Annex 2f Evaluation and record of diagnosis of VS or MCS (DOC, 0.07MB)
advertisement
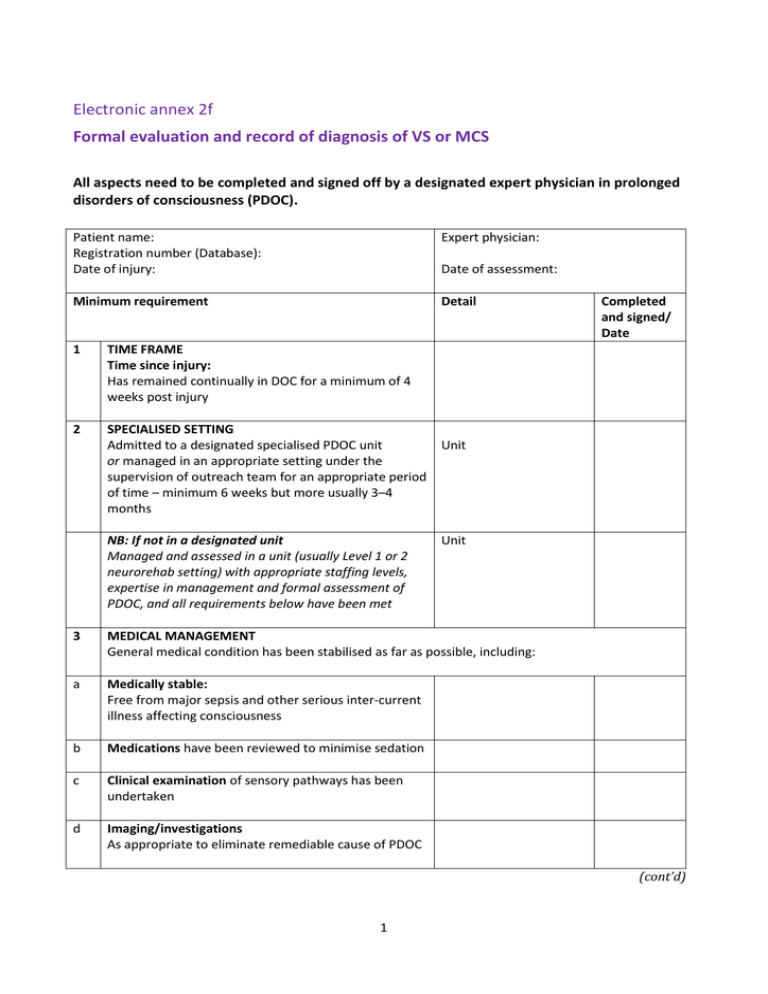
Electronic annex 2f Formal evaluation and record of diagnosis of VS or MCS All aspects need to be completed and signed off by a designated expert physician in prolonged disorders of consciousness (PDOC). Patient name: Registration number (Database): Date of injury: Expert physician: Minimum requirement Detail Date of assessment: 1 TIME FRAME Time since injury: Has remained continually in DOC for a minimum of 4 weeks post injury 2 SPECIALISED SETTING Admitted to a designated specialised PDOC unit or managed in an appropriate setting under the supervision of outreach team for an appropriate period of time – minimum 6 weeks but more usually 3–4 months NB: If not in a designated unit Managed and assessed in a unit (usually Level 1 or 2 neurorehab setting) with appropriate staffing levels, expertise in management and formal assessment of PDOC, and all requirements below have been met Completed and signed/ Date Unit Unit 3 MEDICAL MANAGEMENT General medical condition has been stabilised as far as possible, including: a Medically stable: Free from major sepsis and other serious inter-current illness affecting consciousness b Medications have been reviewed to minimise sedation c Clinical examination of sensory pathways has been undertaken d Imaging/investigations As appropriate to eliminate remediable cause of PDOC (cont’d) 1 Minimum requirement Detail 4 SPECIALIST MANAGEMENT PROGRAMME All essential requirements for management are addressed: a Tone: Active spasticity management in place, including medication b Positioning: A 24-hour programme of positioning is in place with a range of positions available including bed and chair (unless contraindicated) c Has appropriate seating system and sitting tolerance at least 1 hour at a time – preferably up to several hours/day or, if in bed – at least sitting up in profile in midline for 1 hour d Arousal levels recorded: Measures have been taken to maximise arousal e Optimised environment: Consideration has been given to optimising the environment for interaction (adequate light, avoidance of distraction/ overstimulation, rest periods) f Facilitated communication: Has been assessed by clinicians experienced in PDOC to explore ability to access switches/use of communication aids etc g Controlled sensory stimulation programme: Patient has been exposed to a range of controlled stimuli 5 FAMILY/IMPORTANT RELATIONSHIPS Family informed and educated re sensory stimulation and responses etc, and involved in the programme (if able). 2 Completed and signed/ Date 6 Detail FORMAL ASSESSMENT (cont’d) Checked and signed/Date FOR CONTINUING VS OR MCS Has undergone formal assessment as follows: Acute setting/ITU : ‒ WHIM (at least 10 occasions) Rehabilitation/post-acute: VS or ?MCS minus No awareness or no consistent responses seen, ie VS or MCS WHIM at least 2–3 per week over 4 weeks or full SMART other assessments (eg CRS-R) optional MCS Clear evidence of awareness and response albeit inconsistently WHIM at least 2–3 per week over 4 weeks SMART (optional) other assessments (eg CRS-R) optional Long term: WHIM SMART – only indicated if: significant change identified by family/team and reviewed by trained assessor to establish if full re-assessment is necessary or – required to inform key decisions, eg application for withdrawal of CANH I hereby confirm that ………………………………………………………………. (Patient name) has met all of the above criteria for: ☐ Continuing vegetative state ☐ Continuing minimally conscious state (delete as applicable) Date: ……/……/……. (………………….weeks since brain injury) Signed: …………………………………………………………. Print name: ………………………………………………….. (Expert in assessment of prolonged disorders of consciousness) 3 7 Detail FORMAL ASSESSMENT Checked and signed/Date FOR PERMANENT VS OR MCS Has undergone formal assessment as follows: Time frame Date of review: VS: Non traumatic – at 6 months post injury or Traumatic – at 12 months post injury MCS: Non traumatic – at 3 years post injury Traumatic – at 5 years post injury Medical management No evidence of remediable medical condition contributing to low awareness Specialist management Patient has had an adequate period (at least 3 months) of specialist management, meeting the conditions laid out in section 4 above. Formal assessment SMART has been done …………….. Serial WHIMs over time show no significant change since the previous assessment I hereby confirm that ………………………………………………………………. (Patient name) who was diagnosed as in continuing MCS/VS on ………………………… (Date) has met all of the above criteria for: ☐ Permanent vegetative state ☐ Permanent minimally conscious state (delete as applicable) Signed: ………………………………………………………….. Print name: ………………………………………………….. Expert in assessment of prolonged disorders of consciousness Source: Royal College of Physicians. Prolonged disorders of consciousness: national clinical guidelines. London: RCP, 2013. 4