JOHNS HOPKINS
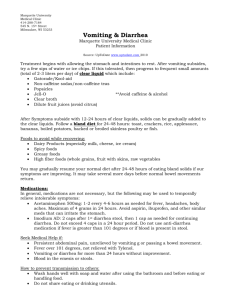
advertisement

JOHNS HOPKINS U N I V E R S I T Y Department of Pathology 600 N. Wolfe Street / Baltimore MD 21287-7093 (410) 955-5077 / FAX (410) 614-8087 Division of Medical Microbiology THE JOHNS HOPKINS MICROBIOLOGY NEWSLETTER Vol. 26, No. 14 Tuesday, August 28, 2007 A. Provided by Emily Luckman, Division of Outbreak Investigation, Maryland Department of Health and Mental Hygiene. There is no information available at this time. B. The Johns Hopkins Hospital, Department of Pathology, Information provided by, Aatur Singhi, M.D., Ph. D. Case presentation: The patient is a 38 year old HIV-positive male (diagnosed 3 years ago) presenting with watery diarrhea for 6 to 7 days. He had no fevers, but had slight nausea and one episode of vomiting. He denies blood in the stool and the diarrhea did not respond to Imodium. During this time, he lost approximately 10 pounds. The patient’s vital signs were T 96.7F, BP 115/70, HR 79 and his weight was 211 pounds. Rectal exam revealed no internal or external lesions. The stool was noted have a green appearance. A stool examination revealed Microsporidium organisms when tested using the calcofluor white and modified trichrome stains. Enterocytozoon bieneusi and Encephalitozoon intestinalis Epidemiology: Microsporidia is a generic designation for obligately intracellular, spore-forming protozoan parasites belonging to the phylum Microspora and the order Microsporida. They are eukaryotes containing 70S ribosomes but lacking mitochondria, peroxisomes, Golgi membranes, and other eukaryotic organelles. The phylum Microspora contains over 1,200 species belonging to 143 genera that have been described as parasites of both vertebrate and invertebrate hosts. 14 species have been identified as opportunistic human pathogens worldwide, two of which are Enterocytozoon bieneusi and Encephalitozoon intestinalis. In the United States, microsporidiosis is reported mostly in immunosuppressed adults, especially with HIV. E. bieneusi infection of small intestine enterocytes is detected in 15-34% of AIDS patients who lack other identified causes for chronic diarrhea. Most cases in HIV patients are reported with severe immunocompromise (CD4 <100), and morbidity can be significant. E. bieneusi infections often result in protracted debilitating diarrheal illness which can last months. Mortality with E. bieneusi is as high as 56%. In addition to chronic diarrhea, malabsorption and wasting occur in patients with AIDS and microsporidiosis. E. bieneusi causes > 90% of intestinal microsporidiosis in this population; E. intestinalis causes the remainder. Increasingly cases of microspoidiosis are reported in immunocompetent patients. E. bieneusi and E. intestinalis infections are increasing among HIV negative travelers and residents of tropical countries. Laboratory identification: There are several laboratory methods for diagnosis. Transmission electron microscopy is considered the gold standard and allows species identification based on ultrastructural morphology, but is costly and time consuming. Microscopic examination of body fluid samples allows the most rapid diagnosis of Microsporidial infection, but does not allow identification to the species level. The modified trichrome stain (Chromotrope 2R) is commonly used to detect Microsporidia in urine, stool, or mucus. Using this method, Microsporidia appear as ovoid, refractile spores with bright red walls; some have a belt-like stripe. Another method is the rapid Gram Chromotrope stain that requires only 10 min and combines the Chromotrope method with a Gram-stain. Here, the spores stain dark violet, and the equatorial stripe is enhanced. Microsporidium spores can be identified in tissue obtained by biopsy or at autopsy. Although the organisms can be detected on H&E preparations, special stains used to detect Microsporidia include the Brown-Brenn stain, Warthin-Starry stain, Giemsa, and trichrome blue. Fluorochrome stains, including Calcofluor white and Uvitex 2B have a high affinity for chitin in Microsporidium walls and can be used in urine, stool, mucus, and tissue sections. Clinical aspects: The main manifestations of E. bieneusi and E. intestinalis infection are chronic nonbloody diarrhea, anorexia, weight loss and bloating. Some patients experience intermittent diarrhea, and a few excrete microsporidium spores in the absence of diarrhea. The stool is watery or soft, and 3 to 7 bowel movements per day is usual, but rarely up to 20 per day can occur. About half of patients report abdominal pain, some with nausea and vomiting. Physical findings are nonspecific. Extraintestinal E. bieneusi has been detected in the biliary tree and gallbladder. In contrast, E. intestinalis can spread to the kidneys and other tissues lacking a luminal connection to the intestines, yet intestinal symptoms predominate. Albendazole is the drug of choice. When used to treat infections due to E. intestinalis, it is associated evidence of clearance in the intestine and weight gain. No consistently effective therapies exist for E. bieneusi. Although albendazole is reported to reduce frequency and volume of diarrhea and stabilize the weight of patients with E. bieneusi infection in some studies, this is not associated with clearance of the organism in stool. Pathogenesis: Microsporidium spores possess a unique organelle called the polar tubule. Once ingested or inhaled, the spore extrudes its polar tubule injecting the infective sporoplasm into the eukaryotic host cell. Inside the cell, the sporoplasm undergoes extensive multiplication either by merogony (binary fission) or schizogony (multiple fission). This development can occur either in direct contact with the host cell cytoplasm (e.g., E. bieneusi) or inside a parasitophorous vacuole (e.g., E. intestinalis). Whether free in the cytoplasm or inside a parasitophorous vacuole, microsporidia develop by sporogony into mature spores. During sporogony, a thick spore wall forms which resists adverse environmental conditions. When the spores increase in number and completely fill the host cell cytoplasm, the cell membrane is disrupted and the spores are released into the surroundings. The free mature spores infect new cells thus continuing the cycle. References: CDC Microsporidiosis website. Koneman's Color Atlas and Textbook of Diagnostic Microbiology, 6th edition. LWW, 2005. Mandell GL, Bennett JE and Dolin R. Principles and Practice of Infectious Diseases, 6th edition. Churchill Livingstone, 2004. McPherson RA and Pincus, MR. Henry’s Clinical Diagnosis and Management by Laboratory Methods, 25th edition. Elsevier, 2007. Weber R and Bryan RT. Microsporidial infections in immunodeficient and immunocompetent patients. Clin Infect Dis 1994 Sep; 19(3): 517-21. Weber R, Bryan RT, Schwartz, DA and Owen, RL. Human Microsporidial Infections. Clin Microbiol Rev 1994 Oct;7(4):426-61.