KDP poster Berlin ISPOR nov 2012
advertisement
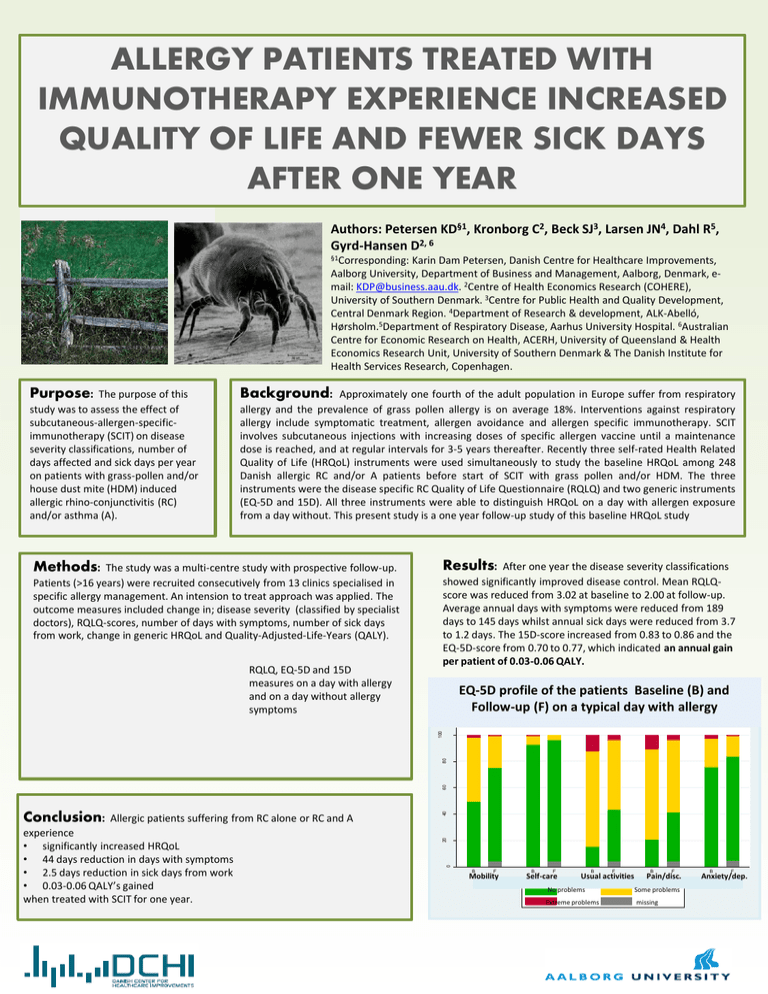
ALLERGY PATIENTS TREATED WITH IMMUNOTHERAPY EXPERIENCE INCREASED QUALITY OF LIFE AND FEWER SICK DAYS AFTER ONE YEAR Authors: Petersen KD§1, Kronborg C2, Beck SJ3, Larsen JN4, Dahl R5, Gyrd-Hansen D2, 6 §1Corresponding: Karin Dam Petersen, Danish Centre for Healthcare Improvements, Aalborg University, Department of Business and Management, Aalborg, Denmark, email: KDP@business.aau.dk. 2Centre of Health Economics Research (COHERE), University of Southern Denmark. 3Centre for Public Health and Quality Development, Central Denmark Region. 4Department of Research & development, ALK-Abelló, Hørsholm.5Department of Respiratory Disease, Aarhus University Hospital. 6Australian Centre for Economic Research on Health, ACERH, University of Queensland & Health Economics Research Unit, University of Southern Denmark & The Danish Institute for Health Services Research, Copenhagen. Purpose: The purpose of this study was to assess the effect of subcutaneous-allergen-specificimmunotherapy (SCIT) on disease severity classifications, number of days affected and sick days per year on patients with grass-pollen and/or house dust mite (HDM) induced allergic rhino-conjunctivitis (RC) and/or asthma (A). Background: Approximately one fourth of the adult population in Europe suffer from respiratory allergy and the prevalence of grass pollen allergy is on average 18%. Interventions against respiratory allergy include symptomatic treatment, allergen avoidance and allergen specific immunotherapy. SCIT involves subcutaneous injections with increasing doses of specific allergen vaccine until a maintenance dose is reached, and at regular intervals for 3-5 years thereafter. Recently three self-rated Health Related Quality of Life (HRQoL) instruments were used simultaneously to study the baseline HRQoL among 248 Danish allergic RC and/or A patients before start of SCIT with grass pollen and/or HDM. The three instruments were the disease specific RC Quality of Life Questionnaire (RQLQ) and two generic instruments (EQ-5D and 15D). All three instruments were able to distinguish HRQoL on a day with allergen exposure from a day without. This present study is a one year follow-up study of this baseline HRQoL study Methods: The study was a multi-centre study with prospective follow-up. Results: After one year the disease severity classifications Patients (>16 years) were recruited consecutively from 13 clinics specialised in specific allergy management. An intension to treat approach was applied. The outcome measures included change in; disease severity (classified by specialist doctors), RQLQ-scores, number of days with symptoms, number of sick days from work, change in generic HRQoL and Quality-Adjusted-Life-Years (QALY). showed significantly improved disease control. Mean RQLQscore was reduced from 3.02 at baseline to 2.00 at follow-up. Average annual days with symptoms were reduced from 189 days to 145 days whilst annual sick days were reduced from 3.7 to 1.2 days. The 15D-score increased from 0.83 to 0.86 and the EQ-5D-score from 0.70 to 0.77, which indicated an annual gain per patient of 0.03-0.06 QALY. RQLQ, EQ-5D and 15D measures on a day with allergy and on a day without allergy symptoms EQ-5D profile of the patients Baseline (B) and Follow-up (F) on a typical day with allergy 60 B F B F B F B F 40 F No problems Extreme problems Some problems Missing 20 experience • significantly increased HRQoL • 44 days reduction in days with symptoms • 2.5 days reduction in sick days from work • 0.03-0.06 QALY’s gained when treated with SCIT for one year. B 0 Conclusion: Allergic patients suffering from RC alone or RC and A propertion of patients 80 100 Figure 2. EQ5D profile of patients (N=210) screened to SCIT on a day with allergy, baseline (B) and followup (F) B F Mobility Mobility B F Self-care Self-care B F Usual activities Usual activities No problems No problems Extreme problems Extreme problems B F Pain/disc. Pain/discomfort Some problems Some or moderate problems Missing missing B F Anxiety/dep. Anxiety/depression