Respiratory Emergencies …or all that wheezes is NOT asthma
advertisement

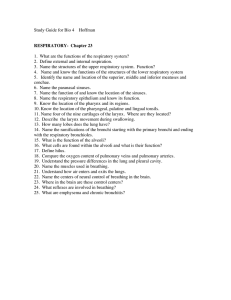
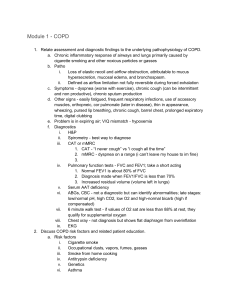
Respiratory Emergencies …or all that wheezes is NOT asthma Definitions Apnea Dypsnea Orthopnea Tachypnea Bradypnea Hypercarbia Acidosis Alkalosis Ventilation Diffusion Perfusion Respiration Anatomy Anatomy Physiology Takes in oxygen Disposes of wastes O2 + Glucose – Carbon dioxide – Excess water The Cell CO2 + H2O Physiology Physiology Inspiration Active process Chest cavity expands Intrathoracic pressure falls Air flows in until pressure equalizes Expiration Passive process Chest cavity size decreases Intrathoracic pressure rises Air flows out until pressure equalizes Physiology Autonomic Function Primary drive: increase in arterial CO2 Secondary (hypoxic) drive: decrease in arterial O2 Adequate Breathing Normal rate and depth Regular breathing pattern Good breath sounds on both sides of lungs Equal chest rise and fall Pink, warm, dry skin Inadequate Breathing Breathing rate < 12 or > 20* Shallow or irregular respirations Unequal chest expansion Decreased or absent lung sounds Accessory muscle usage Pale or cyanotic skin color Cool, clammy skin appearance Obstructive Pathophysiology • • • • Tongue Foreign body obstruction Anaphylaxis and angiodema Facial trauma and inhalation injuries (burns) • Epiglottitis and Croup • Aspiration Restrictive Pathophysiology • Asthma • COPD • Emphysema • Chronic Bronchitis Diffusion Pathophysiology • Pulmonary Edema: • Left-sided heart failure • Toxic inhalations • Near drowning • Pneumonia • Pulmonary Embolism: • Blood clots • Amniotic fluid • Fat embolism Ventilation Pathophysiology • Trauma: rib fractures, flail chest, spinal • • • • • cord injuries Pneumothorax, hemothorax, SCW Diaphragmatic hernia Pleural effusion Morbid obesity Neurological/muscular diseases: polio, MD, myasthenia gravis Control System Pathophysiology • Head trauma • CVA • Depressant drug toxicity • Narcotics • Sedative-hypnotics • Ethyl alcohol FBAO • Obstruction may result from head position, tongue, aspiration, or foreign body. • Be prepared to treat quickly and aggressively. • Head-tilt/chin-lift to open airway Upper Airway Infections • • • • • • • Bronchitis Common cold Diphtheria Pneumonia Croup Epiglottitis Severe Acute Respiratory Syndrome Upper Airway Infections Signs & Symptoms • Dyspnea or respiratory distress • Seal-bark cough • Acute angiodema • Excessive salivation • Stridor • Sniff positioning Acute Pulmonary Edema • Fluid buildup in lungs • History of CHF • High recurrence • Signs & symptoms: • Dypsnea • Frothy, pink sputum • Pedal edema, ascities • Rales, wheezes • Hypertension . Pedal Edema Ascites Bronchitis • Chronic condition similar to emphysema • Reduction in ventilation due to increased mucus production. • Productive cough, copious sputum • “Blue bloaters” • Treatment goals: relief of hypoxia, reversal of bronchoconstriction COPD • Damaged lungs from repeated infections or inhalation of toxic agents. • Signs & symptoms: • • • • • Chronic cough Rhonchi, wheezing SpO2 88-92% Clubbing Pursed lip breathing Clubbing Asthma • Common but serious disease • Acute bronchiole constriction with increased mucus production • Signs & symptoms: • Wheezing • Patient looks tired • Cyanosis Pneumothorax • Spontaneous or trauma induced • Accumulation of air in the pleural space • Signs & symptoms: • Dypsnea • One-sided chest pain • Absent or decreased breath sounds Anaphylaxis • Characterized by respiratory distress and hypotension • Usually results from body response to allergen. • Airway obstruction due to angiodema is major concern Pneumonia 5th leading cause of death in the U.S. Infection usually caused by bacteria or virus, rare instances fungal Patient will present with sick appearance, febrile, shaking, productive cough, increased sputum. Patient with increase respiratory rate/effort, tachycardic, wheezes/rales/consolidated lung sounds Pleural Effusion • Collection of fluid outside the lung • Caused by irritation, infection, or cancer • Signs & symptoms: • Dypsnea • Decreased breath sounds over effected area • Positional comfort Pulmonary Embolism • Blood clot that breaks off, circulating through venous system. • Signs & symptoms: • • • • • Dypsnea/tachypnea Cyanosis Acute pleuritic pain Hemoptysis Hypoxia Pulmonary Embolism Hyperventilation • Over-breathing resulting in a decrease in the level of CO2 (alkalosis) • Signs and symptoms: • Anxiety • Tingling in hands & feet (carpal-pedal spasms) • A sense of dypsnea despite rapid breathing • Dizziness • Numbness ARDS • Pulmonary edema caused by fluid accumulation in the interstitial spaces, interfering with diffusion causing hypoxia (fluid balance) • Underlying etiology includes sepsis, pneumonia, inhalation injuries, emboli, tumors • Mortality rate >70% • Supportive care at the BLS level Patient Assessment BSI/Scene Safety Initial Assessment (Sick/Not Sick) Focused Exam Detailed Exam Assessment Treatment and Plan Initial Assessment • Initial Impression: • Body position • Skin signs and color • Respiratory rate and effort • Mental status • Pulse (rate & character) • Determine Sick/Not Sick (Oxygen?) • Identify and correct immediate life threats – ABCS! Focused Exam (S) Signs and symptoms Allergies (med allergies) Medications Past medical history Last meal or intake Events leading to call Focused Exam (S) • Onset • Provocation • Quality • Radiation • Severity • Time Listen to the patient… …they will tell exactly what is wrong! Focused Exam (O) • Vital signs: • Skin (signs of adequate perfusion) • Level of consciousness • Respiratory rate and effort • Lung sounds (SpO2?) • Pulse rate and character • Blood pressure (bilateral?) • Pupillary reaction Focused Exam (O) Crackles (Rales) CHF Pneumonia Rhonchi Pneumonia Aspiration COPD Sometimes Asthma Stridor FBAO Croup Anaphylaxis Epiglottitis Airway burn Wheezing Asthma CHF COPD Focused Exam (O) • Based upon your clinical findings. • Observe the patient while they are talking to you, note any distress. • Watch for critical signs: JVD, tracheal deviation, paradoxial chest movement. Detailed Exam • Complete and thorough head, neck-to-toe exam with non critical patients. • Elicit further information and necessary interventions. • Key in on critical signs! Assessment (A) This is your best guess (or rule out) as to what is going on with the patient. It is based upon YOUR Subjective and Objective findings and should help you develop and implement a Plan. Plan Medics? ABC’s/Monitor vitals Patient in position of comfort. Oxygen via ? Assist with medications. Maintain body temperature. Calm and reassure. Minimize patient movement. Rapid transport! PT Management (P) Golden Rules: • If you are thinking about giving O2, then give it! • If you can’t tell whether a patient is breathing adequately, then they aren’t! • If you’re thinking about assisting a patient’s breathing, you probably should be! • When a patient quits fighting it does not mean that they are getting better! Tools of the Trade