Host-Pathogen Interactions
advertisement
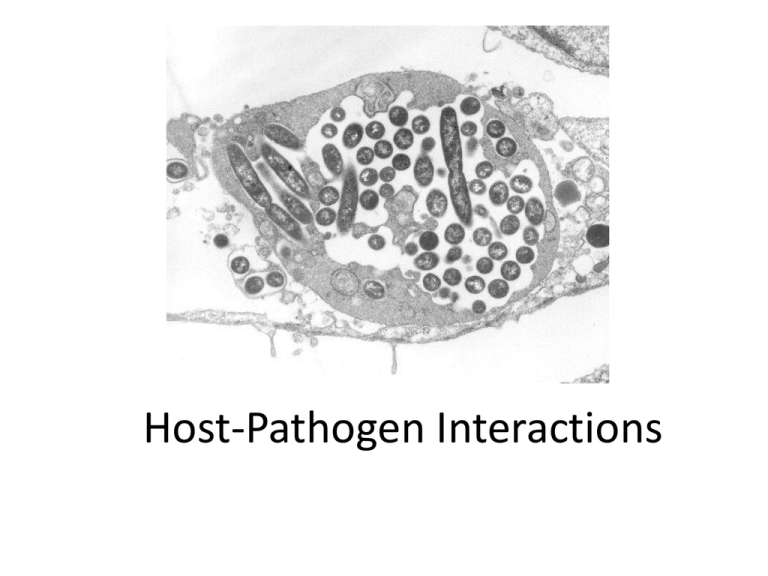
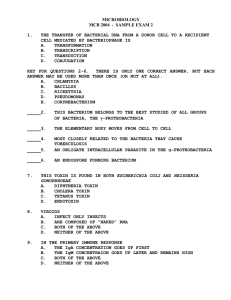
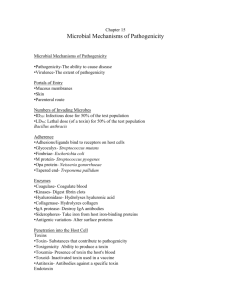
Host-Pathogen Interactions Symbiosis • Commensual • Mutualistic • Parasitic Normal microbiota • DYNAMIC! • Resident vs transient • Protective functions: – Block attachment – Consume nutrients – Produce antibiotics Normal microbiota • Other beneficial functions? – Digestion and absorption of nutrients – Production of vitamins and fatty acids – Stimulation and regulation of the immune system Normal microbiota • Can also become opportunistic pathogens – Injury to normal mucosal or skin surfaces – Antibiotic use Colonization • 2 possible outcomes: – Symbiosis – commensual or mutualistic – Infection = parasitic symbiosis • Infection: – Subclinical vs infectious disease – Primary vs secondary infection – Opportunist vs primary pathogen What determines outcome of infection? • • • • Host defenses Predisposing infection Pathogenicity Infectious dose Establishing infection • Adherence – Pili, capsules, cell wall components – binding to receptors on host cells • Colonization – Compete for iron, nutrients – Resist opsonization – Resist resident microbiota’s antimicrobials • Invasion/translocation – Type III secretion systems – Directed uptake – Exploitation of antigen sampling processes Type III Secretion System • Pore-forming protein inserted in host cell membrane = type III translocon • aka“injectisome” – bacterial proteins = virulence factors are injected into host cell cytoplasm Exploitation of antigen sampling processes Avoiding host defenses • Hide in cells • Avoid complementmediated killing • Avoid phagocytosis • Survive in phagocytes • Avoid antibodies Avoiding phagocytosis: Don’t get seen, don’t get recognized or don’t get caught – C5a peptidase – C3b binding sites: capsules, M protein – Membrane damaging toxins – Fc receptors Surviving in phagocytes • Escape from phagosome • Block fusion of the phagosome and lysosome • Survive in the phagolysosome Avoiding antibodies • IgA protease • Antigenic variation • Molecular mimicry Disease: damage to host • Damage caused by bacterial exotoxins – Proteins synthesized by bacteria – Highly specific interactions with host cells – Highly immunogenic • Toxoids • Antitoxin Disease: damage to host • Damage caused by the immune response – Inflammation – Immune complex deposition – Cross-reaction of antibodies with host tissues Types of exotoxins: functional/target tissue classification • Enterotoxins: bind to receptors on enterocytes; alter function but do not kill target cells • Neurotoxins: target cells in peripheral nervous system, interfere with nerve signal transduction (↑ or ↓) • Cytotoxins: receptors may be present on a single cell type or many cell types; toxin is lethal to target cells Types of exotoxins: structural/mechanistic classification • A-B toxins – Inhibit protein synthesis – Interfere with cell signaling systems • Membranedamaging toxins • Superantigens Diseases caused by A-B type exotoxins • Cytotoxins – Anthrax: Bacillus anthracis – lethal toxin, edema toxin (A-B toxins) – Pertussus (whooping cough): Bordetella pertussis – pertussis toxin (A-B toxin) – Diphtheria: Corynebacterium diphtheriae – diphtheria toxin – Hemolytic uremic syndrome: Escherichia coli O157:H7 – Bacillary dysentery: Shigella dysenteriae (and less severe forms caused by other Shigella species) Diseases caused by A-B type exotoxins • Enterotoxins – Cholera: Vibrio cholerae – Traveler’s diarrhea: many possible etiologies, but most cases are caused by enterotoxigenic strains of Escherichia coli Diseases caused by A-B type exotoxins • Neurotoxins – – – – Botulism: Clostridium botulinum Tetanus: Clostridium tetani Diseases caused by membrane-damaging exotoxins • Gas gangrene: Clostridium perfingens • Strep throat: Streptococcus pyogenes • Abscesses – pyogenic bacteria (many) Diseases caused by superantigens • Some foodborne intoxications • Toxic shock syndromes • Autoimmune disease, i.e. rheumatoid arthritis Anthrax Etiologic agent: Bacillus anthracis Toxins: edema toxin (protective antigen + edema factor) and lethal toxin (protective antigen + lethal factor) Toxin type: A-B toxins B component of both = protective antigen A component of edema toxin = edema factor A component of lethal toxin = lethal factor Target cell: many cells, many mammals – receptor =highly conserved Diphtheria Etiologic agent: Corynebacterium diphtheriae Toxin: diphtheria toxin Toxin type: A-B toxin Cell type with receptor: many human cells Toxin is encoded by a bacterial phage (virus) Botulism Etiologic agent: Clostridium botulinum = G+ rod; obligate anaerobe; widespread Toxin: BoNTs Toxin type: A-B toxins Target cell: motor nerves at NM junction – people and dogs most suscecptible Effect: blocks release of acetylcholine = excitatory neurotransmitter → no nerve signal transmission → flaccid paralysis Tetanus Etiologic agent: Clostridium tetani = G+ rod; obligate anaerobe; widespread Toxin: TeTx Toxin type: A-B toxin Target cell: spinal cord – receptors are highly conserved but susceptibiltiy is variable; people & horses most susceptible Effect: blocks release of GABA and glycine = inhibitory neurotransmitters → spastic or rigid paralysis Cholera Etiologic agent: Vibrio cholerae Toxin: cholera toxin Toxin type: A-B toxin Cell type with receptor: human enterocytes Effect: secretion of Cl-; H2O and Na+ follow = severe watery diarrhea Superantigens • Bind directly to the outside of MHC-II molecules and the TCRs • Activate many T4lymphocytes • A specific TCR is not required for activation. Endotoxin • Non-specific: triggers innate immune response; no antibody to endotoxin is produced • Effect on cells is widespread • A component of all (and only) Gram-negative bacteria Viral pathogenesis • Binding to host cells • Invasion of host cells • Interference with host defenses • Regulation of apoptosis