Peripheral Circulation & Regulation Chapter 21
advertisement

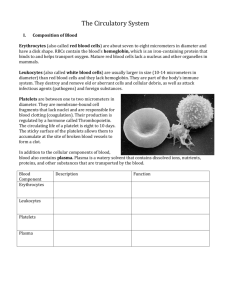
Chapter 21 Peripheral Circulation & Regulation Vessels carrying blood away from the heart Arteries – carry blood away from the heart and toward the body organs/tissues Most arteries carry blood rich in oxygen exception – Pulmonary Aorta & arteries (heart lungs) Arterioles – smaller branches of the arteries Capillaries – smallest vessels – this is the exchange point between the circulatory system and the tissues. Nutrients & O2 pass to tissues from capillaries Waste products from tissues into capillaries Capillaries – Several Types Capillaries – first stage on return to heart, typically only slightly larger than the diameter of a single RBC. Capillaries are composed primarily of a layer of simple squamous epithelium, external to this is a basement membrane then a delicate layer of connective tissue Continuous Capillaries– have no areas where substances can freely flow across the epithelial cells. No pores. Substances must be VERY small to go through endothelial cells or must be actively transported. O2 can flow across due to small size. Continuous capillaries are an effective part of the blood brain barrier. Several more types… (next slide) Capillary types cont. Fenestrated Capillaries – have fenestrae (“windows”) areas 70-100 m in diameter where the cells have no cytoplasm, simply a porous diaphragm. Highly permeable areas. Found in intestinal villi, ciliary process of eye, kidneys, endocrine glands, & choroid plexus of brain. – “leaky capillaries” Sinusoidal Capillaries – relatively large lumen (inner diameter) occur in endocrine glands allowing for greater blood flow and thus greater absorption of hormones produced in these areas Sinusoids – still larger diameter sinusoidal capillaries (may lack a basement membrane). Found in liver & bone marrow, often have macrophages associated with their interior More Capillaries Venous Sinuses – also larger than sinusoidal capillaries, occur in spleen. These have large gaps between their endothelial cells (actual gaps in wall of capillary) As you can see, capillaries range from being almost impermeable to relatively leaky. This changes with capillary type, and with location within the body Networking – Capillaries are often arranged in branching networks. Blood flows into these networks through small branches off the arterioles know as metarterioles. Branches of the metarterioles form the arterial half of the capillary bed Flow is controlled by precapillary sphincter muscles Return to Heart While flow into a capillary bed is often controlled by precapillary sphincter muscles. The return half usually lacks these ‘valves’ – free flow Venules – vessels slightly larger than capillaries which drain the capillary beds Veins – larger still… these vessels merge into gradually larger veins which proceed back to the heart. Largest diameter veins are the superior & inferior vena cava which drain the upper & lower portions of the body into the heart Structural information about arteries & veins follows… Wall of “Typical” Blood Vessel 3 distinct layers – it’s not really THIS easy. but you’ll see that in a moment… Tunica intima (inside layer) Tunica media (… middle layer) Tunica externa (you guessed it! – external layer) sometimes called tunica adventitia Fig 21-3 – ‘typical’ vessel - this is similar to a muscular artery which we will discuss in a moment Tunica Intima Proceeding to describe inside to outside Tunica intima Endothelium layer of simple squamous called Basement membrane a delicate layer of connective tissue Internal Elastic Membrane – elastic fibers (fenestrated) Tunica Media Smooth muscle cells Allows for control of blood flow by contraction or relaxation Vasoconstriction or Vasodilation Some elastic and collagen fibers may be present (varies with size of vessel) some longitudinally oriented smooth muscle in some arteries near the border of the tunica intima. External elastic membrane occurs at the outer edge of tunica media in elastic arteries (see figure later) Tunica Adventitia (externa) Connective tissue – eventually merges with the connective tissue surrounding the blood vessel Composition varies from dense connective tissue near T. media, to loose connective tissue near its outer edge Elastic Arteries Largest arteries – sometimes called Conducting Arteries Larger amount of elastic tissue, smaller amount of smooth muscle. Much elastic fiber in the tunica media. Blood pressure higher in these vessels – they are nearer to the heart. Their elastic nature lets them tolerate fluctuations between systole and diastole Tunica intima – relatively thick Tunica adventitia relatively thin Muscular Arteries Midsize arteries – large enough to have distinct names More muscle in the tunica media than seen in elastic arteries 25 – 40 layers of smooth muscle – circular arrangement Yes, I know when you look at the figures, it looks like less muscle. Remember these are smaller in diameter than the elastic arteries… Tunica intima has well developed internal elastic membrane In general – arteries tend to be muscular and elastic elastic artery muscular artery Arterioles Tunica intima has no obvious internal elastic membrane Tunica media has only one or two layers of smooth muscle cells which wrap circularly (capable of constricting vessel) Capable of vasoconstriction & vasodilation Venules Diameter of 40-50 microns Endothelium plus a basement membrane Walls thin enough for substantial nutrient exchange, similar to capillaries Except for larger size these are structurally very similar to capillaries Small veins Larger than veinules Have an outer layer (tunica adventitia) of collagenous connective tissue Walls too thick to allow much nutrient exchange to take place Medium & Large Veins Thin tunica intima (mostly epithelium) Thin tunica media – a sparse layering of smooth muscle, some collagen and a very few elastic fibers Tunica adventitia – most prominent layer, mostly collagenous connective tissue Valves in Veins Veins larger than 2mm have one-way valves These valves prevent backflow, permit blood to flow toward the heart, but not away from the heart Structure – two ‘leaflets’ or flaps overlapping in the vein when blood flows backward it presses the flaps closed More valves present in lower extremities than in other parts of the body – Naturally! They prevent flow against gravity Varicose veins due to failed valves allowing blood to pool Blood Supply to Vessels! Yes, they need blood too, and don’t get it from ‘inside’ Vasa vasorum – small blood vessels providing nutrients to all blood vessels greater than 1mm in diameter Vessels smaller than 1mm can absorb nutrients from the blood they carry Laminar Flow Blood does not flow in ‘one bulk unit’ through a blood vessel Flow is much like the currents in a river This type of flow helps reduce turbulence The End Day 1 Ch 20. Day 2 Chapter 21 Continues…. Peripheral Circulation & Regulation Blood Flow Flow – how much blood passes between two points in a given amount of time Flow is affected by : Pressure exerted on the blood by the heart Resistance (friction) from the walls of the blood vessel Two types of flow Laminar Turbulent fig 21.32 p 674 Turbulence Any constriction of a blood vessel decreases rate of flow & creates turbulence Turbulence creates resistance, usually by narrowing the vessel Cross Sectional Diameter (related to blood flow) Greater CSD = less resistance and blood flow This differs from Total Cross Sectional Area Total Cross Sectional Area determined by the diameter of the vessel and # of vessels For example, the aorta is relatively large in diameter but there is only one aorta An individual capillary is quite small in diameter but there are millions of capillaries greater TCSA in capillaries Blood flows faster in aorta even though capillaries have a greater TOTAL area velocity of flow fig 21.34 p 677 More factors affecting flow Viscosity – the ‘thickness’ of blood or its resistance of a liquid to flowing In blood this is, in large part due to the Hematocrit (packed cell volume) If blood viscosity increases, more force must be applied to get it to move, producing more friction against the vessel wall Blood Pressure – Pressure exerted against the walls of a blood vessel by the blood Blood Pressure affects flow also… Blood Pressure – Pressure exerted against the walls of a blood vessel by the blood Needed to keep blood vessels open If BP decreases below a Critical Closing Pressure vessels will collapse Force = Diameter x Pressure (see LaPlace’s Law pg 676) CCP important in cardiovascular shock: BP decreases vessels collapse vessels downstream loose pressure and collapse (heart attack or electrocution) Blood Pressure as a Clinical Factor Force exerted on a vessel keeps it moving BUT some pressure is expended against the wall of the vessel If this pressure is too great the wall of the vessel can be damaged Damage to vessel wall increases the rte at which plaque is deposited, increasing chance of stroke & heart attack Systolic Pressure – exerted when heart is contracting (maximal) Diastolic (residual BP) – exerted when heart is relaxing, this is the least amount of pressure a vessel is under at any given time DIASTOLIC is more important Blood Pressure… Normal BP 120/80 (systolic/diastolic) Clinically you are hypertensive (high blood pressure) if: Systolic > 165 OR Diastolic >90 Measuring BP clinically Sphygmomanometer – “that cuff thingy” Sphygmomanometer – includes an inflatable cuff and a method of measuring (column of mercury or digital readout) Stethoscope placed over brachial artery Pump inflates cuff over brachial artery (constricting flow) until no sound is heard Pressure slowly released until first sound heard = Systolic Dramatic change in sound (no sound) = Diastolic Vascular Compliance Compliance = increase in volume (mL) --------------------------------increase in pressure (mm Hg) Tendency for vessel volume to increase as pressure increases Greater elasticity greater compliance Lower elasticity lower compliance Veins are much more compliant than are arteries about 24:1 - walls of arteries too muscular to be very compliant So… veins act as a ‘storage’ area for blood volume Pulse Pressure Serves as an index of whether BP is or Systolic – Diastolic = PP Vascular Compliance affects pulse pressure since it reflects the vessels ability to increase in volume as BP increases Compliance decreases with age (less elastic): decreased compliance causes pulse pressure Stroke Volume of the heart also affects PP as SV - PP Stroke volume – volume pumped from one ventricle with each heartbeat Pulse Pressure – fig 21.35 p 679 Starling’s Law of Capillaries Equal volumes of fluid move out of the capillaries at the arteriole end and at the venous end Factors affecting Starling’s Law: At arteriole end Hydrostatic Pressure dominates: Result - pushes fluids into tissues At venous end Osmotic Pressure (pull) dominates: pulls fluids from tissues back into blood vessel 15% of fluid remains in tissues and is ultimately removed by the lymphatic system Regulation of BP – Short Term Baroreceptor Reflexes Adrenal Medullary Mechanism Chemoreceptor Reflexes CNS Ischemic Response Vasomotor Center Blood vessel diameter is controlled by this (VM) center in the medulla oblongata Stimulation from the VMC increases muscle tone in blood vessels (especially arteries) which causes vasoconstriction If blood pressure coming from heart increases this is detected by baroreceptors (pressure receptors) in the aortic arch and in the carotid arteries These receptors send an afferent signal via glossopharyngeal and vagus nerves which inhibits VMC With VMC inhibited vessels relax vasodilation and BP decreases decreased BP vasoconstriction Adrenal Medulla Activated when stimulated by sympathetic nervous system increases secretion of epinephrine and smaller amounts of norepinephrine These hormones increase heart rate & stroke volume Also cause vasoconstriction in skin and gut Additionally cause vasodilation in heart Rapid onset, short duration Cardiac Regulatory Center in Medulla oblongata Chemoreceptors located in Aorta and in Carotid artery Detect levels of CO2, O2, and blood pH If pH is low (acidic) and CO2 is high these signal the CRC which stimulates the sympathetic nervous system Sympathetic increases heart rate and causes vasoconstriction Decreases in CO2 , and increased pH result in decreased heart rate and in vasodilation CNS Ischemic Response RARE – Is important only when the blood supply to the Vasomotor Center decreases dramatically (less O2) VMC stimulates vasoconstriction causing BP to rise dramatically Occurs only when BP falls below 50 mm Hg This is used as a message to say: Get blood to the brain NOW! Long Term BP regulation Renin-Angiotensin-Aldosterone Mechanism Vasopressin Mechanism Atrial Natriuretic Mechanism Renin-Angiotensin-Aldosterone Mechanism Kidneys release an enzyme - Renin Renin acts on angiotensinogen (a blood protein) Causes angiotensinogen to release a fragment called angiotensin Angiotensin is then activated by another enzyme called angiotensin-converting enzyme Angiotensin II (active form) Angiotensin II causes vasoconstriction & it stimulates the adrenal cortex to release aldosterone Aldosterone causes kidneys to retain Na, Cl & water Angiotensin II also causes thirst and salt craving and ADH secretion – all cause increase blood volume Renin-Angiotensin-Aldosterone Vasopressin When dissolved solids in blood increase or when BP decreases the hypothalamus increases secretion of vasopressin (ADH) from the posterior pituitary Vasopressin (ADH) – causes kidneys to reduce production of urine – increasing the amount of fluids in blood Vasopressin also acts as a mild vasoconstrictor Vasopressin Mechanism Atrial Natriuretic Mechanism Atrial Natriuretic Hormone – released from cells in atrium Release of ANH stimulated by increased venous input to atrium ANH causes kidneys to increase urine production and excretion of sodium – this decreases blood volume Chapter 21 That’s it for now…