciplinary meeting (including unit administrators) and prioritize the barriers to tackle. • Identify action plans and assign responsibilities • Review the progress periodically © 2009 References • Azjen (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179-211. • Carayon et al. (2006) Works system design for patient safety: the SEIPS model. QSHC 15: i50 - i58. • Gurses et al. (2008) Systems ambiguity and guideline compliance, QSHC 17:351-359 • Pronovost et al. (2008). Translating evidence into practice: a model for large scale knowledge translation. BMJ 337:a1714 • Reason (1990) Human Error. Cambridge University Press, Cambridge. • Rogers, E. M. (1995). Lessons for guidelines from the diffusion of innovations. Jt.Comm J.Qual.Improv. 21, 324-328. • Thompson (2008) View the world through a different lens: shadowing another Jt.Comm J.Qual.Improv . 34, 614-618(5). © 2009