Local Anesthetic Systemic Complications and Treatment
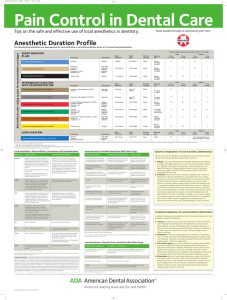
advertisement

Local Anesthetic Systemic Complications and Treatment Adverse Drug Reactions 1) Side effects 2) Overdose reactions 3) Local toxic effects (most common) 4) Allergic reactions Toxicity caused by alteration in the recipient of the drug 1) Disease process 2) Emotional disturbances 3) Genetic aberrations 4) Idiosyncrasy Signs and Symptoms – Toxic Reaction to Local Anesthesia • • • • • • • • Talkativeness Slurred speech Dizziness Nausea Depression Euphoria Excitement Convulsions Overdose Reactions Clinical signs and symptoms that develop as a result of an over-administration of a drug Overdose Contributing Factors • Age • Weight • Other medications • Presence of disease • Genetics • Mental wellbeing Drug Factors • • • • • • • Vasoactivity Concentration Dose Route of administration Rate of injection Vascularity of the injection site Presence of vasoconstrictors Mild Overdose Reaction • • • • • Slow onset Reassure patient Administer oxygen Monitor vital signs Allow patient to recover as long as necessary Slower Onset of Overdose • • • • • • Reassure patient Administer oxygen Monitor vital signs Administer anticonvulsant Call 911 After reaction, have patient examined by a physician • Do not let patient leave alone Severe Overdose Reaction • Rapid onset (within one minute) • Remove syringe (if in the process of an injection) • Protect patient for trauma if convulsions are present • Call 911 • Basic life support • Administer anticonvulsant • Allow patient to recover • Do not let patient leave alone Epinephrine Overdose Very rare for patient to experience an epinephrine overdose Signs and Symptoms of Epinephrine Overdose • • • • • • • • • • • Fear, anxiety Tenseness Restlessness Throbbing headache Tremor Perspiration Weakness Dizziness Pallor Respiratory difficulty Palpitations Management of Epinephrine Overdose • • • • • Terminate dental procedure Sit patient upright in the dental chair Reassure patient Monitor blood pressure Administer oxygen Allergic Reactions to Local Anesthetic Agents • Hypersensitive state as a result of exposure to an allergen • Re-exposure can heighten the initial reaction Clinical Manifestations of an Allergy • • • • • • • Fever Angioedema Urticaria Dermatitis Depression of blood-forming organs Photosensitivity Anaphylaxis Angioedema Urticaria (hives) Allergy • Incidents of allergy are low • Often allergic reaction is to one of the ingredients within the cartridge, not the local anesthesia itself How to Prevent An Allergic Reaction • Take a thorough medical history • Dialogue the medical history with the patient Common Questions to Ask the Patient • Allergic to any medications? • Have you ever had a reaction to local anesthesia? • If yes, describe what happened • Was treatment given? If so, what? Allergic Responses to local anesthetic • • • • Dermatitis (hives) Bronchospasm Systemic anaphylaxis Hypersensitivity to esters (atypical pseudo cholinesterase, PABA) Latex Allergy • The cartridge opening into which the needle is inserted is aluminum with a very thin diaphragm of latex in the middle • Though patients with a latex allergy are at an increased risk, there are no known cases or reports of an allergic response from the latex on a local anesthetic cartridge Asthma Patient • Thorough medical and dental history • Avoid use of anesthesia that contain epinephrine or levonordefrin because of sulfites (may cause wheezing) • Asthma patient that is steroid dependant may develop brochospasms • Establish rapport and calm environment Renal Disease Common diseases associated with renal failure are diabetes mellitus, hypertension, or systemic lupus erythematosus (SLE) Kidneys are compromised Drugs Metabolized by the Liver • • • • Lidocaine (Xylocaine) Prilocaine (Citanest) Mepivacaine (Carbocaine, Polocaine) Bupivacaine (Marcaine) • Appear to be safe for use on patients with liver disease when used in appropriate amounts Pregnancy • Anesthesia crosses the placenta and could be toxic to the fetus, but is not a known teratogen • No drug should be administered during pregnancy especially the first trimester • If treatment is necessary, local anesthetics with epinephrine are considered relatively safe for use during pregnancy; check with patient’s physician • Educate patients to the potential risks (document) FDA Category of Prescription Drugs Drug Category Use During Pregnancy Risk Lidocaine B Yes - Prilocaine B Yes - Mepivacaine C Use with cautionConsult physician Fetal bradycardia Bupivacaine C Use with cautionConsult physician Fetal bradycardia Hypertension • Stress and anxiety may raise the patient’s blood pressure (>160/100) • Thorough medical, dental and patient history • Norepinephrine and levonordefrin should not be used because of alpha1 stimulation (2% Mepivacaine with 1:20,000 levonordefrin) • Up to two cartridges of 2% lidocaine with 1:100,000 epinephrine is safe Contraindication for Local Anesthetic with Epinephrine • • • • Uncontrolled hypertension Myocardial infarction (within 6 months) Unstable angina Coronary artery bypass graft (> 3 months) Quiz 1. Local anesthetics and vasoconstrictors do cross the placenta in pregnant women; local anesthetics and vasoconstrictors are known teratogens (cause birth defects). a. The first part of the statement is true, the second part is true. b. The first part of the statement is true, the second part is false. c. The first part of the statement is false, the second part is false. d. The first part of the statement is false, the second part is true. 2. What should you do when using local anesthesia on a patient with controlled hypertension? a. Take the BP before the injection and use Mepivacaine only b. Take the BP before the injection and use an anesthetic without a vasoconstrictor c. Take the BP before the injection and use anesthetic with a vasoconstrictor judiciously d. Local anesthetics should not be used on patients with hypertension 3. Since local anesthetics are excreted through the kidneys, what is true concerning giving local anesthesia to a patient with renal dysfunction? a. Consult patient’s physician b. Potential for overdose c. Use anesthetics in minimal doses d. All of the above 4. What is the most common reason for allergies to local anesthetic solutions? a. Asthma b. The anesthetic solution itself c. The other added ingredients to the solution d. The vasoconstrictor 5. To prevent an overdose, what should the maximum safe doses of anesthetic be based on? a. The patient’s age b. The patient’s weight c. The patient’s physical status d. The patient’s health e. All of the above