Overview of the Reproductive System Parts of the Male Reproductive System
advertisement

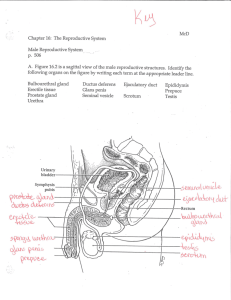
Male Reproductive Anatomy and Physiology Overview of the Reproductive System Parts of the Male Reproductive System Testes and Epididymis Ductus Deferens and Urethra Accessory Glands External Genitalia Spermatogenesis and Mature Sperm Testosterone Production The Reproductive System Gonads – primary sex organs • Testes in males • Ovaries in females Gonads produce gametes (sex cells) and secrete hormones • Sperm – male gametes • Ova (eggs) – female gametes Male Reproductive System Testes Duct system • Epididymis • Ductus deferens • Urethra Accessory organs • Seminal vesicle • Prostate gland • Bulbourethral gland External genitalia • Penis • Scrotum Coverings of the Testes Coverings of the testes (internal to the scrotum) • Tunica vaginalis o Serous membrane derived from peritoneum; parietal and visceral layers • Tunica albuginea – capsule that surrounds each testis • Septa – extensions of the capsule that extend into the testis and divide it into lobules Tunica vaginalis Testes Each lobule contains one to four seminiferous tubules • Tightly coiled structures • Function as spermforming factories • Empty sperm into the rete testis Sperm travels through the rete testis to the epididymis Sertoli (sustenacular) cells provide nourishment for developing sperm and protect them from the body’s immune system by housing them inside their membranes. Interstitial (Leydig) cells produce androgens such as testosterone Cross section of seminiferous tubule Figure 16.1 Epididymis Comma-shaped, tightly coiled tube Found on the superior part of the testis and along the posterior lateral side Functions to mature and store sperm cells (at least 20 days) Sperm become motile during their stay in the epididymis Expels sperm with the contraction of muscles in the epididymis walls to the vas deferens Ductus Deferens, Ejaculatory Duct, Urethra Ductus (Vas) Deferens • Carries sperm from the epididymis to the ejaculatory duct • Passes through the inguinal canal and over the bladder • Moves sperm by peristalsis • Coated with microvilli-like stereocilia that reabsorb some of the fluid produced with the sperm • Spermatic cord – ductus deferens, blood vessels, and nerves in a connective tissue sheath • Ends in the ejaculatory duct which unites with the urethra Vasectomy – cutting of the ductus deferens on both sides, at the level of the testes, to prevent transportation of sperm. Sperm are reabsorbed. Seminal Vesicles: Energy Source for Sperm Located at the base of the bladder Produces a thick, yellowish secretion (60% of semen) • Fructose (sugar) • Vitamin C • Prostaglandins • Other substances that nourish and activate sperm Prostate Gland Encircles the upper part of the urethra Secretes a milky fluid • Helps to activate sperm • Alkaline fluid added to neutralize vaginal secretions. • Adds ~ 30% of total semen fluid • Enters the urethra through several small ducts • Easily palpated through rectum (check for cancer); important in men over 50. Bulbourethral (Cowper's) Glands Pea-sized gland inferior to the prostate Produces a thick, clear mucus • Cleanses the urethra of acidic urine • Adds a lubricant for sperm during ejaculation • Secreted into the penile urethra Male Urethra Urethra • Extends from the base of the urinary bladder to the tip of the penis • Carries both urine and sperm • Sperm enters from the ejaculatory duct Regions of the urethra • Prostatic urethra – surrounded by prostate • Membranous urethra – from prostatic urethra to penis • Spongy (penile) urethra – runs the length of the penis External Genitalia Scrotum • Divided sac of skin outside the abdomen • Maintains testes at 3°C lower than normal body temperature to protect sperm viability Penis • Delivers sperm into the female reproductive tract • Regions of the penis o Shaft o Glans penis (enlarged tip) o Prepuce (foreskin) Folded cuff of skin around proximal end Often removed by circumcision Semen Composition and Analysis Mixture of sperm and accessory gland secretions Advantages of accessory gland secretions • Fructose from prostate provides energy for sperm cells • Alkalinity of semen (from seminal vesicles) helps neutralize the acidic environment of vagina • Semen inhibits bacterial multiplication • Elements of semen enhance sperm motility Source Volume Characteristics Urethral and bulbourethral glands 0.1-0.2cc Viscous, clear Testes, epididymides,vas a deferentia 0.1-0.2cc Sperm present Prostate 0.5-1.0cc Acidic,watery Seminal vesicles 1.0-3.0cc Gelatinous, fructose positive Complete ejaculate 2.0-5.0cc Liquefies in 2025min Parameters of Normal, Fertile Semen VOLUME >2.0 ML pH 7.2-7.8 CONCENTRATION >20x106/ML MOTILITY >50% MORPHOLOGY >30% NORMAL MORPHOLOGY WBC < 1x106/ML Regulation of Male Androgens (Sex Hormones) Acts directly on spermatogonia Acts on Interstitial cells, called Interstitial Cell Stimulating Hormone Figure 16.6 Spermiogenesis (64-72 days) Lumen Inhibin GnRH - + testosterone + testosterone Maturation sequence + LH (ICSH) GnRH Lumen FSH Testosterone Testosterone Production • The most important hormone of the testes • Produced in interstitial cells Functions of testosterone • Stimulates reproductive organ development • Facilitates spermatogenesis and promotes the maturation of sperm • Influences sexual desire and related behaviours • Causes secondary sex characteristics o Deepening of voice o Increased hair growth o Enlargement of skeletal muscles o Thickening of bones Anatomy of a Mature Sperm Cell Acrosome Reaction (in sea urchins) Acrosomal enzymes of many sperm digesting follicle cells around ovum Diseases and Conditions of the Male Reproductive System Cryptorchidism (undescended testicle) • Phimosis • External urethral meatus is below the tip Variocele • Fluid-filled sac surrounding the testes Hypospadias (literally “below the fleshy spike”) • Penis cannot be extruded from the prepuce (foreskin) Hydrocele • Can lead to sterility and testicular cancer Dialated and twisted veins of the testes, causes swelling Orchitis and Epididymitis • Infections of the testicles and epididymus; may lead to sterility Cancer (penile, prostate, testicular) Balanitis • Inflammation of the foreskin and head of penis due to • infection (old reason for circumcision) Priapism • Constant state of erection due to neurological defect or damage Peyronie’s Disease • Hard lump forms on the penis in erectile tissue layers MALE REPRODUCTIVE SYSTEM OVERVIEW ANIMATION Reproduction II - Female Anatomy and Physiology Structures of the Female Reproductive System • Ovaries • Fallopian Tubes • Uterus and Vagina • External Genitalia Oogenesis Menstrual Cycle Female Sex Hormones Mammary Glands Overview of Female Reproductive System Ovaries Duct System • Uterine tubes (fallopian tubes) • Uterus • Vagina External genitalia Ovaries Composed of ovarian follicles (sac-like structures) Structure of an ovarian follicle • Oocyte • Follicular cells Primary follicle – contains an immature oocyte. All primary oocytes formed by birth, suspended in Prophase I. Graafian (vesicular) follicle – growing follicle with a maturing oocyte and an antrum Ovulation – when the egg is mature the follicle ruptures • Occurs about every 28 days The ruptured follicle is transformed into a corpus luteum Support for Ovaries Support Structures • Suspensory ligaments – secure ovary to lateral walls of the pelvis • Ovarian ligaments – attach to uterus • Broad ligament – a fold of the peritoneum, encloses suspensory ligament Uterine (Fallopian) Tubes/Oviducts Features of the Oviducts • Receive the ovulated oocyte • Provide a site for fertilization • Attaches to the uterus • Does not physically attach to the ovary • Supported by the broad ligament Functionality • Fimbriae – finger-like projections at the distal end that receive the oocyte • Cilia inside the uterine tube slowly move the oocyte towards the uterus (takes 3–4 days) • Fertilization occurs inside the uterine tube Uterus Features • Located between the urinary bladder and rectum • Hollow organ Functions of the uterus • Receives a fertilized egg • Retains the fertilized egg • Nourishes the fertilized egg Landmarks • Body – main portion • Fundus – area where uterine tube enters • Cervix – narrow outlet that protrudes into the vagina Uterine Walls • Endometrium o Inner layer o Allows for implantation of a fertilized egg o Sloughs off if no pregnancy occurs (menses) • Myometrium – middle layer of smooth muscle • Serous layer – outer visceral peritoneum (perimetrium) Vagina Vagina extends from cervix to exterior of body Behind bladder and in front of rectum Serves as the birth canal Receives the penis during sexual intercourse Hymen – partially closes the exit of the vagina until it is ruptured Various forms taken by the normal hymen External Genitalia Mons pubis • Fatty area overlying the pubic symphysis • Covered with pubic hair after puberty Labia – skin folds • Labia majora • Labia minora (hairless, pink) Vestibule • Area enclosed by labia majora • Contains opening of the urethra and the greater vestibular glands (produce mucus) Clitoris • Contains erectile tissue • Corresponds to the male penis Oogenesis Steps of Oogenesis • Oocytes are matured in developing ovarian follicles • Oogonia – female stem cells found in developing fetus, divide mitotically-> 1o oocytes • Primary oocytes are surrounded by cells that form primary follicles in the ovary • Oogonia no longer exist by the time of birth • Primary oocytes are inactive until puberty • Follicle stimulating hormone (FSH) causes some primary follicles to mature o Meiosis starts inside maturing follicle producing a secondary oocyte and the first polar body o Meiosis is completed after ovulation only if sperm penetrates and two additional polar bodies are produced Ovarian and Menstrual (Uterine) Cycle Cyclic changes of the endometrium Regulated by cyclic production of estrogens and progesterone Stages of the menstrual cycle • Menstrual stage – functional layer of the endometrium is sloughed when progesterone levels fall (corpus luteum degenerates) • Proliferative stage – buidling functional endometrial layer coordinated with follicular maturation, (stimulated by follicles producing estrogen) o • Ovulation occurs in this phase, estrogen levels fall as progesterone levels rise Secretory stage – endometrium increases in size and readies for implantation, maintained by progesterone from corpus luteum Hormone Production by the Ovaries Estrogens • Produced by follicle cells • Cause secondary sex characteristics o Enlargement of accessory organs o Development of breasts o Appearance of pubic hair o Increase in fat beneath the skin o Widening and lightening of the pelvis o Onset of menses Progesterone • Produced by the corpus luteum • Production continues until LH diminishes in the blood • Helps maintain pregnancy, endometrial lining FEMALE REPRODUCTIVE SYSTEM OVERVIEW ANIMATION Mammary Glands Features • Present in both sexes, but only function in females o Modified sweat glands • Function is to produce milk • Stimulated by sex hormones (mostly estrogens) to increase in size Anatomy • Areola – central pigmented area • Nipple – protruding central area of areola • Lobules – internal structures that radiate around nipple • Alveolar glands – clusters of milk producing glands within lobules • Lactiferous ducts – connect alveolar glands to nipple Reproduction II - Female Anatomy and Physiology Structures of the Female Reproductive System • Ovaries • Fallopian Tubes • Uterus and Vagina • External Genitalia Oogenesis Menstrual Cycle Female Sex Hormones Mammary Glands