Jessica L. Colburn, MD Johns Hopkins School of Medicine
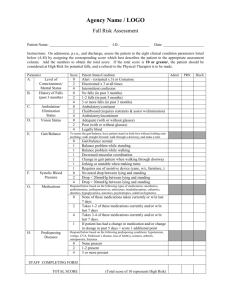
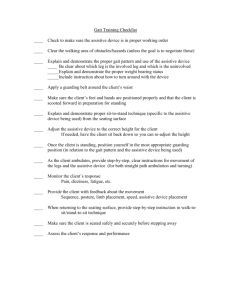
advertisement

Jessica L. Colburn, MD Johns Hopkins School of Medicine Division of Geriatric Medicine & Gerontology April 15, 2015 Discuss prevalence of falls in older adults Develop an approach for fall risk screening and post-fall assessment in older adults Discuss interventions that reduce fall risk in older adults Prevalence Outcomes Risk Factors ◦ Common Medical Conditions ◦ Changes with Aging Screening Evaluation Risk Reduction Community Resources Take Home Points One-third of older adults in the community fall each year One-half of older adults in long term care fall each year Falls are the leading cause of traumatic injuries in adults over the age of 65 Increased mortality secondary to falls with each decade of life Estimated direct medical costs for injuries in older adults due to falls was $32 billion in the year 2013 www.cdc.gov/HomeandRecreationalSafety/Fal ls/fallcost.html 20% need medical attention 5% fractures 5-10% other serious injuries (lacerations, head injuries, dislocations, bleeding) Kannus et al, Lancet 2005 Hip fracture ◦ Increased risk of dying within the 3-6 months following a hip fracture ◦ Functional impairment – 20-30% of older adults do not return to baseline function ◦ Pain, difficult recovery Found down – risk of injury due to delay to medical care, can lead to functional impairment Fear of falling – leads to social withdrawal, admission to long term care facilities Sterling et al, Journal of Trauma 2001 Patients who have fallen in the past year are more likely to fall again Most consistent predictor of future falls is abnormal gait or balance Think about conditions that your patient has that contribute to abnormal gait Ganz et al, JAMA 2007 Patient (Intrinsic) Factors External Factors Medical conditions Medications Age-related changes Alcohol use Cognitive impairment Vision and hearing impairment Falls Using an assistive device improperly Environmental hazards Kannus et al, Lancet 2005 Medical Conditions Parkinson’s disease Stroke Seizures Dementia Depression Dizziness Orthostatic hypotension Arrhythmia Osteoarthritis Diabetes Peripheral neuropathy Age-related changes Changes in balance Vision changes Loss of muscle Cell death in substantia nigra -> reduction in brain dopamine levels Clinical features: ◦ ◦ ◦ ◦ ◦ Tremor at rest (pill-rolling) Cogwheeling rigidity Masked facies Bradykinesia Shuffling gait Treatment: ◦ Symptomatic relief only ◦ Dopaminergic agents Image: careplanning.blogspot.com Early stage – Same fall risk as other community-dwelling older adults Middle stage - patients may forget that they need an assistive device or have knee pain until they get up and start to walk ◦ Lose fine motor skills, forget how to navigate environment Late stage– patients forget how to perform motor tasks like walking or even swallowing ◦ Muscle wasting, weight loss Change in blood pressure with position changes Reflex mechanisms needed to counteract gravity are less effective with age ◦ Vasoconstriction ◦ Elevated heart rate Comorbid medical conditions Medications – beta blockers, diuretics, antihypertensives Volume depletion Image: nlm.nih.gov Very common in older adults Major contributor to gait and balance problems ◦ Joint pain is commonly reported in primary care ◦ Balance changes due to joint abnormalities ◦ Fear of falling Pain control: Acetaminophen is safe ◦ NSAIDs (ibuprofen, naproxen) are less safe due to renal and GI effects ◦ Opiates increase risk of falls and confusion ◦ Physical therapy very useful Tight control in older adults has been shown to increase severe hypoglycemic events and mortality Oral hypoglycemics (except for metformin) and insulin are associated with high rates of hospitalization in older adults Peripheral neuropathy also contributes to falls MEDICATIONS! Antidepressants Sedatives/Pain Meds Benzodiazepines Opiates Antipsychotics Dementia agents (acetylcholinesterase inhibitors) Dopaminergic agents Antihypertensives Diuretics Digoxin Anticholinergics Benadryl Ditropan (incontinence) Polypharmacy Environmental hazards Loose rugs Cords Clutter Low lighting Hand rails Improper use of assist devices Cane Walker Wheelchair/scooter Medications that could increase risk of injury ◦ Blood thinners (benefit may outweigh risk but important to think about) Improper use of assistive devices ◦ Hand-me-down devices Osteoporosis ◦ Increased risk of fracture with a fall Acute fall? Two or more falls in the past year? Difficulty with walking or balance? YES FALL ASSESSMENT YES NO Fall in the past year? NO YES Gait and balance assessment Abnormal ? NO Reassess periodically Adapted from AGS Guideline for Prevention of Falls in Older Persons, 2010 Obtain relevant medical history, physical exam, cognitive and functional assessment Determine multifactorial fall risk: ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ History of falls Feet/footwear Medications Environmental hazards Gait, balance, mobility Visual acuity Other neurologic impairments Muscle strength Heart rate and rhythm Orthostatic hypotension Adapted from AGS Guideline for Prevention of Falls in Older Persons, 2010 How did the fall happen? Did the patient have any symptoms? Was there an injury? Patient risk factors for falls (medical problems, gait imbalance, footwear) Patient risk factors for injury (anticoagulants, osteoporosis) Where there any environmental hazards? Are there any new or problem medications? Any change in mental status or functioning? Moncada LV. Am Fam Phys 2011 Vital signs (orthostatics) Vision exam Cognitive assessment Other neurologic impairments Muscle strength Heart rate and rhythm Gait and balance assessment Watch your patient walk! Drop in systolic blood pressure of 20 mm Hg with position change (sitting to standing) within 3 minutes Five minutes of rest before first blood pressure Drop may be delayed so typically I check immediately with standing and again at 2-3 minutes later Assess for lightheadedness, but not all patients who are orthostatic get lightheaded Snellen chart Pocket card okay Wearing glasses? Glasses appropriate? Reading vs. distance Bifocals may increase fall risk 3 word recall + Clock Draw Test Sensitivity/specificity comparable to using a cutpoint of 25 on the MMSE ◦ Sensitivity 76% (vs 79% MMSE) ◦ Specificity 89% (vs 88% MMSE) Shorter to administer in practice than the MMSE Borson et al, JAGS, 2003 Borson et al, Int Jnl Geri Psych, 2011 Mini-Cog ◦ Give the patient 3 words to remember Banana, chair, sunrise ◦ Administer the Clock Drawing Test – “ten past eleven” or “two forty-five” or “eight twenty” ◦ 3 word recall Scoring: ◦ 1 point for each word recalled (0-3 points) ◦ Clock draw test = 2 points normal, 0 points abnormal ◦ 0-2 = positive screen (“possibly impaired”) ◦ 3-5 = negative screen (“probably normal”) Borson et al, Int Jnl Geri Psych, 2011 Neurologic exam to assess for causes of falls Parkinsonian features Muscle strength Sensation Gait/balance Cardiac examination Evaluation for abnormalities that would affect balance or positioning Irregular heart rhythm Bradycardia or tachycardia Timed Up and Go ◦ Start with patient seated in a chair ◦ Instruct patient to stand, walk 3 meters (10 feet), turn around, come back, and sit down in the chair ◦ Time from when you say go until when patient is re-seated in the chair ◦ Patient may use his or her assistive device Scoring: ◦ >/= 12 seconds associated with increased risk of falls 87% sensitivity & specificity Shumway-Cook et al, PT, 2000 Assess home environment for risks for falling ◦ Rugs, clutter, cords, lighting Consider ways to improve safety in the home environment with assistive devices Initiate multifactorial intervention to address identified risks: Minimize/adjust medications Recommend appropriate exercise program Treat vision impairment (consider cataracts, bifocals) Manage orthostatic hypotension Manage heart rate and rhythm abnormalities Supplement vitamin D Manage foot/footwear problems Modify the home environment Consider risks for injury (osteoporosis, blood thinners) ◦ Provide education and information ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Adapted from AGS Guideline for Prevention of Falls in Older Persons, 2010 Check orthostatics (some patients do not report dizziness) ◦ Goal BP based on JNC 8 guidelines is 140 – 150 systolic, reduce antihypertensives if appropriate ◦ Encourage fluid intake Vision screening Home safety evaluation ◦ Cautious use of bifocals, can increase fall risk especially with navigating curbs and steps ◦ Medicare no longer reimburses for home safety evaluation unless it is done as part of home physical therapy treatment ◦ Can provide instructions for patient/caregiver to assess home environment Vitamin D therapy (Grade B evidence) - 800 IU daily for at least 12 months, regardless of serum level Physical therapy or exercise referral (Grade B evidence) ◦ PT for gait & balance training ◦ Assessment of appropriate assistive device and training to use assistive device ◦ Many types of exercise will reduce falls – Tai Chi, low to high intensity, group or in home, many are effective Multifactorial risk assessment not needed for every patient, tailor interventions to individual needs Moyer, Ann Int Med, 2012 Department of Aging –> Resources for Fitness and Fall Prevention/Risk Reduction ◦ Baltimore County Department of Aging –> Maryland Access Point: 410-887-2594 ◦ Baltimore City Department of Aging -> Maryland Access Point: 410-396-2273 ◦ Senior Centers, exercise programs, fall prevention programs (ie. Stepping On) ◦ Online tools to help patients/caregivers do their own home safety assessments Falls are a common problem for older adults Falls are dangerous – increased risk of functional impairment and death Risk can be modified with screening, assessment, and intervention You can prevent an older adult from falling! Email: ◦ Jessica Colburn, MD ◦ jcolbur1@jhmi.edu Thank you!