The Management of Cervical , Vulvar and Vaginal Cancers
advertisement
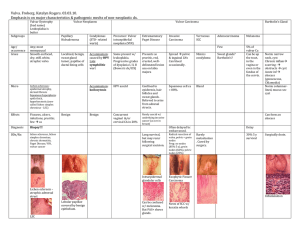
The Management of Cervical , Vulvar and Vaginal Cancers Kerry J. Rodabaugh, M.D. Division of Gynecologic Oncology University of Nebraska Medical Center Incidence: global public health issue 450,000 – 500,000 women diagnosed each year worldwide In developing countries, it is the most common cause of cancer death 340,000 deaths in 1985 United States Incidence 15,000 women diagnosed annually 4,800 annual deaths Mortality Rates • <2/100,000: Finland, France, Greece, Israel, Japan, Korea, Spain, Thailand • 2.7/100,000: USA • 12-15.9/100,000: Chile, Costa Rica, Mexico Lifetime risk of developing cervical cancer 5% - South America 0.7% - USA Cervical CA Risk Factors • • • • • • • Early age of intercourse Number of sexual partners Smoking Lower socioeconomic status High-risk male partner Other sexually transmitted diseases Up to 70% of the U.S. population is infected with HPV Screening Guidelines for the Early Detection of Cervical Cancer, American Cancer Society 2003 • Screening should begin approximately three years after a women begins having vaginal intercourse, but no later than 21 years of age. • Screening should be done every year with regular Pap tests or every two years using liquid-based tests. • At or after age 30, women who have had three normal test results in a row may get screened every 2-3 years. However, doctors may suggest a woman get screened more if she has certain risk factors, such as HIV infection or a weakened immune system. • Women 70 and older who have had three or more consecutive Pap tests in the last ten years may choose to stop cervical cancer screening. • Screening after a total hysterectomy (with removal of the cervix) is not necessary unless the surgery was done as a treatment for cervical cancer. American Cancer Society. Cancer Facts & Figures. 2004. Atlanta, GA; 2005 Pap Smear • Single Pap false negative rate is 20%. • The latency period from dysplasia to cancer of the cervix is variable. • 50% of women with cervical cancer have never had a Pap smear. • 25% of cases and 41% of deaths occur in women 65 years of age or older. Clinical Presentation • • • • • • CIN/CIS/ACIS – asymptomatic Irregular vaginal bleeding Vaginal discharge Pelvic pain Leg edema Bowel/bladder symptoms Physical Findings • Exophytic, cauliflower like mass • Cervical ulcer, friable or necrotic • Firm “barrel-shaped” cervix • Hydronephrosis • Anemia • Weight loss Histology Squamous 85-90% Adenocarcinoma 10-15% Lymphoma Neuroendocrine/small cell Melanoma Route of Spread Cervical cancer spreads by direct invasion or by lymphatic spread Vascular spread is rare Staging • • • • • • Physical exam Cervical biopsies Chest x-ray IVP (Ct scan) Barium enema, cystoscopy, proctoscopy Surgical staging Staging Stage I – confined to the cervix IA1 – <3mm depth of invasion IA2 – stromal invasion 3-5mm in depth or <7 mm in width IB1- tumor < 4 cm IB2 - tumor > 4 cm in diameter Stage II – extension beyond cervix IIA – upper 2/3 of vagina IIB – Parametrial involvement Staging Stage III IIIA – lower 1/3 of vagina IIIB – extension to pelvic sidewall or hydronephrosis Stage IV IVA – bladder or rectal mucosa IVB – distant metastases 5 year survival rates Stage IA Stage IB Stage II Stage III Stage IV 90-100% 70-90% 50-60% 30-40% 5% Therapy Cervical conization Simple hysterectomy Radical hysterectomy Radiation therapy with chemosensitization 5 year Survival • • • • Stage I Stage II Stage III Stage IV 70% 51% 33% 17% Pros and Cons Surgery Bladder dysfunction Vesico/uretero fistula Bowel obstruction Ovarian preservation Vaginal preservation Radiation Sigmoiditis Rectovaginal fistula Bowel obstruction Vesico/uretero fistula Ovarian failure Radiation Therapy External Beam Whole pelvis or para-aortic window 4000-6000 cGy Over 4-5 weeks Brachytherapy Intracavitary or interstitial 2000-3000 cGy Over 2 implants Recurrent Cervical Cancer 10-20% of patients treated with radical hysterectomy Recurrence has an 85% mortality 83% are diagnosed within the first two years of post-treatment surveillance Recurrent Cervical Cancer Radiation Pelvic exenteration Palliative chemotherapy Vulvar Cancer • 3870 new cases 2005 • 870 deaths • Approximately 5% of Gynecologic Cancers American Cancer Society. Cancer Facts & Figures. 2004. Atlanta, GA; 2005 Vulvar Cancer • • • • 85% Squamous Cell Carcinoma 5% Melanoma 2% Sarcoma 8% Others Vulvar Cancer • Biphasic Distribution • Average Age 70 years • 20% in patients UNDER 40 and appears to be increasing Vulvar Cancer Etiology • Chronic inflammatory conditions and vulvar dystrophies are implicated in older patients • Syphilis and lymphogranuloma venereum and granuloma inguinal • HPV in younger patients • Tobacco Vulvar Cancer • Paget’s Disease of Vulva – 10% will be invasive – 4-8% association with underlying Adenocarcinoma of the vulva Symptoms • Most patients are treated for “other” conditions • 12 month or greater time from symptoms to diagnosis Symptoms • • • • • • • • Pruritus Mass Pain Bleeding Ulceration Dysuria Discharge Groin Mass Symptoms • May look like: – – – – – Raised Erythematous Ulcerated Condylomatous Nodular Vulvar Cancer • IF IT LOOKS ABNORMAL ON THE VULVA • BIOPSY! • BIOPSY! • BIOPSY! Tumor Spread • Very Specific nodal spread pattern • Direct Spread • Hematogenous Staging • Based on TNM Surgical Staging – Tumor size – Node Status – Metastatic Disease Staging • Stage I T1 N0 M0 – Tumor ≤ 2cm – IA – IB ≤1 mm depth of Invasion 1 mm or more depth of invasion Staging • Stage II T2 N0 M0 – Tumor >2 cm – Confined to Vulva or Perineum Staging • Stage III – – – – T3 N0 M0 T3 N1 M0 T1 N1 M0 T2 N1 M0 • Tumor any size involving lower urethra, vagina, anus OR unilateral positive nodes Staging • Stage IVA – – – – T1 N2 M0 T2 N2 M0 T3 N2 M0 T4 N any M0 • Tumor invading upper urethra, bladder, rectum, pelvic bone or bilateral nodes Staging • Stage IVB – Any T Any N M1 • Any distal mets including pelvic nodes Treatment • Primarily Surgical – Wide Local Excision – Radical Excision – Radical Vulvectomy with Inguinal Node Dissection • Unilateral • Bilateral • Possible Node Mapping, still investigational Treatment • Local advanced may be treated with Radiation plus Chemosensitizer • Positive Nodal Status – 1 or 2 microscopic nodes < 5mm can be observed – 3 or more or >5mm post op radiation Treatment • Special Tumor – Verrucous Carcinoma • Indolent tumor with local disease, rare mets UNLESS given radiation, becomes Highly malignant and aggressive • Excision or Vulvectomy ONLY Vulva 5 year survival • • • • Stage I Stage II Stage III Stage IV 90 77 51 18 Hacker and Berek, Practical Gynecologic Oncology 4th Edition, 2005 Recurrence • Local Recurrence in Vulva – Reexcision or radiation and good prognosis if not in original site of tumor – Poor prognosis if in original site Recurrence • Distal or Metastatic – Very poor prognosis, active agents include Cisplatin, mitomycin C, bleomycin, methotrexate and cyclophosphamide Melanoma • 5% of Vulvar Cancers • Not UV related • Commonly periclitoral or labia minora Melanoma • Microstaged by one of 3 criteria – Clark’s Level – Chung’s Level – Breslow Melanoma Treatment • Wide local or Wide Radical excision with bilateral groin dissection • Interferon Alpha 2-b Vaginal Carcinoma • 2140 new cases projected 2005 • 810 deaths projected 2005 • Represents 2-3% of Pelvic Cancers American Cancer Society. Cancer Facts & Figures. 2004. Atlanta, GA; 2005 Vaginal Cancer • 84% of cancers in vaginal area are secondary – – – – – Cervical Uterine Colorectal Ovary Vagina Fu YS, Pathology of the Uterine Cervix, Vagina and Vulva, nd Vaginal Carcinoma • • • • Squamous Cell Clear Cell Sarcoma Melanoma 80-85% 10% 3-4% 2-3% Clear Cell Carcinoma • Associated with DES Exposure In Utero – DES used as anti abortifcant from 1949-1971 – 500+ cases confirmed by DES Registry – Usually occurred late teens Vaginal Cancer Etiology • Mimics Cervical Carcinoma – HPV 16 and 18 Staging • Stage I • Stage II Confined to Vaginal Wall Subvaginal tissue but not to pelvic sidewall • Stage III Extended to pelvic sidewall • Stage IVA Bowel or Bladder • Stage IVB Distant mets Treatment • Surgery with Radical Hysterectomy and pelvic lymph dissection in selected stage I tumors high in Vagina • All others treated with radiation with chemosensitization