• Blood Vessel Anatomy Arteries and arterioles

Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure
Blood Vessels: The Vascular System
Arterial system Venous system
Large veins
(capacitance vessels)
Heart
Elastic arteries
(conducting vessels)
Small veins
(capacitance vessels)
Large lymphatic vessels
Lymph node
Lymphatic system
Arteriovenous anastomosis
Muscular arteries
(distributing vessels)
Postcapillary venule
Thoroughfare channel
Sinusoid
Lymphatic capillary
Arterioles
(resistance vessels)
Terminal arteriole
Metarteriole
Capillaries
Precapillary sphincter
(exchange vessels)
Figure 19.2
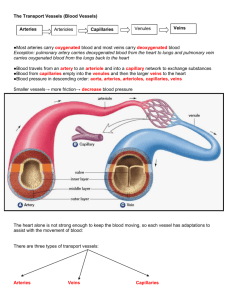
Layers of Blood Vessels
Tunica intima
• Endothelium
• Subendothelial layer
Internal elastic lamina
Tunica media
( smooth muscle under control of symp. n.s. and elastic fibers)
External elastic lamina
Tunica externa
( fibrous connective: collagen fibers)
(b)
Lumen
Artery
Valve
Capillary
Capillary network
Lumen
Vein
Basement membrane
Endothelial cells
Figure 19.1b
Differences Between Blood Vessel Types
Walls of arteries are the thickest, while lumen is smaller in diameter
Walls of veins are thinner, while lumens of veins are larger
Walls of capillaries are only one cell layer thick to allow for exchanges between blood and tissue
Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure
Arteries, Compared
Elastic Arteries
Large thick-walled arteries with elastin in all three tunics
Aorta and its major branches
Large lumen offers low-resistance
Act as pressure reservoirs—expand and recoil as blood is ejected from the heart
Muscular Arteries
Distal to elastic arteries; deliver blood to body organs
Have thick tunica media with more smooth muscle
Active in vasoconstriction
Arterioles
Smallest arteries
Lead to capillary beds
Control flow into capillary beds via vasodilation and vasoconstriction
Table 19.1 (1 of 2)
Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure
Capillaries and Capillary Beds
Arterial system Venous system
Large veins
(capacitance vessels)
Heart
Elastic arteries
(conducting vessels)
Small veins
(capacitance vessels)
Large lymphatic vessels
Lymph node
Lymphatic system
Arteriovenous anastomosis
Muscular arteries
(distributing vessels)
Postcapillary venule
Thoroughfare channel
Sinusoid
Lymphatic capillary
Arterioles
(resistance vessels)
Terminal arteriole
Metarteriole
Capillaries
Precapillary sphincter
(exchange vessels) Figure 19.2
Capillaries
Found in all tissues except for cartilage, epithelia, cornea and lens of eye
Three structural types
1.
Continuous capillaries
2.
Fenestrated capillaries
3.
Sinusoidal capillaries (sinusoids)
Continuous Capillaries
Abundant in the
skin and muscles
•
Tight junctions connect endothelial cells
•
Intercellular clefts allow the passage of fluids and small solutes
Continuous capillaries of the brain
•
Tight junctions are complete, forming the blood-brain barrier
Pericyte
Red blood cell in lumen
Intercellular cleft
Endothelial cell
Basement membrane
Tight junction
Endothelial nucleus
Pinocytotic vesicles
(a) Continuous capillary.
Least permeable, and most common (e.g., skin, muscle).
Figure 19.3a
Fenestrated Capillaries
Some endothelial cells contain pores
(fenestrations)
More permeable than continuous capillaries
Function in absorption or filtrate formation
(
small intestines, endocrine glands, and kidneys
)
Pinocytotic vesicles
Red blood cell in lumen
Fenestrations
(pores)
Endothelial nucleus
Basement membrane
Intercellular cleft
Tight junction Endothelial cell
(b) Fenestrated capillary.
Large fenestrations
(pores) increase permeability. Occurs in special locations (e.g., kidney, small intestine).
Figure 19.3b
Sinusoidal Capillaries
Fewer tight junctions, larger intercellular clefts, large lumens
Usually fenestrated
Allow large molecules and blood cells to pass between the blood and surrounding tissues
Found in the
liver, bone marrow, spleen
Endothelial cell
Red blood cell in lumen
Large intercellular cleft
Tight junction
Incomplete basement membrane
Nucleus of endothelial cell
(c) Sinusoidal capillary.
Most permeable. Occurs in special locations (e.g., liver, bone marrow, spleen).
Figure 19.3c
Capillary Beds
Interwoven networks of capillaries form the microcirculation between arterioles and venules
Consist of two types of vessels
1.
Vascular shunt (metarteriole—thoroughfare channel): o Directly connects the terminal arteriole and a postcapillary venule
2.
True capillaries o 10 to 100 exchange vessels per capillary bed o Branch off the metarteriole or terminal arteriole
Blood Flow Through Capillary Beds
Precapillary sphincters
Metarteriole
Vascular shunt
Thoroughfare channel
Terminal arteriole
True capillaries
Postcapillary venule
(a) Sphincters open —blood flows through true capillaries.
Low O
2
CO
2
, high
, high pH, low nutrients, hot external temperatures, relaxation
Terminal arteriole Postcapillary venule
(b) Sphincters closed —blood flows through metarteriole thoroughfare channel and bypasses true capillaries.
High O
2
, low pH, nutrients, low CO
2
, cold external temperatures, fight or flight conditions
Figure 19.4
Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure
Venules and Veins
Venules
Formed when capillary beds unite
Very porous; allow fluids and WBCs into tissues
Postcapillary venules consist of endothelium and a few pericytes
Larger venules have one or two layers of smooth muscle cells
Veins
Formed when venules converge
Have thinner walls, larger lumens compared with corresponding arteries
Blood pressure is lower than in arteries
Thin tunica media and a thick tunica externa consisting of collagen fibers and elastic networks
Called capacitance vessels (blood reservoirs); contain up to 65% of the blood supply
Table 19.1 (2 of 2)
Veins
Adaptations that ensure return of blood to the heart
1.
Large-diameter lumens offer little resistance
2.
Valves prevent backflow of blood o Most abundant in veins of the limbs
Venous sinuses: flattened veins with extremely thin walls (e.g., coronary sinus of the heart and dural sinuses of the brain)
One-way valves in veins prevent backflow where positive pressure is at a mininum
Most of the Blood is in Veins and Venules
Pulmonary blood
Systemic arteries and arterioles 15% vessels 12%
Heart 8%
Capillaries 5%
Systemic veins and venules 60%
Figure 19.5
Vascular Anastomoses
Interconnections of blood vessels
Arterial anastomoses provide alternate pathways (collateral channels) to a given body region
• Common at joints, in abdominal organs, brain, and heart
Vascular shunts of capillaries are examples of arteriovenous anastomoses
Venous anastomoses are common
Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure
Pulse
Pulse – pressure wave of blood
Monitored at
“pressure points” where pulse is easily palpated
Figure 11.16
Physiology of Circulation: Definition of Terms
Blood flow
• Volume of blood flowing through a vessel, an organ, or the entire circulation in a given period, measured in ml/min
Blood pressure (BP)
• Force per unit area exerted on the wall of a blood vessel by the blood, expressed in mm Hg
•
Measured as systemic arterial BP in large arteries near heart
Peripheral Resistance
• Opposition to flow; a measure of the amount of friction blood encounters
•
Generally encountered in the peripheral systemic circulation
•
Three important sources of resistance o Blood viscosity (relatively constant) o Total blood vessel length (relatively constant) o Blood vessel diameter (Resist. varies inversely with the fourth power of vessel radius (e.g., if the radius is doubled, the resistance is 1/16 as much)
Local Blood Pressures
Systemic pressure
•
Highest in the aorta, declines throughout the pathway; 0 mm Hg in the right atrium
Arterial pressure
Reflects two factors of the arteries close to the heart
• Elasticity (compliance or distensibility)
•
Volume of blood forced into them at any time
Blood pressure near the heart is pulsatile o Systolic pressure: pressure exerted during ventricular contraction o Diastolic pressure: lowest level of arterial pressure o Pulse pressure = difference between systolic and diastolic pressure
Mean arterial pressure (MAP): pressure that propels the blood to the tissues
MAP = diastolic pressure + 1/3 pulse pressure
Pulse pressure and MAP both decline with increasing distance from the heart
Capillary blood pressure
Low capillary pressure is desirable; low pressure forces filtrate into interstitial spaces
Venus blood pressure - near zero
Comparison of Blood Pressures
Blood pressure results when flow is opposed by resistance
Disease causing blood pressure change
Arteriosclerosis:
Hardening of the artery walls and decrease of elasticity, restricting flow and increasing blood pressure.
Atherosclerosis : A specific type of arterosclerosis where arteries are clogged by an accumulation of plaques: cholesterol particles (lipoproteins), fat, calcium, cellular waste and other substances.
Factors Aiding Venous Return
1.
Respiratory “pump”: pressure changes created during breathing move blood toward the heart by squeezing abdominal veins as thoracic veins expand
2.
Muscular “pump”: contraction of skeletal muscles “milk” blood toward the heart and valves prevent backflow
3.
Vasoconstriction of veins under sympathetic control
Measuring Arterial Blood Pressure
Measurements by health professionals are made on the pressure in large arteries
•
Systolic – pressure at the peak of ventricular contraction
•
Diastolic – pressure when ventricles relax
Pressure in blood vessels decreases as the distance away from the heart increases
Listen for the sounds of Kortokoff
Normal BP is 120/75-80 Blood pressure animation online
Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure
Variations in Blood Pressure
Human normal range is variable
• Normal o 110-140 mm Hg systolic or just 120/70 o 70-80 mm Hg diastolic
•
Hypotension o Low systolic (below 110 mm HG) o Often associated with illness or physical conditioning
•
Hypertension o High systolic (above 140 mm HG) o Can be dangerous if it is chronic o Caused by many things, including a high saturated fat and/or salty diet, little exercise, & chronic stress
Cardio System II: Vasculature and Pressure
Blood Vessel Anatomy
•
Arteries and arterioles
•
Capillaries (3 types)
•
Veins and venules
Pulse and Pressure Points
Blood Pressure
•
Factors Regulating
Blood Pressure