CARDIOVASCULAR EMERGENCIES Temple College ECA
advertisement

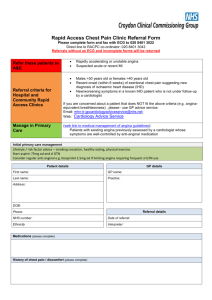
CARDIOVASCULAR EMERGENCIES Temple College ECA Cardiovascular Disease 63,400,000 Americans have one or more forms of heart or blood vessel disease 50% of all deaths are cardiovascular disease Cardiovascular Disease Acute Myocardial Infarction (Heart Attack) - leading cause of death in U.S. 1.5 million Americans will have AMI’s this year Of these .5 million will die! 350,000 will die in first two hours! Cardiovascular Disease Acute Coronary Syndromes Acute Myocardial Infarction Non ST Segment Elevation (NSTEMI) ST Segment Elevation (STEMI) Unstable Angina Pectoris Stable Angina Pectoris Cardiovascular Disease Risk Factors Major Uncontrollable Age Sex Race Heredity Cardiovascular Disease Risk Factors Major Controllable Smoking High BP High blood cholesterol Diabetes Cardiovascular Disease Risk Factors Minor Controllable Obesity Lack of exercise Stress Personality Cardiovascular Disease Control of risk factors = decrease in Coronary Artery Disease and Acute Myocardial Infarction Coronary Artery Disease Myocardium (heart muscle) requires continuous oxygen and nutrient supply Myocardial blood supply passes through coronary arteries Coronary Artery Disease Atherosclerosis Narrowing of lumen plaque formation - related to Risk Factors results in decreased myocardial perfusion Poor tissue perfusion causes: tissue damage (ischemia) tissue death (infarction) Atherosclerotic Plaque Formation Angina Pectoris “A choking in the chest” Angere - to choke Myocardial oxygen demand exceeds supply during periods of increased activity, exercise, or stressful event Angina Pectoris During stress the myocardium demands more O2 Coronary arteries would normally dilate to supply more blood and O2 In Angina Pectoris, the coronary arteries are unable to dilate sufficiently to increase perfusion Classic Presentation Chest Pain SOB Diaphoresis N/V NOT ALL PATIENTS READ THE TEXTBOOK! Symptoms -Angina Pectoris Pain Substernal Squeezing/Crushing/Heaviness May radiate to arms, shoulders, jaw, upper back, upper abdomen back May be associated with shortness of breath, nausea, sweating Symptoms -Angina Pectoris Pain usually associated with 3E’s Exercise Eating Emotion Symptoms -Angina Pectoris Pain seldom lasts > 30 minutes Pain relieved by Rest Nitroglycerin Symptoms -Angina Pectoris Great anxiety/Fear Fixation of the body Pale, ashen, or livid face Dyspnea (SOB) may be associated Symptoms -Angina Pectoris Nausea Diaphoresis BP usually up during attack Dysrhythmia may be present Angina Pectoris Following an angina attack there is no residual damage to the myocardium Forms of Angina Pectoris Stable Angina Occurs with exercise Predictable Relieved by rest or Nitroglycerin Forms of Angina Pectoris Unstable More Angina frequent/severe Can occur during rest May indicate impending MI Requires immediate treatment and transport to appropriate facility Acute Myocardial Infarction “Heart Attack” Inadequate perfusion of myocardium Death of myocardium Infarct Damage to myocardium Ischemia Symptoms - AMI Chest Pain - cardinal sign of myocardial infarction Occurs in 85% of MI’s Substernal “Crushing,” “squeezing,” “tight,” “heavy” Symptoms - AMI Chest Pain May radiate to arms, shoulders, jaw, upper back, upper abdomen back May vary in intensity Unaffected by: swallowing coughing deep breathing movement Symptoms - AMI Chest Pain Unrelieved by rest/nitroglycerin Pain lasts longer than angina pain (up to 12 hours) “Silent’ MI 15% of patients with MI, particularly common in elderly and diabetics Symptoms - AMI Shortness of breath Weakness, dizziness, fainting Nausea, vomiting Pallor and diaphoresis (heavy sweating) Symptoms - AMI Sense of impending doom Denial 50% of deaths occur in first two hours Average patient waits 3 hours before seeking help Symptoms - AMI Changes in pulse, BP, respiration are not diagnostic of AMI Acute Myocardial Infarction Early recognition of MI is critical Management of Cardiac Chest Pain When in doubt, manage all chest pain as MI Management of Cardiac Chest Pain Begin management immediately if angina or MI are suspected. Complete the history and physical exam as you treat. Management of Cardiac Chest Pain Position of Comfort Patent Airway High concentration O2 non-rebreather mask 10-15 lpm Management of Cardiac Chest Pain Reassure the patient Obtain a brief history and physical exam Aspirin 325mg p.o. Management of Cardiac Chest Pain Nitroglycerin Patient 0.4mg tablet sublingual should be sitting or lying down Has Pt. Taken nitroglycerin in last 10 minutes? Is pain relieved? Headache? Is BP > 100 systolic? q 5 minutes until pain relieved or three tablets administered Management of Cardiac Chest Pain If pain is unrelieved by rest, oxygen, nitroglycerin or if a change has occurred in pattern of angina, transport immediately Transport in semi-sitting position if BP normal or elevated; flat if BP low Management of Cardiac Chest Pain Do not walk patient to the ambulance Do not use lights/siren if patient is awake, alert, breathing without distress Monitor vital signs every 5-10 minutes Management of Cardiac Chest Pain Request Deaths early ALS back-up in MI result from arrhythmia's Arrhythmia's can be prevented with early drug therapy Hypertension Condition Chronic Acute Pathophysiology Increased pressure to organs Reduced blood flow Increased Afterload Congestive Heart Failure CHF = Inability of heart to pump blood out as fast as it enters. Type left-sided right-sided both. Causes of CHF Coronary Artery Disease Chronic hypertension (high blood pressure) AMI Valvular heart disease Congestive Heart Failure Usually begins with left-sided failure. Increased workload on left ventricle Left ventricle fails Blood “stacks up” in lungs High pressure in capillary beds Fluid forced out of capillaries into alveoli Congestive Heart Failure Right-sided failure most commonly caused by Left-sided failure. Blood “backs up” into systemic circulation Distended neck veins Fluid in abdominal cavity Pedal edema Symptoms of CHF Weakness Dyspnea Dyspnea on exertion Paroxysmal nocturnal dyspnea Attacks of SOB that usually occur at night that awakens the patient Symptoms of CHF Orthopnea Difficulty breathing in any position other than standing or sitting Abdominal discomfort Jugular Vein Distention (JVD) Pedal “Pitting” edema in lower extremities Symptoms of CHF Tachycardia Pulmonary Noisy, Edema labored breathing Coughing Rales, wheezing Pink, frothy sputum Heart Failure Management of CHF Sit patient up, let feet dangle Administer high concentration O2 Assist ventilation as needed Monitor vital signs q 5-10 minutes Request early ALS back-up Pacemaker Failure Position of comfort Patent airway High Concentration O2 Assist ventilations as needed ALS Intercept CPR as needed DO NOT worry about damage to pacemaker Coronary Artery Bypass Position of comfort Patent airway High Concentration O2 Assist ventilations as needed ALS Intercept CPR as needed DO NOT worry about damage to sutures/staples or by-passed arteries Implanted Defibrillator If performing CPR on a patient: Implanted defibrillator may “fire” May feel slight “tingle”