Document 15541760
advertisement

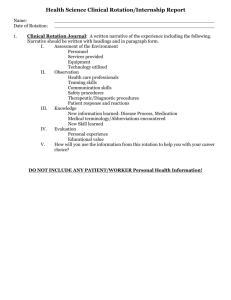
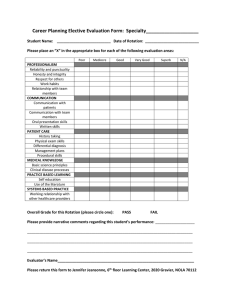
http://www.medschool.lsuhsc.edu/emergency_medicine/critical_concepts_rotation.aspx WELCOME TO CRITICAL CONCEPTS ROTATION OBJECTIVES: Provide all senior students with exposure to acute and critical care concepts in a variety of learning modalities. Review and reinforce diagnostic and management skills in common and/or critical disease entities and procedures encountered in a range of specialties. Prepare senior students for their new roles as resident physicians with direct patient care and health care team responsibilities. UNDERLYING PRINCIPLE Every physician – regardless of specialty – should know how to manage acutely ill, undifferentiated patients with a variety of emergent conditions CLINICAL SCENARIOS: Case 1 JUNE 5, 2014 When suddenly … “Is there a doctor on the plane? your picture here A 63 year old woman traveling alone in first began shouting incoherently and wandering around about ten minutes ago. Suddenly, she slumps forward and becomes unresponsive. The flight attendant hands you a medical bag. You are able to feel a weak radial pulse at approximately 110 beats/minute and note a respiratory rate of 8 breaths/minute. CLINICAL SCENARIOS: Case 2 JULY 1, 2014 When suddenly … your pager goes off … A 60 year old man admitted to the floor got up to go to the restroom. Suddenly, he fell back into bed and became unresponsive. The floor nurse goes out to find a code cart. You are able to feel a weak radial pulse at approximately 120 beats/minute and note a respiratory rate of 10 breaths/minute. CLINICAL SCENARIOS: Case 3 October 10, 2014 You are on your EM rotation on a busy night shift when … EMS brings in a 57 year old man who was an unrestrained driver in a rollover MVC with multiple cars. He was not responsive at the scene. Vital signs in the ambulance were HR 115, BP 100/60, and RR 10. All of the EM residents are busy working up the other cars’ passengers. WHAT NOW?? What would your immediate actions be In the air? If/when this happens to you on your first day of internship? If you are the first medical professional caring for an acutely ill/injured patient? FOR EACH CASE - LIST 5 OF THE FOLLOWING: Initial actions Possible diagnoses Management/treatment steps MANAGEMENT OF THE ACUTELY ILL PATIENT Based on the principles of identifying and treating the immediate, life-threatening conditions first All other considerations come second KEEP IT SIMPLE PRIMARY SURVEY VITAL SIGNS = CRITICAL IMPORTANCE HR RR BP Temp Pulse Ox PRIMARY SURVEY A – airway evaluation Are there any signs of obstruction? ○ FB ○ Masses ○ Trauma ○ TONGUE INTERVENTIONS RELIEVE THE OBSTRUCTION before moving on ○ Finger sweep ○ Chin tilt/head lift or jaw thrust ○ Repositioning ○ Suctioning/hemorrhage control FUTURE AIRWAY PROTECTION? PRIMARY SURVEY B – breathing, oxygenation & ventilation Is the patient able to sufficiently oxygenate and/or ventilate? Look for ○ Agitation/restlessness ○ Tachypnea/use of accessory muscles ○ Bradypnea/apnea ○ Breath sounds on BOTH sides ○ Tracheal deviation? ○ JVD? PRIMARY SURVEY Life threatening conditions requiring immediate intervention Tension PTX Flail chest Respiratory failure/distress ○ Primary pulmonary issue ○ Consequence of underlying disorder INTERVENTION: Assisted oxygenation/ventilation through ○ Supplemental O2 (how much & how?) ○ Proper bag-valve-mask ○ Non-invasive positive pressure ventilation ○ Intubation (RSI) PRIMARY SURVEY C – circulatory status Assess for PULSES (bilaterally) and heart tones Any obvious bleeding? Other s/s: ○ MS changes ○ Cool, pale extremities ○ Capillary refill ○ BP/HR – shock index PRIMARY SURVEY Life threatening conditions requiring immediate intervention Shock states: ○ Hypovolemic? ○ Cardiogenic? ○ Distributive? ○ Obstructive? Active hemorrhage INTERVENTION Venous access (large bore/CVC) Administration of blood or fluid products in rapid boluses Target to specific types of shock: Cardiogenic – inotropes, BP support, procedures Sepsis (distributive) – EGDT, source control Obstructive (PE/tamponade) Anaphylactic – epi, antihistamines PRIMARY SURVEY D – disability assessment Mental status/level of consciousness Gross neurologic exam Pupils GCS if trauma INTERVENTION Prompt imaging as warranted (trauma – hemorrhage or fracture; medical – CVA/mass) Prompt Neuro specialist involvement if appropriate Reversal/supportive care if toxidrome Consider likelihood of airway protection (“GCS less than 8 = intubate”) PRIMARY SURVEY E – FULL exposure Every inch of the patient is surveyed and documented for obvious life threats Occult traumatic injury Infectious sources Rashes/skin changes Medications/patches INTERVENTIONS Imaging/tests/treatment based on findings Removal of any offending agent After stabilization … Brief, targeted HPI/PMH etc. (“AMPLE”) REASSESSMENT OF VITAL SIGNS and success of any intervention Detailed testing Longer-term treatment and management Secondary survey: FULL PHYSICAL! GOALS … in the care of the undifferentiated patient: Identify life-threatening processes Immediate stabilization Consideration of most serious and most likely diagnoses Initiation of definitive treatment and care Utilization of all available resources when appropriate DON’T BE AFRAID … This is fun! ROTATION HOUSEKEEPING Course structure and expectations; 1 didactics week 2 EM weeks 1 ICU week You are expected to be an active participant in all parts of the course, and a full member of each team (consider yourselves acting interns) YOUR GOALS What should you get out of this? Expanded skills and knowledge base from 3rd year Application of those skills/knowledge to more complicated/critically ill patients Increased exposure to/experience with common and emergent procedures & interventions More sophisticated understanding of disease complexity & health systems management Most of you are here: REPORTER WHO WHAT WHERE WHEN We want to move you here: INTERPRETER MANAGER HOW WHY WHAT NEXT? DIDACTICS WEEK Please read assigned material on website prior to each session … come prepared to discuss! Each of the 9 specialties has designed their own interactive module on what they perceive to be most important in managing their most critical or common emergencies Each module requires a faculty/preceptor signature ICU ROTATION You are an active part of the ICU team and expected to have direct patient care and documentation duties You should participate in family and team discussions of care plans Details will differ between ICUs Information on where/when to report to ICUs – see CC website under “Didactics Schedule & ICU Information”* *TICU students – please contact fellows for time/place to meet prior to starting the week EM ROTATION Again, you are expected to have direct patient care responsibilities as part of the EM team Please read the assigned EM readings during your 2 week block While on the EM portion of the rotation, you are expected to attend EM student lectures and labs CASE & PROCEDURE LOGS During your EM block, please log all patient encounters and procedures that you observe, assist with, and/or perform into New Innovations This is a way to begin to build your medical portfolio RESPONSIBILITIES BE ON TIME … for all sessions, rounds, and shifts Adhere to the school honesty policy at all times Be properly supervised in all educational and clinical settings and duties EVALUATION METHODS Final grade is based on: End of rotation on-line exam, derived from: ○ EM and specialty-specific reading (all online on website) ○ Social media content ○ Didactic session lectures and labs Professionalism assessment during clinical rotation H/HP/P/F system Either component can be remediated if necessary ATTENDANCE POLICY Students may miss 2 days of the rotation FOR INTERVIEWS ONLY: During EM block – may miss 1 ED shift and one “free” day During ICU block – if 2 ICU days are missed, they must be remediated the weekend before or after (in order to have a full week of ICU) DIDACTICS DAYS MAY NOT BE MISSED Please contact Dr. Avegno for attendance questions FORMS Please turn in evaluation form to Jennifer Jeansonne, course coordinator, upon completion of the rotation (room 615) NOW … ENJOY THE COURSE!