Case Presentation Using Progressive Disclosure Example slides
advertisement

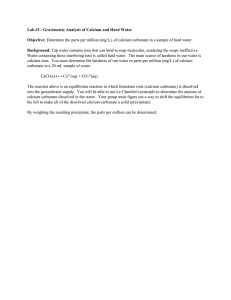
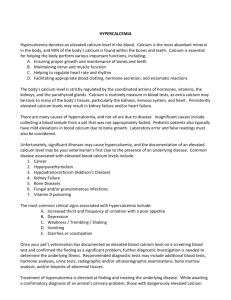
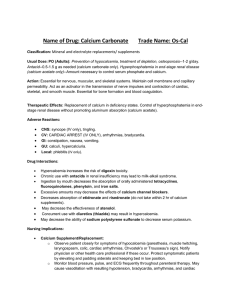
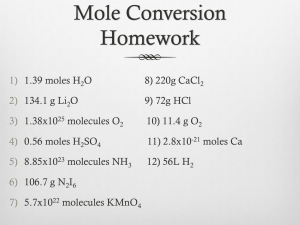
Case Presentation Using Progressive Disclosure Example slides Patient Presents to ER 66 yr old white male Complains of progressive weakness for 2 weeks Intermittent cough, pleuritic chest pain and exertional dyspnea for 6 days Nausea and vomiting for 2 days PTA What questions do you ask in history? History hypertension coronary artery disease MI 1989 long history of heartburn – takes 300 Tums per week and drinks a gallon of milk every other day Physical Exam appears weak vital signs stable oral mucosa and tongue dry Lungs: bibasilar crackles Cardiac: S3 gallop What do you order? Labs/X-ray Serum Ca = 15.1 mg/dL BUN = 65 mg/dL Creatinine = 5.9 mg/dL Intact PTH and 1,25 DihydroxyvitaminD levels were normal Serum phosphate = 4.9 mg/dL Serum dicarbonate = 38 mmol/L Chest x-ray showed bilateral basilar infiltrates What is your differiential diagnosis? Hypercalcemia of malignancy? Primary hyperparathyroidis? Milk-alkali syndrome? Immobilization? Multiple Myeloma? Milk-alkali Syndrome Presents with the triad of hypercalcemia, alkalosis and renal failure Occurs in acute, subacute, and chronic forms Milk-alkali Syndrome Related to excessive ingestion of calcium and absorbable antacids such as calcium carbonate and milk First reported in 1923 – thought to be a toxic reaction to the then popular Sippy treatment of peptic ulcer disease. The Sippy regimen: hourly administration of milk or cream with a mixture of bicarbonate containing salts that included calcium carbonate. Milk-alkali Syndrome Became rare with the advent of modern ulcer therapy with nonabsorbable antacids, H2 blockers and sucralfate. May be an increased frequency of this syndrome because of the growing popularity of over-the-counter calcium carbonate marketed either as antacids or as calcium supplements for the prevention of osteoporosis What is your treatment plan? Treatment Plan Hospitalization, hydration, and diuresis Discontinue injestion of calcium IV Lasix and fluids If life threatening: short course high dose calcitonin (Calcimar) (8 IU per kg IM Q 68) Consult? Consult? Consult if renal failure might require dialyses. Prevention Milk-alkali syndrome might easily be prevented by restricting calcium intake to 1.2 to 1.5 g/day or by using a supplement that does not contain absorbable alkali. Recent Articles Medline search of ‘94-present yielded 10 hits. Brandwein SL, Sigman KM, Case report: milk-alkali syndrome and pancreatitis., Am J Med Sci 308: 3, 173-6, Sep, 1994. – The relation between hypercalcemia and pancreatitis, first described in patients with hyperparathyroidism, is controversial. Other causes of hypercalcemia also have been associated with pancreatitis. In this report, the authors describe a patient with pancreatitis and the milk-alkali syndrome who had the classic triad of hypercalcemia, alkalosis, and renal insufficiency. The authors also review the literature for all the reported cases of pancreatitis associated with hypercalcemia. Recent Articles Muldowney WP, Mazbar SA, Rolaids-yogurt syndrome: a 1990s version of milk-alkali syndrome., Am J Kidney Dis 27: 2, 270-2, Feb, 1996. Milk-alkali syndrome is characterized by progressive hypercalcemia, systemic alkalosis, and renal insufficiency. After calcium carbonate is ingested with diary products, hypercalcemia and alkalosis may develop in susceptible persons, particularly those with underlying renal insufficiency. We describe a young woman who neither drank milk nor had peptic ulcer disease, yet who ingested enough calcium carbonate to require admission to an intensive care unit for acute renal failure. Chronically bulimic, she was taking Rolaids (Warner-Lambert Co, Morris Plains, NJ), which contained calcium carbonate, and was eating yogurt daily to prevent osteoporosis. We discuss the characteristics and complex metabolic interactions of the milk-alkali syndrome, a critical but generally reversible electrolyte disorder. Early recognition of coincident hypercalcemia and alkalosis and prompt cessation of calcium carbonate ingestion are essential for successful recovery. Finally, we suggest that nephrologists should discourage patients with renal insufficiency and chronic vomiting from consuming calcium-containing antacids and excessive dietary calcium. How do you ICD9 code this? 275 Disorders of mineral metabolism – 275.40 Disorders of calcium metabolism hypercalcemia, calcilosis, . . 276 Disorders of fluid, electrolyte, & acidbase balance – 276.30 Alkalosis – – NOS, respiratory, metabolic 276.50 Volume depletion disorder 276.9 Electrolyte & fluid disorders not elsewhere classified