Document 15686220
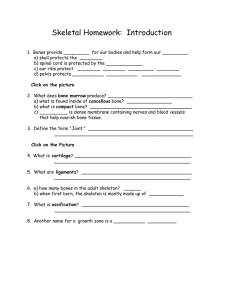
advertisement

http://images5.fanpop.com/image/photos/26500000/-skeleton-dance-skeletons-26529088-725-544.png Skeletal Cartilages • Contain no blood vessels or nerves • Perichondrium (dense irregular connective tissue girdle) contains blood vessels for nutrient delivery to cartilage • Types – Hyaline – Elastic – Fibrocartilage Cartilage in external ear Cartilage in Intervertebral disc Cartilages in nose Articular Cartilage of a joint Epiglottis Thyroid cartilage Cricoid cartilage Larynx Trachea Lung Costal cartilage Respiratory tube cartilages in neck and thorax Pubic symphysis Meniscus (padlike cartilage in knee joint) Articular cartilage of a joint Bones of skeleton Axial skeleton Appendicular skeleton Cartilages Hyaline cartilages Elastic cartilages Fibrocartilages Figure 6.1 Growth of Cartilage • Appositional – Cells secrete matrix against the external face of existing cartilage • Interstitial – Chondrocytes divide and secrete new matrix, expanding cartilage from within http://www.vetmed.vt.edu/education/curriculum /vm8054/labs/Lab7/IMAGES/elastic%20cartilage% 20WITH%20LABEL%20copy.jpg Cartilage in external ear Cartilage in Intervertebral disc Cartilages in nose Articular Cartilage of a joint Bones of the Skeleton Costal cartilage Pubic symphysis Meniscus (padlike cartilage in knee joint) Articular cartilage of a joint Figure 6.1 Classification of Bones by Shape • Long bones • Short bones • Flat bones • Irregular bones Functions of Bones • • • • Support Protection Movement Mineral & Growth Factor Storage • Blood cell formation • Triglyceride storage • Hormone Production Bone Structure • Bones are organs! – Multiple tissue types • Bone (osseous) tissue, nervous tissue, cartilage, fibrous connective tissue, muscle and epithelial cells (in its blood vessels) Bone Texture • Compact – Dense outer layer; smooth and solid • Spongy (trabecular) – Honeycomb of flat pieces of bone (trabeculae) deep to compact – Space b/w trabeculae filled with red or yellow bone marrow Structure of Short, Irregular, and Flat Bones • Periosteum covered compact bone on the outside • Endosteum covered spongy bone within – diploë • Bone marrow b/w the trabeculae • Hyaline cartilage on articular surfaces Structure of Typical Long Bone • Diaphysis – Tubular shaft forms long axis – Compact bone surrounds medullary cavity • Epiphyses (bone ends) – Compact bone outside; spongy bone inside – Articular cartilage covers articular surfaces • Epiphyseal line – b/w diaphysis and epiphysis – Remnant of epiphyseal plate Membranes of Bone • Periosteum – Outer fibrous layer – Inner osteogenic layer – Contains nerve fibers, nutrient blood vessels, and lymphatic vessels that enter the bone via nutrient foramina – Secured to underlying bone by Sharpey’s fibers Membranes of Bone • Endosteum – Delicate membrane on internal surfaces of bone – Contains osteogenic cells Hematopoietic Tissue (Red Marrow) • Infants (long bones) – Medullary cavities and spongy bone • Adults (long bones) – Little red marrow • Red marrow in flat and some irregular bones is most active http://www.gla.ac.uk/ibls/US/fab/images/generic/bocompac.jpg Bone Markings • Projections, depressions, and holes – Sites of attachment for muscles, ligaments, and tendons – Joint surfaces – Passageways for blood vessels and nerves Bone Markings: Projections • Sites of muscle and ligament attachment – Tuberosity – Crest – Trochanter – Line – Tubercle – Epicondyle – Spine – Process • Projections that help to form joints – Head – Facet – Condyle – Ramus Bone Markings: Depressions and Openings • Passages for blood vessels and nerves – Meatus – Sinus – Fossa – Groove – Fissure – Foramen Microscopic Anatomy of Bone Microscopic Anatomy of Bone: Compact Bone • Haversian system (or osteon) – Lamellae – Central (Haversian) canal Microscopic Anatomy of Bone: Compact Bone • Perforating (Volkmann’s) canals • Lacunae • Canaliculi Microscopic Anatomy of Bone: Spongy Bone • Trabeculae – Align along lines of stress – No osteons – Irregularly arranged lamellae, osteocytes, and canaliculi – Capillaries in endosteum supply nutrients Chemical Composition of Bone • Organic – Bone cells – Osteoid—organic bone matrix secreted by osteoblasts • Ground substance, collagen fibers • Inorganic – Hydroxyapatites (mineral salts) • 65% of bone by mass • Mainly calcium phosphate crystals Bone Development • Ossification (osteogenesis): process of bone tissue formation – Formation of bony skeleton • Begins in 2nd month of development – Postnatal bone growth • Until early adulthood – Bone remodeling and repair • Lifelong Types of Ossification • Endochondral ossification – Bone forms by replacing hyaline cartilage – Majority of skeleton • Intramembranous ossification – Bone develops from fibrous membrane – Bones called membrane bones – Forms flat bones, e.g. clavicles and cranial bones Endochondral Ossification • Forms most all bones inferior to base of skull (except clavicles) • Begins late in 2nd month of development • Uses hyaline cartilage models • Hyaline cartilage must be broken down before ossification Month 3 Week 9 Birth Childhood to adolescence Articular cartilage Secondary ossification center Epiphyseal blood vessel Area of deteriorating cartilage matrix Hyaline cartilage 1 2 Epiphyseal plate cartilage Medullary cavity Spongy bone formation Bone collar Primary ossification center Spongy bone Blood vessel of periosteal bud 3 4 5 Figure 6.9 Intramembranous Ossification • Forms cranial bones of the skull and clavicles • Begins within fibrous connective tissue membranes formed by mesenchymal cells • Ossification centers appear • Osteoid is secreted • Woven bone and periosteum form • Lamellar bone replaces woven bone & red marrow appears Osteoblast Mesenchymal cell Osteoid Collagen fibril Ossification center Osteocyte Newly calcified bone matrix Osteoid Osteoblast 1 Ossification centers appear in the fibrous connective tissue membrane. 2 Osteoid is secreted within the fibrous membrane and calcifies. Fibrous periosteum Mesenchyme condensing to form the periosteum Osteoblast Plate of compact bone Trabeculae of woven bone Blood vessel 3 Woven bone and periosteum form. Diploë (spongy bone) cavities contain red marrow 4 Lamellar bone replaces woven bone, just deep to the periosteum. Red marrow appears. Figure 6.9 Intramembranous ossification. Postnatal Bone Growth • Interstitial growth: – length of long bones • Appositional growth: – thickness and remodeling of all bones by osteoblasts and osteoclasts on bone surfaces Interstitial (Longitudinal) Growth • Epiphyseal plate cartilage organizes into 5 important functional zones: – Resting (quiescent) zone – Proliferation (growth) – Hypertrophic – Calcification – Ossification (osteogenic) Resting zone Proliferation zone Cartilage cells undergo mitosis. 1 Hypertrophic zone Older cartilage cells enlarge. 2 Calcified cartilage spicule Osteoblast depositing bone matrix Osseous tissue (bone) covering cartilage spicules Calcification zone Matrix becomes calcified; cartilage cells die; matrix begins deteriorating. 3 4 Ossification zone New bone formation is occurring. Figure 6.10 Appositional Growth • Growth in Width – Osteoblasts active in periosteum – Osteoclasts active in the endosteum – Building > Breaking down = thicker stronger bone Bone growth Cartilage grows here. Bone remodeling Articular cartilage Epiphyseal plate Cartilage is replaced by bone here. Cartilage grows here. Cartilage is replaced by bone here. Bone is resorbed here. Bone is added by appositional growth here. Bone is resorbed here. Figure 6.11 Hormonal Regulation of Bone Growth • Growth hormone • Thyroid hormone • Testosterone and Estrogen http://2.bp.blogspot.com/-FrC7iCwLqDk/Tb8hrWvYXnI/AAAAAAAAOOg/il4zBWZI5Q/s1600/2008_01_17_pb%252520kids%252520growth.jpg Bone Remodeling • Bone is constantly being “recycled” • Occurs @ surface of periosteum and endosteum • Deposit – Injury or needed strength, requires good diet – Osteoid seam and Calcification front • Resorption – Osteoclasts secrete: lysosomal enzymes, acids – Dissolved matrix is transcytosed Control of Remodeling • What controls continual remodeling of bone? – Hormonal mechanisms that maintain calcium homeostasis in the blood – Mechanical and gravitational forces http://tutor4physics.com/workliftbox.gif Hormonal Control of Blood Ca2+ • Most calcium in the body is in the bones • Less that 1.5g in blood – tightly regulated narrow range • Calcium is necessary for – Transmission of nerve impulses – Muscle contraction – Blood coagulation – Secretion by glands and nerve cells – Cell division Calcium homeostasis of blood: 9–11 mg/100 ml BALANCE BALANCE Stimulus Falling blood Ca2+ levels Thyroid gland Osteoclasts degrade bone matrix and release Ca2+ into blood. Parathyroid glands PTH Parathyroid glands release parathyroid hormone (PTH). Figure 6.12 Hormonal Control of Blood Ca2+ • May be affected to a lesser extent by calcitonin Blood Ca2+ levels Parafollicular cells of thyroid release calcitonin Osteoblasts deposit calcium salts Blood Ca2+ levels Response to Mechanical Stress • Wolff’s law: A bone grows or remodels in response to forces or demands placed upon it Hormones and Mechanical Stress • Hormones – – when remodeling occurs – As a response to what??? • Mechanical Stress – Where the remodeling occurs Classification of Bone Fractures • Bone fractures may be classified by four “either/or” classifications 1. Position of bone ends after fracture: • Nondisplaced or Displaced 2. Completeness of the break • Complete or Incomplete 3. Orientation of the break to the long axis of the bone: • Linear or transverse 4. Whether or not the bone ends penetrate the skin • Compound (open) or Simple (closed) Common Types of Fractures • In addition to the previous classification, all fractures can be described in terms of – Location – External appearance – Nature of the break http://www.schultzlegalgroup.com/images/Bone-FractureInjury-Lawyer.jpg Table 6.2 Table 6.2 Table 6.2 Fracture Healing 1. Hematoma forms 2. Fibrocartilaginous callus forms Fracture Healing 3. Bony callus formation 4. Bone remodeling Homeostatic Imbalances • Osteomalacia and Rickets – Calcium salts not deposited – Rickets (childhood disease) causes bowed legs and other bone deformities – Cause: vitamin D deficiency or insufficient dietary calcium http://upload.wikimedia.org/wikipedia/commons/thumb/a/a9/Xray RicketsLegssmall.jpg/230px-XrayRicketsLegssmall.jpg Homeostatic Imbalances • Osteoporosis – Loss of bone mass – Spongy bone of spine and neck of femur become most susceptible to fracture – Risk factors • Lack of estrogen, calcium or vitamin D; petite body form; immobility; low levels of TSH; diabetes mellitus; smoking Developmental Aspects of Bones • Embryonic skeleton ossifies predictably so fetal age easily determined from X rays or sonograms • At birth, most long bones are well ossified (except epiphyses) Developmental Aspects of Bones • Nearly all bones completely ossified by age 25 • Bone mass decreases with age beginning in 4th decade • Rate of loss determined by genetics and environmental factors • In old age, bone resorption predominates