INVASIVE HEMODYNAMIC MONITORING
advertisement

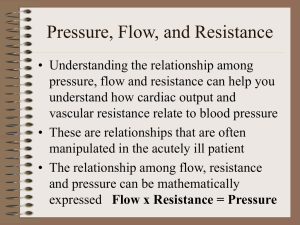
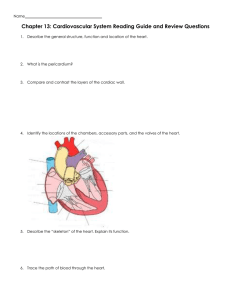
INVASIVE HEMODYNAMIC MONITORING Presentation by Donna Cohen, BSN, RN Heart and Vascular Center Medical University of South Carolina February 2006 INVASIVE HEMODYNAMIC MONITORING Objectives Verbalizes purposes of Hemodynamic Monitoring Verbalize indications for Hemodynamic Monitoring Identify components of a Pulmonary Artery Catheter[Swan-Gantz] Verbalize necessary equipment needed Objectives [con’t] Identify the correct pressure waveforms Identify the components of invasive hemodynamic monitoring[RA,PA,PAM and PCWP] Identify “normal” parameters for each component of monitoring Verbalize how to troubleshoot abnormal waveforms Objectives [con’t] Verbalize definition of preload and afterload Verbalize what and where to document data collected Verbalize understanding of the Critical Care Hemodynamic Monitoring Policy [C1] Introduction Swan-Ganz catheter has been in use for almost 30 years Initially developed for the management of acute myocardial infarction Now, widespread use in the management of a variety of critical illnesses and surgical procedures Purposes of Invasive Hemodynamic Monitoring Early detection, identification, and treatment of life-threatening conditions such as heart failure and cardiac tampanade Evaluate the patient’s immediate response to treatment such as drugs and mechanical support Evaluate the effectiveness of cardiovascular function such as cardiac output and index Indications for Hemodynamic Monitoring Any deficit or loss of cardiac function: such as AMI,CHF,Cardiomyopathy All types of shock;cardiogenic,neurogenic,or anaphylactic Decreased urine output from dehydration, hemorrhage,G.I. bleed,burns,or surgery Components of a Pulmonary Artery Catheter Components of Swan-Ganz [con’t] Normally has four[4] ports Proximal port – [Blue] used to measure central venous pressure/RAP and injectate port for measurement of cardiac output Distal port – [Yellow] used to measure pulmonary artery pressure Balloon port – [Red] used to determine pulmonary wedge pressure;1.5 special syringe is connected Infusion port – [White] used for fluid infusion Components of the Monitoring System Bedside monitor – amplifier is located inside. The amplifier increases the size of signal Transducer – changes the mechanical energy or pressures of pulse into electrical energy; should be level with the phlebostatic axis[ you can estimate this by intersecting lines from the 4th ICS,mid axillary line Recorder – please record information Phlebostatic Axis Commonly used Terminology Preload Afterload Cardiac Output Cardiac Index Systemic Vascular Resistance [SVR] Pulmonary Vascular Resistance [PVR] Preload Is the degree of muscle fiber stretching present in the ventricles right before systole Is the amount of blood in a ventricle before it contracts; also known as “filling pressures” Left ventricular preload is reflected by the PCWP Right ventricular preload is reflected by the CVP [RA] Afterload Any resistance against which the ventricles must pump in order to eject its volume How hard the heart [either side left or right] has to push to get the blood out Also thought of as the “ resistance to flow” or how “clamped” the blood vessels are Cardiac Output/Index Is the amount of blood ejected from the ventricle in one minute Two components multiply to make the cardiac output: heart rate and stroke volume [amount of blood ejected with each contraction] Cardiac index is the cardiac output adjusted for body surface area (BSI) Computation Constant Computation constant is based on the 1) type of catheter 2) temperature (iced or room temp) of the injectate 3) the number of mL’s (5mL vs 10mL) ---we use 10 mL of room temperature injectate for our regular swanns, which requires a computation constant of 0.592 SVR / PVR Systemic Vascular Resistance – reflects left ventricular afterload Pulmonary Vascular Resistance – reflection of right ventricular afterload Many of the drugs we administer will affect Preload, Afterload, SVR/PVR, Cardiac Output Possible Complications Increased risk of infections – same as with any central venous lines—use occlusive dressing and Biopatch to prevent Thrombosis and emboli-- air embolism may occur when the balloon ruptures, clot on end of catheter can result in pulmonary embolism Catheter wedges permanently—considered an emergency, notify MD immediately, can occur when balloon is left inflated or catheter migrates too far into pulmonary artery (flat PA waveform)…can cause pulmonary infarct after only a few minutes! Ventricular irritation – occurs when catheter migrates back into RV or is looped through the ventricle, notify MD immediately…can cause VT Troubleshooting Dampened waveform –can occur with physical defects of the heart or catheter; can be caused by kinks, air bubbles in the system, or clots Solution: Check your line for kinks & air bubbles, aspirate (not flush) for clots, straighten out tubing or patient as much as possible No waveform – can occur with non-perfusing arrhythmias or line disconnection Solution: Check your line for disconnection, check your patient for pulse, could also be wet transducer or broken cable or box Equipment Needed SET-UP FOR HEMODYNAMIC PRESSURE MONITORING 1. Obtain Barrier Kit, sterile gloves, Cordis Kit and correct swan catheter. Also need extra IV pole, transducer holder, boxes and cables. 2. Check to make sure signed consent is in chart, and that patient and/or family understand procedure. 3. Everyone in the room should be wearing a mask! 4. Position patient supine and flat if tolerated. 5. On the monitor, press “Change Screen” button, then select “Swan Ganz” to allow physician to view catheter waveforms while inserting. 6. Assist physician (s) in sterile draping and sterile setup for cordis and swan insertion. Equipment Needed 7. Set up pressure lines and transducers [see Critical Care Skills: Clinical Handbook, Second Edition pages 293 -298] Please level pressure flush monitoring system and transducers to the phlebostastic axis. Zero the transducers. Also check to make sure all connections are secure. 8. Connect tubings to patient [PA port and CVP port] when physician is ready to flush the swann. Flush all ports of swann before inserting. 9. While floating the swann, observe for ventricular ectopy on the monitor, and make physician aware of frequent PVC’s or runs of VT ! 10. After swann is in place, assist with cleanup and let patient know procedure is complete. Equipment Needed 11. Obtain your RA [CVP], PAS/D, PAM, and wedge. For Cardiac Outputs, inject 10 mLs of D5W after pushing the start button, repeat X 3. Delete outputs not within 1 point of the mean value. Can use .9NS instead, but affects the accuracy of the output reading. 12. Before obtaining the cardiac output, please check the computation constant [should read 0.692 for regular yellow swans; 0.692 for SVO2 or blue swanns] 13. Perform hemocalculations (enter today’s height and weight). 14. Document findings on the ICU flowsheet. PA Insertion Waves Central Venous Pressure (CVP) Zero transducer to the patient’s phlebostatic axis Always read CVP at end expiration CVP is a direct measurement of right ventricular end diastolic pressure Right Ventricular Waveform If the swan falls or gets pulled back into the RV it is considered a swan emergency. If you see an RV waveform (looks like VT) pull the swan immediately. If the swan remains in the RV it may cause the patient to go into VT. Pulmonary Capillary Wedge Pressure (PCWP) Zero the transducer to the patient’s phlebostatic axis. Measure the PCWP at end expiration PCWP should not be higher than PA diastolic PCWP is an indirect measurement of left ventricular end diastolic pressure. Cardiac Output It is the amount of blood pumped by the heart in one minute. Calculated by multiplying heart rate times stroke volume. Cardiac Index is the cardiac output adjusted for body surface area. How to read a PA waveform Measured at end expiration! Dicrotic notch (closure of PulmonicValve) should always be on Right side of wave (if notch on Left side find out if the tip in the RV) Measure PAS at the top of the wave upslope (at end of QRS); PAD is measured at the trough preceding the systolic peak (be careful not to measure whip in the wave) How to read a PCWP (aka wedge) Measured at end expiration! After balloon is inflated, compare waveform to respiratory waveform to determine measurement at the end of expiration (last clear wave before patient inspires) Tip: if waveform is difficult to read, try resting hand on pt’s chest as you wedge; determine where the end of expiration occurs on the wedge waveform, then measure across several waves for consistency Documentation Document PAS, PAD, and PCWP on nursing flowsheet under Hemodynamic Parameters PCWP will rarely be > PAD (if so, means blood is flowing backwards) If PCWP = PAD, look for tamponade Under circumstances where the catheter will not wedge (or should not be), do not document any values in the PCWP column on the flowsheet If you use the PAD measurement for calculations, it is acceptable to write ONLY “PAD value used for calculations” at the top of your numbers