Chapter 19. Vessels and Circulation BIOL242
advertisement

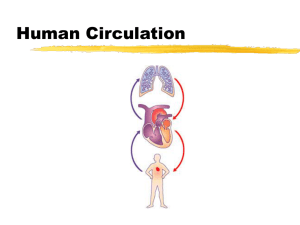
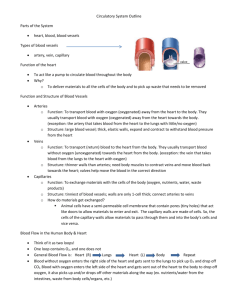
Chapter 19. Vessels and Circulation BIOL242 Lab Pracicum Weds.? • On Chap 16 – 19 (Endocrine & Cardiovascular Lab) • Lab Practical, 24 Oct. Weds on 16 -19 (Lab schedule says “No Lab Scheduled”) Overview • Classes of blood vessels and their structures • Cardiovascular physiology • Circulatory pressures • Capillary exchange • Cardiovascular regulation • Vascular diseases • Vessels to know (repeat from lab) Blood Vessels • Closed system of tubes that starts and ends at the heart Arteries: large vessels that carry blood away from heart Arterioles: smallest branches of arteries Capillaries: smallest blood vessels with a small diameter and thin walls; location of exchange between blood and interstitial fluid (exchange vessels) Venules: smaller branches of veins collect blood from capillaries Veins: Larger vessels that return blood to heart Structure of Vessel Walls Figure 21-1 Generalized Structure of Blood Vessels • Arteries and veins are composed of three tunics – tunica interna, tunica media, and tunica externa • Lumen – central blood-containing space surrounded by tunics • Capillaries are composed of endothelium with sparse basal lamina Artery and Vein Walls – 3 layers • Tunica Interna (Intima): innermost layer – endothelial lining of all vessels – In vessels larger than 1 mm, a subendothelial connective tissue basement membrane is present – In arteries only the internal elastic membrane is a layer of elastic fibers in outer margin • Tunica Media: middle layer – concentric sheets of smooth muscle in loose connective tissue – regulated by sympathetic nervous system – Controls vasoconstriction/vasodilation of vessels – External elastic membrane (arteries only) separates tunica media from tunica externa – Thickest layer in a small artery Artery and Vein Walls – 3 Layers • Tunica Externa (adventitia): outer layer – – – – Connective tissue sheath with collagen fibers Anchors vessel to adjacent tissues Thick in veins Larger vessels contain vasa vasorum • In arteries: – collagen fibers – elastic fibers • In veins: – elastic fibers – smooth muscle cells Vasa Vasorum • Small arteries and veins found in the walls of large arteries and veins • These are the blood supply for the large vessels • Supply cells of tunica media and tunica externa with oxygen and nutrients • Why don’t you need these in capillaries? Arteries vs. Veins at a glance • Arteries and veins run side-by-side • Arteries have thicker walls and higher blood pressures • Collapsed artery has small, round lumen • Vein has a large, flat lumen • Vein lining contracts, artery lining does not • Artery lining folds • Arteries more elastic • Veins have valves • Arteries thick t. media, veins thick t. externa Vessel Composition Arteries • Elasticity allows arteries to absorb pressure waves that come with each heartbeat • Contractility: arteries change diameter, controlled by sympathetic division of ANS – Vasoconstriction: contraction of arterial smooth muscle by the ANS, shrinking lumen – Vasodilation: The relaxation of arterial smooth muscle, enlarging lumen Vasoconstriction and Vasodilation • Active processes that affect: – afterload on heart (how?) – peripheral blood pressure (how?) – capillary blood flow Note: elasticity of the arteries also allows them to expand and contract passively in response to changes in blood pressure Structure of Blood Vessels Figure 21-2 Vascular Components Artery Characteristics • From heart to capillaries, arteries change characteristics (along a continuum): – Elastic arteries (conducting arteries) • Large vessels (e.g. and aorta) dmax = 2.5cm, lumen allow lowresistance conduction of blood • Contain elastin in all three tunics • Withstand and even out large blood pressure fluctuations • Serve as pressure reservoirs • Tunica media has many elastic fibers and few muscle cells – Muscular arteries (distribution arteries) • • • • Medium-sized davg =0.4cm Account for most arteries Thick tunica media has many muscle cells Active in vasoconstiction – Arterioles (resistance vessels) • Smallest arteries (d ≤ 30 micons) • Have little or no tunica externa, thin or incomplete media • Control blood flow into capillaries by change diameter in response to ANS, local conditions Artery Diameter and Resistance • Small muscular arteries and arterioles change diameter with sympathetic or endocrine stimulation (vasomotor response) – Decreasing diameter increases resistance, the force opposing blood flow – Arterioles also called resistance vessels Aneurysm • Bulge in an arterial wall • Caused by weak spot in elastic fibers • Pressure may rupture vessel Capillaries • Are smallest vessels with thin walls (davg = 8 microns) • We have about 10 billion or 25,000 miles • Have only a tunica interna, one cell thick • Pericytes on the outer surface stabilize their walls • Microscopic capillary networks permeate all active tissues • Blood flow through caps is slow (why?) • Exchange occurs here: materials diffuse between blood and interstitial fluid • All living cells no more than 125 um from a cap 3 Types of Capillaries • Continuous – Abundant in skin and muscles – Have complete endothelial lining, connected by tight junctions – Small clefts permit diffusion of water, small solutes, and lipid soluble material (but NOT blood cells or plasma proteins) – thymus and brain have specialized continuous capillaries (barriers) • Fenestrated – Have pores in endothelial lining (not gaps between cells) – Permit more rapid exchange of water and larger solutes between plasma and interstitial fluid – Found in: choroid plexus, kidneys, intestinal tract, and? • Sinusoids – Modified fenestrated capillaries – Very leaky, with large gaps between adjacent endothelial cells that allow large molecules (plasma proteins) and cells through – Found only in: Liver, spleen, bone marrow, other lymphoid tissues, used for phagocyte monitoring, plasma protein entry from liver Capillary Structure Figure 21-4 Capillary Networks • One arteriole gives rise to several capillary beds • Each Capillary bed connects 1 arteriole to 1 venule • Each capillary entrance guarded by precapillary sphincter Capillary Bed – key parts • Capillaries – 10 to 100 capillaries per capillary bed, they branch off the metarteriole and return to the thoroughfare channel at the distal end of the bed • Thoroughfare Channels – Are direct capillary connections between arterioles and venules – Controlled by smooth muscle segments called metarterioles found at channel entrance • Collaterals – Multiple arteries contribute to one capillary bed and allow circulation if one artery is blocked – Arterial anastomosis = fusion of two collateral arteries • Arteriovenous Anastomoses – direct connections between arterioles and venules allow blood to bypass the capillary bed Capillary Networks Figure 21-5 Precapillary Sphincters • Guards entrance to each capillary • Open and close, causing capillary blood to flow in pulses • Vasomotion: – Contraction and relaxation cycle of capillary sphincters – Causes blood flow in capillary beds to constantly change routes – Contract/relax on the order of 10 times/min – Causes capillary flow to pulse – Controlled by autoregulation (see later) Closed precapillary sphincters Capillary Volume • At rest, blood is flowing in about 25% of your capillaries • When you begin to exercise, vessels must redistribute blood within the capillary network (you can’t just open up more capillaries) • If all your capillaries open at once: shock Veins • Collect blood from capillaries in all tissues and organs and return it to heart • Larger in diameter than arteries, but have thinner walls and much lower blood pressures • Tunica externa is usually thickest layer • Capacitance vessels (blood reservoirs) that contain 65% of the blood supply • Classified on the basis of size Vein Characteristics • Venules – Collect blood from capillaries – Average diameter of 20 um, resemble capillaries in structure – Allow fluids and WBCs to pass from the bloodstream to tissues • Medium Sized Veins – thin tunica media and few smooth muscle cells – Thickest part is tunica externa with longitudinal bundles of elastic fibers and collagen – Size ranges from 2 – 9 mm • Large Veins (e.g. sup/inf vena cava) – have all 3 tunica layers – thick tunica externa with thin tunica media Vein Valves • • • • Valves are folds of tunica interna Resemble semilunar heart valves Prevent blood from flowing backward Compression from muscular contractions (even rotation in isometric contractions) pushes blood toward heart • Not so important when lying down • Compartmentalize blood flow: blood return from below heart is like a boat traversing several locks to get up a hill Valves in the Venous System Figure 21-6 Blood Distribution Figure 21-7 Blood Distribution • Heart, arteries, and capillaries: – 30 – 35% of blood volume • Venous system: – 60 – 65% – Fully ⅓ of venous blood is in the large venous networks of the liver, bone marrow, and skin (some of this is part of the venous reserve) Capacitance • The ability to stretch or the relationship between blood volume and blood pressure • Veins (capacitance vessels) stretch more than arteries (8x as much as arteries) • Lower resistance = higher capacitance = expands easily at low pressures • Means veins can accommodate large changes in blood volume Veins Response to Blood Loss • Vasomotor centers (medulla) stimulate sympathetic nerves • Venoconstriction = smooth muscles in systemic medium sized veins constrict • Affects blood pressure in venous system but major effect is to cause veins in liver, skin and lungs to redistribute venous reserve back to arterial system (about 20% of total blood) Cardiovascular Physiology Figure 21-8 Cardiovascular Physiology • Cardiac output = blood flow – Determined by pressure and resistance in the cardiovascular system – Force is proportional to pressure gradient resistance • Pressure (P) = force the heart generates to overcome resistance • Absolute pressure is less important than pressure gradient • Pressure Gradient (P) = the difference between pressure at the heart and pressure at peripheral capillary beds Blood Flow, Pressure, and Resistance • Blood flow (F) is directly proportional to the difference in blood pressure (P) between two points in the circulation – If P increases, blood flow speeds up; if P decreases, blood flow declines • Blood flow is inversely proportional to resistance (R) – If R increases, blood flow decreases • R is more important than P in influencing local blood pressure • The differences in pressure within the vascular system provide the driving force that keeps blood moving, always from higher to lower pressure area Measuring Pressure • Blood pressure (BP): – arterial pressure (mm Hg) – Pressure required to move blood • Capillary hydrostatic pressure (CHP): – pressure within the capillary beds – pressure where diffusion and osmosis occur • Venous pressure: – pressure in the venous system • Circulatory Pressure: ∆P across the systemic circuit (about 100 mm Hg) Resistance • Resistance – opposition to flow – Measure of the amount of friction blood encounters – Generally encountered in the systemic circulation – Referred to as peripheral resistance (PR) • Circulatory pressure must overcome total peripheral resistance of entire cardiovascular system which comes from 3 sources: – Vascular resistance (length and diameter) – Blood viscosity – Turbulence Peripheral Resistance: vascular resistance • Vascular resistance (= major factor): R of blood vessels due to friction between blood and vessel walls depends on vessel length and vessel diameter – Adult vessel length is constant – Vessel diameter varies by vasodilation and vasoconstriction – R increases exponentially (4th power!) as vessel diameter decreases (double the radius, decrease resistance by 16x) Peripheral Resistance: viscosity and Turbulence • Viscosity also increases resistance – Normal whole blood viscosity is about 4 – 5 times that of water, changes with hematocrit • Turbulence: swirling action that disturbs smooth flow of liquid – Occurs in heart chambers and great vessels – Atherosclerotic plaques cause abnormal turbulence Overview of Circulatory Pressures: Arteries • Largest pressure gradient is between aorta and proximal end of capillary beds (100 35 mmHg so gradient = 65) • This part of the system also has the highest resistance. • Both the pressure (CO) and the resistance (vasomotor tone) can be regulated, determining the rate of flow in the capillaries Overview of Circulatory Pressures: Capillaries • Blood at the proximal (arterial) side of cap beds has pressure of 35 mmHg • At distal end, where blood enters venules, pressure is 18 mmHg • Low capillary pressure is desirable because high BP would rupture fragile, thin-walled capillaries • Low BP is sufficient to force filtrate out into interstitial space and distribute nutrients, gases, and hormones between blood and tissues Overview of Circulatory Pressures: Veins • Blood entering venules is 18 mmHg, enters right atrium at 0 – 2 mmHg so gradient = 18 mmHg (pretty small) • However, veins provide very low resistance and so they don’t require great pressures for blood to move • As blood gets closer to heart, veins get larger and larger, decreasing resistance. This doesn’t increase the pressure but it does increase the velocity of blood flow Systemic Blood Pressure Figure 19.5 Vessel Diameter Cross-Sectional Area Average Systemic Blood Pressure Systemic Blood Velocity What the graphs show • Arteries capillaries (divergence) • Capillaries veins (convergence) • Blood pressure and velocity are proportional to the TOTAL cross sectional area of all vessels • As total cross-sectional area increases, avg. blood pressures and velocities decline • Velocity continues to decline until the veins, where cross sectional areas increase (reducing friction) • Velocity is slowest at capillaries and flow allows adequate time for exchange between blood and tissues Pressures in the Systemic Circuit • Systolic pressure: – peak arterial pressure during ventricular systole • Diastolic pressure: – minimum arterial pressure during diastole • Pulse pressure: – difference between systolic pressure and diastolic pressure • Mean arterial pressure (MAP): – MAP = diastolic pressure + ⅓ pulse pressure Pressure and Distance • MAP and pulse pressure decrease with distance from heart • Blood pressure decreases with friction • Pulse pressure decreases due to elastic rebound • Near the heart, BP pulses • By the arterioles, pulsing is gone (if you cut a vein it will bleed continuously; an artery spurts) Elastic Rebound • Elastic rebound = Ability of arteries to expand and recoil • Arterial walls: – stretch during systole – rebound during diastole – keeps blood moving during diastole • Dampens the effect of the pulse: – By the time the blood reaches the arterioles, flow is continuous Abnormal Blood Pressure • Hypertension: – abnormally high blood pressure, greater than 140/90 – High diastolic can be very dangerous • Hypotension: – abnormally low blood pressure Venous Return • Amount of blood arriving at right atrium each minute • Both pressure and resistance are low in venous system • Venous BP alone is too low to promote adequate blood return and is aided by – the respiratory pump: pressure changes created during breathing suck blood toward the heart by squeezing local veins. Becomes a larger factor as breathing rate increases. – compression of skeletal muscles, pushes blood toward heart (one-way valves) Capillary Diffusion Routes • • • • • Oxygen and nutrients pass from the blood to tissues Carbon dioxide and metabolic wastes pass from tissues to the blood Water-soluble solutes pass through clefts and fenestrations Lipid-soluble molecules diffuse directly through endothelial membranes Plasma proteins cross endothelial lining in sinusoids only Capillary Exchange • Capillary Exchange is fluid movement between capillaries and interstitial space – Capillary pressure normally forces water and solutes OUT into the tissues – vital to homeostasis, creates and circulates interstitial fluid – moves materials across capillary walls by: • Filtration • Reabsorption (diffusion) Filtration • Filtration: the removal of solutes through a porous membrane, driven by hydrostatic pressure • Hydrostatic pressure = pressure exerted by a fluid (at rest or while flowing) • Capillary filtration: water and small solutes forced through capillary wall, leaving behind larger solutes in bloodstream Capillary Filtration Figure 21-11 Reabsorption • Occurs via osmosis, where water enters the solute compartment with higher osmotic pressure • Solutes in a solvent generate a pressure = Osmotic pressure: – equals pressure required to prevent osmosis – is a pulling force generated by solutes in a solution that cannot cross the membrane Overview: Osmotic and Hydrostatic Pressures • Hydrostatic pressure: – forces water out of a solution compartment • Osmotic pressure: – forces water into a solution compartment • Balance between them controls filtration and reabsorption through capillaries Forces Across Capillary Walls Figure 21-12 Hydrostatic Pressures • Capillary hydrostatic pressure (HPc): pressure within the capillary beds generated by heart pumping – Ranges from 35 at arterial end to 18 at venous end • Interstitial fluid hydrostatic pressure (HPif): pressure generated by mechanical force pushing fluid back into the blood – Different in different tissues but overall average is 0 • Net Hydrostatic Pressure (NHP): The difference between HPc and HPif • HPc is higher, so net pushes water and solutes out of capillaries into interstitial fluid (this is filtration) Osmotic Pressures • Capillary Colloid Osmotic Pressure (OPc) = 25 mmHg normally because suspended plasma proteins are too large to cross capillary walls thus they exert an osmotic pressure that pulls water back into the capillary – Also called oncotic pressure • Interstitial Fluid Colloid Osmotic Pressure (OPif) = effectively zero under normal conditions because there is no pressure exerted by suspended proteins outside cells • Net Colloid Osmotic Pressure (NCOP): The difference between OPc and OPif • OPc is higher and so it pulls water and solutes into capillary from interstitial fluid (this is reabsorption) Net Filtration Pressure (NFP) • NFP – all the forces acting on a capillary bed • The difference between net hydrostatic pressure and net osmotic pressure NFP = (NHP) – (NCOP) NFP = (HPc – HPif) – (OPc – OPif) NFPArt = (35 – 0) – (25 – 0) = +10 mmHg (out) NFPVen = (18 – 0) – (25 – 0) = -7 mmHg (in) Capillary Exchange • At arterial end of capillary bed hydrostatic forces dominate: – fluid moves out of capillary into interstitial fluid = filtration • At venous end of capillary osmotic forces dominate: – fluid moves into capillary out of interstitial fluid = reabsorption • But what about in between? • Transition Point = point along capillary bed where filtration switches to reabsorption. • If this were right in the middle, what would the net result be (filtration, reabsorption?) Capillary Exchange • Since we know which one dominates (right?) the question is, where is the transition point? • Closer to the arterial end or to the venous end? Forces Across Capillary Walls Figure 21-12 Summary: Forces in the capillary bed • Hydrostatic pressure tends to push water and solutes OUT OF blood, into interstitial fluid • Colloid osmotic pressure tends to pull water and solutes INTO capillary • Net filtration pressure is the difference between the NHP and NCOP • At proximal end, NHP is higher • At distal end, NCOP is higher The Transition Point • Transition occurs closer to distal (venous) end, thus capillaries filter more than reabsorb so more fluids enter the tissue beds than return to the blood, • Excess fluid enters interstitial space, becomes interstitial fluid (net 3.6L/day) • Eventually, fluid will enter lymphatic vessels, become lymph • Then what? Changes in Capillary Dynamics • Hemorrhaging: – reduces HPc and thus NFP – increases reabsorption of interstitial fluid (called recall of fluids) • Dehydration: – increases OPc, decreases NFP – Also accelerates reabsorption (recalls fluids) • Increase in HPc or decline in OPc : – Happens in starvation, heart failure – fluid moves out of blood – builds up in peripheral tissues (edema) Cardiovascular Regulation • Goal is to maintain adequate Tissue Perfusion, blood flow through the tissues • Carries O2 and nutrients to tissues and organs, carries CO2 and other wastes away • Is affected by: – cardiac output (HR, stroke volume) – peripheral resistance (vessel diameter) – blood volume • Blood pressure = CO x PR Cardiovascular Regulation • Changes blood flow to a specific area at an appropriate time, without changing blood flow to vital organs 3 Regulatory Mechanisms • Control of cardiac output and blood pressure: 1. Autoregulation: • causes immediate, localized homeostatic adjustments 2. Neural mechanisms: • respond quickly to changes at specific sites 3. Endocrine mechanisms: • direct long-term changes • Short-term controls counteract moment-to-moment fluctuations in blood pressure by altering peripheral resistance • Long-term controls regulate blood volume Cardiovascular Responses Figure 21-13 1. Autoregulation • Local blood flow within tissues is adjusted by peripheral resistance while cardiac output stays the same (no effect on heart) • Vasodilators: dilate precapillary sphincters – Local vasodilators: accelerate blood flow at tissue level: • • • • • • Low O2 or high CO2 levels Low pH (acids) Nitric oxide (NO) High K+ or H+ concentrations Chemicals released by inflammation (histamine) Elevated local temperature Autoregulation • Local Vasoconstrictors – e.g. prostaglandins and thromboxanes released by damaged tissues – constrict precapillary sphincters – affect a single capillary bed At high concentrations, both local vasodilators and vasoconstrictors may also affect arterioles (which would affect many capillary beds) 2. Neural Mechanisms • Cardiovascular (CV) centers: vasomotor center plus the cardiac centers of medulla oblongata that integrate blood pressure control by altering cardiac output and blood vessel diameter (adjusts cardiac output and peripheral resistance) – – – – Vasomotor center: adjust size of arterioles Cardioacceleratory center: increases cardiac output Cardioinhibitory center: reduces cardiac output All are part of sympathetic nervous system • Neural controls of peripheral resistance: – Alter blood distribution in response to demands – Maintain MAP by altering blood vessel diameter Neural: Vessels Vasomotor Center • Vasomotor center – a cluster of sympathetic neurons in the medulla that oversees changes in blood vessel diameter – Maintains blood vessel tone by innervating smooth muscles of blood vessels, especially arterioles • Vasoconstriction – controlled by adrenergic nerves (NE) – stimulates smooth muscle contraction in arteriole walls – neurons innervate peripheral blood vessels throughout body • Vasodilation: – controlled by special sympathetic nerves – relaxes smooth muscle – neurons found only in skeletal muscles and heart Vasomotor Center • Vasomotor tone: constant action of sympathetic vasoconstrictor nerves keep arterioles constricted to a point about halfway between fully dilated and fully constricted • Modest adjustments can make huge changes in peripheral resistance, and thus in arterial blood pressure • Extreme widespread sympathetic stimulation causes venoconstriction too, a narrowing of systemic veins to mobilize the venous reserve Vasomotor Control • For most peripheral tissues the sympathetic nervous system affects the state of the arterioles: at rest, sympathetic tone keeps them in the middle of their possible openness. – If BP drops, sympathetic activity increases and vasoconstriciton occurs – If too high, sympathetic activity declines and vasodilation occurs – Parasympathetic NS does not play a role Cardiovascular centers • Baroreceptors and chemoreceptors monitor arterial blood composition and pressure and signal the cardiovascular centers to change Baroreceptor Reflexes • Baroreceptor reflexes: stretch receptors in walls of the carotid sinuses, aortic sinuses, and right atrium responds to changes in blood pressure: • When blood pressure rises, increased stimulation to cardiovascular centers causes them to: – decrease cardiac output – cause peripheral vasodilation • When blood pressure falls, less stimulation to cardiovascular centers causes them to: – increase cardiac output – cause peripheral vasoconstriction Impulse traveling along afferent nerves from baroreceptors: Stimulate cardioinhibitory center (and inhibit cardioacceleratory center) Baroreceptor Reflexes Baroreceptors in carotid sinuses and aortic arch stimulated Sympathetic impulses to heart ( HR and contractility) CO Inhibit vasomotor center R Rate of vasomotor impulses allows vasodilation ( vessel diameter) Arterial blood pressure rises above normal range CO and R return blood pressure to Homeostatic range Stimulus: Rising blood pressure Homeostasis: Blood pressure in normal range Stimulus: Declining blood pressure CO and R return blood pressure to homeostatic range Peripheral resistance (R) Vasomotor fibers stimulate vasoconstriction Impulses from baroreceptors: Stimulate cardioacceleratory center (and inhibit cardioinhibitory center) Cardiac output (CO) Sympathetic impulses to heart ( HR and contractility) Arterial blood pressure falls below normal range Baroreceptors in carotid sinuses and aortic arch inhibited Stimulate vasomotor center Figure 21-14 Chemoreceptor Reflexes • Chemoreceptors in carotid bodies and aortic bodies – monitor blood for changes in pH, O2, and CO2 concentrations • Reflexes produced by coordinating cardiovascular and respiratory activities 3. Hormonal Regulation • Hormones have short-term and long-term effects on cardiovascular regulation – E and NE, hormones produced by adrenal medullae (neuroendocrine) increase BP – Antidiuretic hormone (ADH) – causes intense vasoconstriction in cases of extremely low BP – Angiotensin II – kidney release of renin generates angiotensin II, which causes vasoconstriction – Erythropoietin (EPO) increases blood volume and pressure – Natriuretic peptides (ANP, BNP) decrease blood volume and pressure Antidiuretic Hormone (ADH) • Released by posterior lobe of pituitary in response to reduced blood volume, an increase in blood oncotic pressure, or to Angoiotensin II release – Elevates blood pressure (mild vasoconstrictor) – Reduces water loss at kidneys to increase blood volume Angiotensin II • Responds to fall in renal blood pressure • Renin – angiotensin system results in its production by ACE in lung capillaries – – – – – Increases aldosterone Increases ADH Induces thirst Increases cardiac output Vasoconstritor (arterioles) • Effect on BP is 4 - 8 times greater than NE • Think about what that means for blood pressure drugs (ACE inhibitors versus Beta blockers) Erythropoietin (EPO) • Released at kidneys • Responds to low blood pressure, low O2 content • Stimulates red blood cell production ANP and BNP • Atrial natriuretic peptide (ANP): – produced by cells in right atrium • Brain natriuretic peptide (BNP): – produced by ventricular muscle cells • Respond to excessive diastolic stretching • Lower blood volume and blood pressure by: – blocking ADH, aldosterone, E and NE and stimulating peripheral vasodilation • Reduces stress on heart Hormonal Regulation Figure 21-16 CV Response to: Light Exercise • Local vasodilation (capillaries): local changes in oxygen cause release of local vasodilators • Increased venous return from increased skeletal muscle contractions and increased respiratory rate (resp. pump) • Cardiac output rises to 2 times resting levels due to increased venous return (Frank-Starling principle) and atrial reflex • A little sympathetic activation CV Response to: Heavy Exercise • General sympathetic activation • Major redistribution of blood to muscles due to dilation there and constriction everywhere else • Cardioaccelaratory centers increase HR, increase CO, so blood moves through the system more quickly Vascular pathology BIOL242 Hemorrhage • Short term problem: maintain blood pressure and flow • Long term problem: restore normal blood volume Responses to Blood Loss Figure 21-17 Short-Term Responses to Hemorrhage • To prevent drop in blood pressure baroreceptor reflexes: – increase cardiac output (increasing heart rate) – cause peripheral vasoconstriction • Sympathetic nervous system: – further vasoconstriciton constricts arterioles – venoconstriction improves venous return if necessary • Hormonal effects: – increase cardiac output – increase peripheral vasoconstriction (E, NE, ADH, angiotensin II) • Kidneys filter less, make less urine Long-Term Responses to Hemorrhage • Restoration of blood volume can take several days: 1. Recall of fluids from interstitial spaces (caused by decline in CHP) 2. Aldosterone and ADH promote fluid retention and reabsorption 3. Thirst increases, replaces “borrowed” fluid 4. Erythropoietin stimulates red blood cell production Kidney and blood pressure Shock • Short-term responses compensate up to 20% loss of blood volume • Failure to restore blood pressure results in circulatory shock • Certain after 30 – 35% blood loss Circulatory collapse • When arterioles and precapillary sphincters can no longer vasoconstrict despite the vasomotor stimulation to elevate blood pressure • Widespread peripheral vasodilation • Leads to fatal decline in BP • This is the endpoint of all types of shock if untreated Newborn Heart • Before Birth – Fetal lungs are collapsed – O2 provided by placental circulation • At Birth – Newborn breathes air – Lungs expand – Pulmonary circulation provides O2 The Neonatal Heart Figure 21-33b Cardiovascular Changes at Birth • • • Pulmonary vessels expand Reduced resistance allows blood flow to pulmonry circuit Rising O2 causes ductus arteriosus constriction • short vessel that connects pulmonary and aortic trunks in fetus • Rising left atrium pressure closes foramen ovale Congenital Cardiovascular Problems Figure 21-34 Congenital Cardiovascular Problems • PFO – Left to right shunt • Patent ductus arteriosus – right to left shunt, can lead to cyanosis • Ventricular septal defects (common) – causes mixing of ventricular blood similar to PFO • Tetralogy of Fallot – narrow pulmonary trunk, incomplete IV septum, aorta originates in middle of defective septum, RV is enlarged • Transposition of great vessels Arteriosclerosis • Thickening of arterial walls, leads to coronary artery disease (CAD), peripheral artery disease, and stroke – Calcification: t. media smooth muscle replaced by calcium – Atherosclerosis: lipid deposits form in t. media • High levels of lipids in blood lead to phagocytosis of lipid particles plaques clot formation • Common in familial hypercholesterolemia • How do plaques increase vascular resistance (and thus afterload) in in two ways? Antihypertensive medications • Calcium channel blockers – negative inotropic effect, may slow conduction • Beta blockers – blocks sympathetic effects on heart, vessels • Diuretics – lower blood volume • Vasodilators – lower BP • ACE inhibitors Edema • Tissue swelling • Caused by disruptions in balance of hydrostatic and oncotic forces • Capillary damage: OPif increases as plasma proteins leak out, reduces reabsorption swelling at injury site • Starvation: decreased plasma protein synthesis, reduced OPc, edema in abdominopelvic cavity (ascites) • Most common in US: increase in HPc due to high afterload (CHF, atherosclerosis, etc.) Vessels Vessels - Generalities • Peripheral distributions are the same on the left and right side of the body except near the heart. • Most arteries and veins follow similar paths and are often similarly named • One vessel can have several names (like a street) • Many tissues are serviced by several arteries and veins Veins - Generalities • Veins are far more variable from person to person than arteries • Several veins, especially in the limbs, have superficial and deep routes. Superficial route usually only caries 10 15% of blood at a maximum and serves to aid in thermoregulation Vessels to know • Be able to identify the following arteries/veins on a model: inferior and superior vena cava, left and right pulmonary arteries and veins, common carotid, subclavian, brachiocephalic, coronary • thoracic and abdominal aorta, celiac, renal, axillary, brachial, radial, ulnar, mesenteric, iliac, peroneal, femoral, popliteal, tibial, jugular, celiac, splenic, gastric, hepatic and saphenous. Major Systemic Arteries Figure 21-20 Branches of the Aortic Arch • Deliver blood to head and neck: – brachiocephalic trunk • right subclavian artery • right common carotid artery – left common carotid artery – left subclavian artery Arteries of Upper Limbs Subclavian axial brachial splits into radial, ulnar 3D Peel Away Descending aorta thoracic aorta abdominal aorta common iliac to be continued renal 3 Unpaired Branches of the Abdominal Aorta • Celiac trunk, divides into: – left gastric artery – splenic artery – common hepatic artery • Superior mesenteric artery • Left mesenteric artery celiac hepatic gastric splenic mesenteric iliac Iliac femoral popliteal Posterior and anterior tibial. Posteror tibial gives rise to peroneal (fibular) Veins • Know the veins with the same names as arteries • Exceptions: – saphenous (leg) no comparable artery – jugular (neck) like carotid arteries