Digestive- (mucosa, etc) and the folds of the small intestine. ... D. 1. I will not go over this anatomical...
advertisement

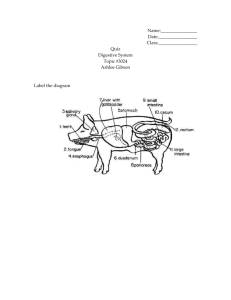
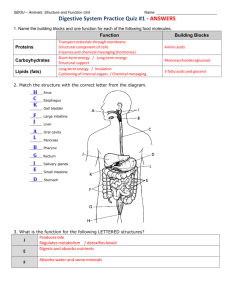
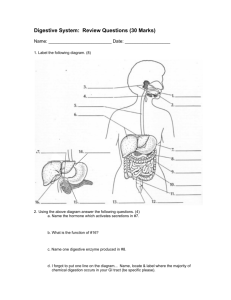
Digestive- Please familiarize/remind yourselves of the linings of the digestive tract (mucosa, etc) and the folds of the small intestine. You can find these on parts I. E. and II. D. 1. I will not go over this anatomical information in class. I. Introduction A. The point of the digestive system is to get nutrients into the body (via the blood). To get into the blood, nutrients need to pass through cells. The process of digestion breaks food into smaller and smaller pieces, until the food is separated into its component nutrient molecules: amino acids, monosaccharides, fatty acids, vitamins, minerals (which are mostly just single atoms, like Na+, K+, and Ca++), and a few other types of molecules like phytochemicals. These molecules are now small enough to pass through cells and enter the bloodstream. Anything that doesn't get broken into small enough pieces passes right through and goes out the other end without giving us any nutrition. For example, we can't digest fiber, so it goes right out the other end (of course, fiber does offer some nice health benefits, it just doesn't offer us any energy). B. The process of absorption describes the component molecules of food moving from the GI tract, across cells, and into the blood. That is, getting nutrients into the body. Virtually all absorption occurs in the small intestine. In order to absorb water-soluble nutrients from food, epithelial cells lining the small intestine must have channels to allow those nutrients in. Like all channels, these channels are specific. So, for example, there are glucose channels, Ca2+ channels, vitamin B12 channels, amino acid channels, etc. Fat-soluble nutrients will be ferried to the lining by bile salts, but then they just diffuse right into the cells. Before these nutrients can be absorbed, however, they must be broken down into small enough pieces to get through the channels or diffuse across. That is what digestion is all about. C. Digestion includes both mechanical (chewing, etc) and chemical (HCl and enzymes) processes. Mechanical digestion just breaks food chunks down into smaller chunks. Enzymatic activity is what gives us the component food molecules. Only carbs, proteins, and fats (triglycerides) require enzymes to break them down. Vitamins and minerals are not long polymers… so they just need to be separated away (not chopped up). The general types of digestive enzymes are: Amylases: hydrolyze starch into disaccharides (NOT absorbable) “Disaccharidases:” Maltase, sucrase, and lactase: hydrolyze disaccharides into monosaccharides (absorbable) Lipases: hydrolyze triglycerides into fatty acids and monoglycerides (absorbable) Proteases: hydrolyze proteins into small peptides (> 3 amino acids NOT absorbable). There are a variety of different proteases; the ones we will consider are: pepsin, trypsin, chymotrypsin, carboxypeptidase. Proteases are always released in an inactive form, and need to be activated once they are in the lumen of the GI tract. Peptidases: hydrolyze small peptides into tripeptides, dipeptides, and amino acids (absorbable) D. The enteric nervous system: the digestive system is innervated by a series of interconnected neurons that bypass the CNS, and operate as short reflexes (reflex arcs that don't go through the CNS). So, once a stimulus arrives to a certain part of the digestive system (ex., stretching of stomach by food), the system can respond on its own (ex, churning of stomach). Of course, we also know that the digestive system is stimulated by the parasympathetic division of the ANS as well (how does the sympathetic division affect it?). E. Linings of the GI tract- from the esophagus down, the GI tract walls are composed of the same basic components: 1. Mucosa- the innermost lining. This is where cells meet food. The mucosa consists of an epithelia and its basement membrane ("lamina propria") and a thin layer of smooth muscle that can move locally. The lamina propria, by the way, carries the blood and lymph capillaries that will pick up nutrients from the interior of the digestive tract. It also houses MALT lymph nodules (Peyer's patches). The epithelium of the GI tract: the mouth, oropharynx, esophagus and rectum are lined with a stratified squamous. The stomach, small intestine and most of the large intestine are lined with a simple columnar. The small intestinal epithelial cells, but not those of the stomach or large intestine, contain microvilli. Why the differences? 2. Submucosa- Dense (irregular) connective tissue, very elastic. Carries larger blood and lymph vessels, as well as nerves and neurons. 3. Muscularis Externa- 2 layers of smooth muscle: >Inner, circular layer: thickened regions form sphincters between sections of the GI tract >Outer, longitudinal layer Together, these layers of muscles propel material through the tract (peristalsis) and aid in mechanical digestion (segmentation, stomach churning). Parasympathetic and sympathetic fibers innervate these muscle layers (how are these muscles [generally] affected by each division?) 4. Serosa- the visceral peritoneum II. The organs and events of the digestive system A. The mouth and pharynx- Salivary glands produce saliva, which contains a variety of substances such as mucus, enzymes and antibiotics. 1. Mechanical digestion: chewing 2. Enzymatic digestion: saliva contains salivary amylase and lingual lipase, so… what gets digested here? 3. Absorption: none! B. Esophagus- a muscular tube connecting the pharynx with the stomach. Peristalsis. Stratified squamous. Separated from the stomach by the esophageal sphincter, which protects the esophagus from stomach acid. 1. Mechanical digestion: none 2. Enzymatic digestion: Starch and fat digestion continues, but no new enzymes and 3. Absorption: none! The esophagus enters the abdominopelvic cavity through a hole in the diaphragm, the esophageal hiatus. C. Stomach 1. Microscopic Anatomy and stomach secretions a. Simple columnar epithelium; the cells lining the stomach are modified goblet cells that secrete huge amounts of mucous with lots of HCO3- embedded in the mucous. b. Gastric pits- invaginations of the epithelium. Along the pits, different types of cells secrete different types of products into the stomach. The "ends" or "bottoms" of the pits are considered gastric glands. c. Gastric pit cell types and their secretions (keep in mind that populations of different types of cells differ between the regions of the stomach) i. Parietal cells- secrete HCl and intrinsic factor. Intrinsic factor is a glycoprotein that "escorts" vitamin B-12 into the bloodstream (without intrinsic factor, you can't absorb B-12). B12, if you recall, supports the growth and maintenance of myelin sheathing. How parietal cells make HCl: Basically, what they do is very similar to what RBC do with CO2. Parietal cells use carbonic anhydrase to drive the reaction CO2 + H2O --> H2CO3. When H2CO3 dissociates into HCO3- and H+, parietal cells send the H+ into the gastric pit (from there, H+ will diffuse into the interior of the stomach). Then, they take the HCO3- and send it to the blood, in exchange for a Cl-. The Cl- is then sent to the gastric pit to follow H+. When the stomach is active, parietal cells send a bunch of HCO3- into the blood. Since HCO3- can bind H+, as they enter the blood in the stomach, they cause a rise in pH. This phenomenon is called the alkaline tide. ii. Chief cells- secrete an inactive protease: pepsinogen. Once in the stomach, pepsinogen is activated by HCl and becomes pepsin, which is an active protease. Chief cells also secrete another type of lipase, gastric lipase. iii. G-cells: secrete gastrin, which stimulates parietal and chief cells as well as stomach muscles. G-cells secrete gastrin into the blood. 3. Protection from acid: the mucosal barrier- stomach cells secrete a thick layer of HCO3- rich mucous, which protects them from HCl. In addition, surface cells die and are replaced every few days, so damage can be quickly repaired. 4. Mechanical Digestion: churning 5. Enzymatic Digestion: HCl activates pepsinogen to pepsin, which is the first protease to be released. So, protein digestion begins in the stomach. In addition, HCl inactivates (denatures) salivary amylase and lingual lipase, so starch digestion stops. Fat digestion continues, however, because of gastric lipase. 6. Other chemical digestion: HCl also denatures dietary proteins, unraveling them a bit, which helps pepsin reach peptide bonds to break them. 7. Absorption: No absorption of nutrients occurs, but some small, lipid soluble substances are absorbed here (most notably aspirin and alcohol). 8. Phases of stomach activity: if anything gets cut from this lecture, this section will be the first to go… stay updated… a. Cephalic Phase- getting ready for food. When you think about eating, or see, smell or hear food, your stomach starts to get active, to make sure it's ready to receive food and start working on it right away. Parasympathetic activity steps up, activating chief cells, mucous cells, parietal cells and G-cells. b. Gastric Phase- dealing with food in the stomach. The enteric nervous system is activated by distention of the stomach and a drop in pH. It will continue to activate secretory cells and will stimulate muscles to start churning motions. Gastrin makes its way through the blood, and when it gets back to the stomach, keeps parietal cells, chief cells, and muscles active. The gastric phase lasts for hours, and the end result is lots of stomach juices and churning. c. Intestinal Phase- Sending food to the small intestine. This is when the stomach starts squeezing chyme into the small intestine. Before we discuss the events, you need to understand a couple of things. The small intestine is not as well protected from stomach acid by mucous. In addition, enzymes in the small intestine work best in a slightly basic environment. So, as soon as chyme enters the small intestine it gets blasted by a stream of HCO3- to neutralize it. It's important that only small bits of chyme enter the small intestine at a time, so that it can be neutralized immediately and completely before going any further into the small intestine. The events of the intestinal phase are designed to control/limit the amount of chyme entering the small intestine. Therefore, we will see that chief cells, parietal cells and G-cells will be inhibited. After chyme has been churning in the stomach for a while, the pylorus contracts, squeezing small amounts of chyme through the pyloric sphincter into the small intestine. As chyme enters the small intestine, the enteric nervous system begins a reflex which will inhibit gastrin production and cause the pyloric sphincter to contract (close). Several hormones are released by enteroendocrine cells of the small intestine. The release of hormones is stimulated by specific types of nutrients in chyme. I am going to list some of them, the stimulus that releases them, and what their effect is. I am going to ask you to choose only one that you will be able to talk about on the exam: Cholecystokinin (CCK)- released in response to fats in chyme. Inhibits chief cells and parietal cells (so, what does that mean in terms of stomach secretions?). Also stimulates the gall bladder and pancreas. Gastric Inhibitory Peptide- released in response to fats and carbs in chyme. Inhibits chief cells, parietal cells, and stomach muscles. Also stimulates the pancreas. Secretin- released in response to a drop in pH in the small intesine. Inhibits chief cells and parietal cells, and increases certain pancreas and liver activity. D. The small intestine and accessory organs 1. The Small Intestine- this is the primary site of digestion and absorption; that is, this is where most digestion and virtually all absorption occurs. a. Microscopic Anatomy, Lining of the small intestinal walls, and absorptive structures. The inner lining of the small intestine has several layers of folding, designed to maximize surface area. The more surface area, the greater the chances that digested nutrients will bump into the wall and pass through cells (be absorbed). Blood and lymph capillaries lie very close to the epithelium, in the lamina propria, ready to pick up nutrients. i. Plicae- large folds of the mucosa and submucosa. ii. Villi- smaller folds of the mucosa. Each plica is covered with villi. Each villus has a specific structure: one layer of epithelial cells called enterocytes meet the interior of the small intestine (lumen). Beneath the enterocytes is the lamina propria. A network of blood capillaries, and one lymph capillary, lie just beneath the enterocytes in the lamina propria. The lymph capillary is called a lacteal. When water-soluble substances pass from the small intestine and through enterocytes during absorption, they will enter blood capillaries. That includes monosaccharides, amino acids, minerals, and water-soluble vitamins. When fat-soluble substances pass from the small intestine and through enterocytes during absorption, they will enter the lacteal. That includes fatty acids, monoglycerides, cholesterol, and fat-soluble vitamins. Fat soluble substances get packaged in enterocytes before they enter the lacteal, but we'll discuss that later. The tiny muscles of the mucosal layer can lengthen and shorten the villi, and "milk" the lacteals (push lymph fluid out). iii. Microvilli- Each individual enterocyte has projections that poke into the intestinal lumen. These are the actual sites of absorption; each microvillus contains protein channels designed to allow digested nutrients to pass from the intestine into the cells. In addition to increasing surface area and allowing absorption to occur, the microvilli contain enzymes that complete carbohydrate and protein digestion (maltase, lactase, sucrase and peptidases). The microvilli are refered to as the brush border. 2. Accessory organs of the small intestine: liver, gall bladder, and pancreas. As an introduction, the liver produces bile, which is then stored in the gall bladder. The pancreas produces digestive enzymes and HCO3-. When chyme enters the small intestine, the pancreas and gall bladder send their products to the duodenum through a duct. a. The liver- The digestive function of the liver is to produce bile, and to receive nutrients and determine their destination. The cells making up the bulk of the liver are called “hepatocytes.” Hepatocytes grow in single layers that look like brick walls. Between the walls are sinusoidal capillaries. In the sinusoids is another type of liver cell, Kupffer cells. These are actually resident macrophages. i. Cell populations and functionsKupffer cells: phagocytize old RBC and pathogens. They are also storage cells, storing iron, heavy metals, and lipids. The hepatocytes: use the sinusoids to put plasma proteins (which they have manufactured) into circulation, -store glucose (as what?), B-12, and fat-soluble vitamins; -detoxify substances like alcohol and urea; -make bile; -remove and break down metabolic substances (such as hormones) and drugs from circulation; perform gluconeogenesis; -monitor and influence blood lipids ii. Bile- bile is a mixture of lots of products coming from the liver. Bile serves a couple of functions: first, it AIDS in fat digestion (but it is not an enzyme; it does not hydrolyze individual triglycerides into fatty acids). Bile also carries waste products to the digestive tract to be excreted in feces, for example bilirubin (remember that?). Bile helps in fat digestion because of bile salts, which are produced by hepatocytes. These molecules have a lipid-soluble (cholesterol based) end, and a water-soluble end. In this way, they are similar to phospholipids. Bile salts surround lipids in the digestive tract with their cholesterol ends, leaving their water soluble ends sticking out. In this way, they suspend lipids in the watery environment of the small intestine. In surrounding lipids, bile salts prevent lipid droplets from reblobbing together, which lipids tend to do in water (think of salad dressing...no matter how much you shake it, the oil still ends up separating from the vinegar). So, bile salts keep lipid droplets small. Why is this important? It allows the maximum number of lipases to work on lipids at once, by increasing the surface area available to those enzymes. Think about lipids as a loaf of bread and lipases as ants. Lets say there are 1000 ants. If they were to work on an unsliced loaf of bread, maybe only 500 ants would be able to fit around the loaf. But, if the bread were sliced and spread out, all 1000 ants would be able to work on it at the same time, making sure that all the bread was accessed. This process is called emulsification. Again, bile salts are not hydrolyzing individual triglycerides; instead, they are limiting how many triglycerides can blob up together. b. The gallbladder- The gallbladder receives bile from the liver via the common hepatic, then cystic duct. Bile is stored in the gall bladder. When chyme enters the small intestine, muscle contractions (stimulated by CCK) squeeze the gallbladder and send bile out through the cystic duct to the common bile duct and through the hepatopancreatic sphincter, into the duodenum. c. The pancreas- The pancreas has both exocrine and endocrine functions. You are already familiar with its endocrine function: areas of the pancreas called Islets of Langerhans contain 2 populations of cells that produce insulin and glucagon, which are released to the blood. As an exocrine gland, the pancreas is composed of a series of ductules that are surrounded by secretory cells. These cells secrete HCO3- and other ions, water, and a full suite of enzymes: pancreatic amylase, pancreatic lipase, 4 inactive proteases (trypsinogen, chymotrypsinogen, and procarboxypeptidase, and proelastase) and nucleases (break down DNA and RNA). The cells lining the ductules secrete the ions (incl. HCO3-) and water. At the end of each ductule is a circle of cells that look like a cul-de-sac. These cells are called acinar cells and they secrete the enzymes. 3. Digestion and Absorption in the small intestine: Chyme enters the duodenum from the stomach and gets blasted with HCO3-, enzymes and bile from the pancreas and gall bladder. Segmentation provides mechanical digestion, keeping chyme sloshing around. Bile salts surround fats, making it easier for lipases to hydrolyze them. Digestive enzymes are sent in from the pancreas. Amylases and lipases start working immediately, but proteases need to be activated. Activation of proteases: Enterocytes secrete an enzyme that will activate trypsinogen to trypsin. Trypsin will then activate each of the other proteases. The active forms of the pancreatic proteases are: trypsin, chymotrypsin, carboxypeptidase, and elastase. Like pepsin, these proteases cleave specific peptide bonds and their actions produce a mixture of single amino acids, dipeptides, and short peptide chains. There is one last processing step that occurs at the brush border (microvilli) before absorption of carbs and proteins occurs. Embedded into the microvilli are the “disaccharidases” and peptidases. They will conduct the final processing of disaccharides and small peptides; then, the products (monosaccharides and absorbable peptides) are right next to their channels and can be absorbed! Lipid absorption is a little different. Lipases hydrolyze triglycerides into fatty acids and monoglycerides. These products are surrounded again by bile salts in a tiny sphere called a micelle. Other fat-soluble nutrients, like cholesterol and fat-soluble vitamins, are trapped in here as well. When micelles contact the intestinal wall, fatty acids and monoglycerides (and other fatty nutrients) are released into enterocytes via diffusion. Once inside the enterocyte, fatty acids are re-attached to monoglycerides, forming triglycerides again! These new triglycerides are surrounded by phospholipids and proteins, into a sphere called a chylomicron. Cholesterol and fat-soluble vitamins are also encapsulated into chylomicrons. Chylomicrons are exocytosed, and enter the lacteal. They won't actually get to the blood until they are dumped into the left subclavian vein. Once most nutrients have been absorbed, 2 waves of peristalsis push whatever is left over into the large intestine. Each wave takes about 2 hours. E. The large intestine- frames the small intestine. The major job of the large intestine is to reabsorb all the water that was thrown into the digestive tract. It also houses bacterial colonies, and we can get a little bit of nutrition from their activities (most notably vitamin K). The large intestine also stores feces. 1. Bacterial Flora- The colon houses bacterial populations, which eat our leftovers. Fiber is one of the major food sources for these bacteria. We get a little bit of nutrition from their activities: vitamin K and a couple of B-vitamins (which are pretty easy to get from food, so they're not really necessary from our bacteria). Our intestinal bacteria are our friends, though. They take up real-estate, helping to prevent pathogens from getting a foothold. Also, it is suspected that some of their metabolic waste products somehow help to protect against cancers and other disorders. Of course, another one of their waste products is gas, and some of them can cause problems if they make it to nearby areas where they don't belong, like the small intestine or the urinary tract. 2. Events in the large intestine- once chyme enters the large intestine through the ileocecal valve, it will be called feces. Feces will spend about 12-24 hours in the large intestine. During that time, most of the water is absorbed. Some additional nutrients can be absorbed here as well. To move feces along, the haustra contract one at a time, pushing feces into the haustrum next door. About 3-4 times daily, a wave of peristalsis pushes everything forward. If you are dehydrated, feces will spend a longer time in the large intestine, as it tries to suck up every last drop of water. On the other hand, if some sort of irritant is detected that could be a pathogen or a toxin, the large intestine will move the feces along very quickly to get it out as fast as possible, and you will get a very strong urge to run to the bathroom screaming, "Get outta my way, I have to go NOW!"