Bioterrorism and Health Care Ethics
advertisement

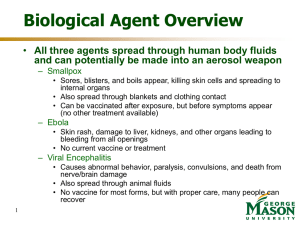
Health Care Ethics and Bioterrorism 20 April 2004 Edward P. Richards Director, Program in Law, Science, and Public Health Louisiana State University Law Center http://biotech.law.lsu.edu Scenario One 12 year old girl in the ER Fever Unusual rash with some sores Sick, but not serious What should you worry about? What do you do? Who do you call? Ethical Issues You are worried, but you do not know what you are dealing with What are the issues? More info State lab says it is not smallpox Looks like another pox, probably monkey pox Contagious, but not as serious as smallpox Only protection is smallpox vaccine What do you do now? What would have happened if it had been smallpox? Why Smallpox Bioterrorism? Stable aerosol Virus Easy to Produce Infectious at low doses Human to human transmission 10 to 12 day incubation period High mortality rate (30%) CDC Materials Herd Immunity – Key to Eradication Smallpox Spreads to the Non-immune Immunization Slows the Spread Dramatically Epidemics Die Out Naturally Herd Immunity Protects the Unimmunized You do not need 100% to end an epidemic Small Pox Vaccine History 1000 AD - China, deliberate inoculation of smallpox into skin or nares resulting in less severe smallpox infection. Vaccinees could still transmit smallpox 1796 - Edward Jenner demonstrated that skin inoculation of cowpox virus provided protection against smallpox infection 1805 - Italy, first use of smallpox vaccine manufactured on calf flank 1864 - Widespread recognition of utility of calf flank smallpox vaccine CDC Materials Small Pox Vaccine History 1940’s - Development of commercial process for freeze-dried vaccine production (Collier) 1950 - Pan American Sanitary Organization initiated hemisphere-wide eradication program Global Eradication Program 1967 - Following USSR proposal (1958) WHO initiated Global Eradication Program Based on Ring Immunization Vaccinate All Contacts and their Contacts Isolate Contacts for Incubation Period Involuntary - Ignore Revisionist History 1977 - Oct. 26, 1977 last known naturally occurring smallpox case recorded in Somalia 1980 - WHO announced world-wide eradication CDC Materials Smallpox Vaccine Live Virus Vaccine (Vaccinia Virus) Crude Preparation We Have Now Not Cowpox, Might be Extinct Horsepox Must be Infected to be Immune Prepared from the skin of infected calves Filtered, Cleaned (some), and Freeze-dried New Vaccine is Clean, but still Live Just failed the clinical trials Complications of Vaccination Local Lesion Can be Spread on the Body and to Others Progressive (Disseminated) Vaccina Deadly Like Smallpox, but Less Contagious Historic Probability of Injury Small Risk from Bacterial and Viral Contaminants Small Risk of Allergic Reaction 35 Years Ago 5.6M New and 8.6M Revaccinations a Year 9 deaths, 12 encephalitis/30-40% permanent Death or Severe Permanent Injury 1/1,000,000 What Happened Last time 1947 New York Outbreak Case from Mexico 6,300,000 Vaccinated in a Month 3 Deaths from the Smallpox 6 Deaths from the Vaccine Would Have Been Much Higher Without Vaccination? Eradication Ended Vaccinations Cost Benefit Analysis Vaccine was Very Cheap Program Administration was Expensive Risks of Vaccine Were Seen as Outweighing Benefits Stopped in the 1970s Immunity Declines with Time Universal Vulnerability Agriculture and Smallpox Isolated Communities Stays Endemic or Dies Out Forever Most Communities had Significant Immunity Synchronous Infection Break Down of Social Order Now the Whole World is Susceptible Why have the Have Risks of Vaccination Changed? Immunosuppressed Persons Cannot Fight the Virus and Develop Progressive Vaccinia Immunosuppression Was Rare in 1970 Immunosuppression is More Common HIV, Cancer Chemotherapy, Arthritis Drugs, Organ Transplants How have Attitudes toward Risk Changed? How have our attitudes about risk changed? How has this affected vaccinations? What has caused this change? Role of Medical Care Smallpox Can Reduce Mortality with Medical Care Huge Risk of Spreading Infection to Others Very Sick Patients - Lots of Resources Cannot Treat Mass Casualties Vaccinia VIG - more will have to be made Less sick patients - longer time Hypothetical 2004 Outbreak Smallpox is Spread by Terrorists in NY City 100 People are Infected They ride the Subway, Shop in a Mall, Work and Live in Different High Rise Buildings What are the Choices? Isolation and Contact Tracing Ring Immunization Mass Immunization What would you do? What if you guess wrong? Is Quarantine a Realistic Option? Proper Isolation Negative Pressure Isolation Rooms Very Few Hospitals and Motels No Respiratory Isolation is Possible One Case Infects the Rest House Arrest Need to provide income support Food Medical Care Emotional Support If many people resist, it is impossible to enforce The Costs of Mass Immunization Assume 1,000,000 Vaccinated in Mass Campaign with No Screening Assume 1.0% Immunosuppressed 10,000 Immunosuppressed Persons Probably Low, Could be 2%+ Potentially 1-2,000+ Deaths and More With Severe Illness What are the Ethical and Political Issues? Vaccinate early Stop the epidemic but with lots of complications Wait until you are sure Lots more deaths Pre-Outbreak Immunizations Can We Control who Gets the Vaccine? Introduces a Disease into the Community Can Spread Person to Person Black-market Vaccine Inoculation from Vaccinated Persons Smallpox as a Threat What should we do based on what we know now? What if we knew terrorists had the virus? What if there has been an outbreak in the mideast? What if there is an outbreak in NYC? What there are a few cases, but it is controlled? Other Agents Anthrax Not contagious Can be treated with antibiotics, but it is better to start within 12 hours of exposure There is a vaccine Plague, tularemia Contagious Potential agents Treatable with antibiotics unless bioengineered Nature’s Own Flu SARS HIV and related agents Ebola Avian Flu West Nile Who knows what else? What if there is an outbreak? Do you keep the ER open? What if you people are afraid to treat patients? Do you admit potentially infected patients? What are the risks? Who pays for the costs to the hospital? What if there is not enough vaccine or antibiotics to go around? The Ethics of Plans Is it ethical to make plans that cannot be implemented? Is there a duty to speak up and say we are not ready? What happens to health care workers and government employees who say the plans will not work?