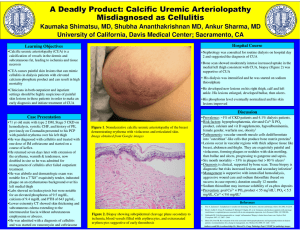
Calcific Uremic Arteriolopathy
advertisement

QuickTime™ and a d eco mpres sor are nee ded to s ee this picture. Calcific Uremic Arteriolopathy ‘Calciphylaxis’ QuickTime™ and a decompressor are needed to see this picture. David Shure Calciphylaxis Syndrome • ‘Coined by Hans Selye ‘62 • Nephrectomized rat model 1) Systemic Sensitization induced by agents i.e. PTH, vitamin D, or high Ca, P diet 2) After ‘critical period’, exposure to appropriate challengers via SC injections of iron salt, egg albumin, polymyxin, glucocorticoids, causing local trauma, led to macroscopic visible deposits of calcium salts systemically and at site of injection Calciphylaxis QuickTime™ and a decompressor are needed to see this picture. Calciphylaxis • Metastatic systemic calcifications after invasive manipulation of animal model • No vascular calcifications found CUA CUA • Occurs in presence of uremia • Abnormalities in divalent ion ie PTH, Ca, PO4 (not required) • Vascular calcifications at site of lesions CUA First Described • Early 1970’s • Cutaneous eruptions usu in pt’s on HD or after Renal Tx • Painful skin lesions with superficial violaceous nodules on tips of digits, ankles, thighs or buttocks • Progressed to hemorrhagic eruptions with ischemic necrosis • Bilaterally symmetrical, superficial, maintained persistent distal pulses • Progressed to necrosis, ischemic severe pain, gangrene Pathogenesis Unclear • Pathogenic Factors – Uremic milieu + high Ca x P – Ca content of skin noted to be high in HD pts and higher when dialysate Ca concentrations of 4.0 meq/L. Lowering dialysate Ca improved CUA in some pts. Also avoiding ca based po4 binders – Presence of high PTH levels: PTX effective in some pts CUA associated with: • Most primary renal diseases including DM • Occurs rarely in non-renal failure diseases, ie primary hyperparathyroidism and alcohol-related cirrhosis Necrotic Skin Lesions QuickTime™ and a d eco mpres sor are nee ded to s ee this picture. QuickTime™ and a decompressor are needed to see this picture. Lesion Evolution • Primary: calcium salts accumulate in media of small arteries – intima is thickened by loose CT – lumen narrows • Secondary Lesion • Infarcts of the subcut tissue and skin comprise the secondary lesions, responsible for initial clinical manifestations of the syndrome. • Before skin ulcerations, tissue ischemia leads to hard lumpy and/or plaque-like charac to the SC tissue. Secondary Lesion • Primary lesion alone not sufficient to initiate infarction ie, thrombosis or reduced perfusion contribute – Thrombi often found in primary lesios – Preexisting disturbances of coagulation are relevant to the pathogenesis: protein c/s and cryofibrinogen – Also iron dextran suggested to aggravate or initiate the secondary lesions Skin Biopsy of the Presented Pt HE Stain • Intimal Constriction • Vascular Calcification of small SC arteries and or arterioles and infarctions of adjacent subcutis and skin QuickTime™ and a decompressor are needed to see this picture. Prevalence • 1-4% of ESRD population • Increasing prevalence suspected due to incr use of vit d analogues and calcium based p04 binders, in addition to increased reporting • Whites > Blacks • Females > Males 3:1 • Obesity confers risk • Mortality: 60-80% – Sepsis from infected/necrotic skin lesions – Higher mortality in proximal dz than acral dz Prototype • Obese Middle Aged Woman on HD • Tender, lumpy, induration of subcutis over lower abd wall, upper thighs and leg • Pedal pulses remain intact • Serum Ca x P and PTH elevated • Mottled skin ulcerates, exposing necrotic SC adipose tissue • Necrosis progresses and despite intensive wound care, pt dies of sepsis Obesity • Consistent localization of secondary lesions in body areas of greatest adiposity – Women deposit more of their fat in SC than internal adipose stored – Bleyer, et al AJKD 1998 identified obesity and low serum alb as highly predictive of CUA – RR of calciphylaxis incr with incr wt Differential Diagnosis • • • • • • • Systemic Vasculitis Warfarin Necrosis Lupus Panniculitis Polyarteritis of SLE HSP Pancreatic panniculitis Weber-Christian Syndrome: panniculitis sometimes with necrotic ulcers • Acquired protein C deficiency Management • Normalization of Ca x P product with ctrl of secondary HPT • Aggressive wound care with debridement of necrotic tissue and systemic Abx therapy • PTX performed in select cases, shown not successful in most pts: Chan et al, Br Jrnl Derm 47 cases survival rate of pts who underwent PTX showed same outcomes. • CUA also described in pts after PTX. Management Cont: • HD with low dialysate Ca concentration no greater than 2.5 meq/L • Avoid Ca containing po4 binders • Local injections in adipose areas where lesions usu develop should be avoided • Other potential triggers: blood products, corticosteroids, immunosuppressant should be avoided Cutaneous Necrosis from Calcific Uremic Arteriolopathy Coates et al; AJKD, 1998 • • • • 16 Cases Reviewed 14 mortalities 13 female, 3 male All developed painful livedo reticularis lesions followed by cutaneous necrosis QuickTime™ and a decompressor are needed to see this picture. Pt Details • 7 cases experienced significant loss of body wt > 10% in 6 mths preceding development of CUA • Cause of wt loss was in assoc w/failing renal tx x 2, progressive severe CRF x 2, severe dieting x 1, combo dieting and diuretics x 1. Causes of Death • 14 mortalities – Sepsis x 6 cases – Withdrawal form HD x 3 cases – Cardiac arrest x 3 – GI hemorrhage x 2 Survivors • Cases 10 and 14 – Both w/ predominantly distal dz, had slow healing of lesions – Case 10: developed necrotic ulcers over lower ant aspect LE after trauma to LE while on warfarin for DVT – Rx: bed rest, saline soak dressings, abx, coumadin converted to LMWH – Lesions healed over 3 mths and pt followed x 18 months without recurrence Survivor Case 14 • Bilat lower limb necrosis in Aug 1992 in assoc secondary hyperparathyroidism and hypercalcemia – Rx: total PTX and split skin grafting – Pt healed and was ulcer free x 4 years Case 15 • Developed CUA while on warfarin rx for AF • Rx: substitution of LMWH for warfarin assoc with arrest of progression of CUA • During healing phase of skin lesions, pt had cardiac arrest Pathology • Small Vessel calcification and endovascular fibrosis • Panniculitis with vascular calcification • Fat necrosis and acute inflammation QuickTime™ and a decompressor are needed to see this picture. Weight Loss as a Predisposing Factor • 7/16 cases had mean wt loss 13 kg over preceding 6 mths – Rapid wt loss may be assoc w/relative intravascular volume depletion and a reduction in tissue perfusion – Previously heavily calcified vessels may be unable to relatively vasodilate to increase skin BF and ischemic areas may develop exacerbated by bed rest in turn predisposing to pressure ulcers High Prevalence of Warfarin Therapy • 8/14 cases – Only 2 pts had evidence of PVD , therefore unlikely that warfarin usage is only a marker of those pts with PVD – Fluctuating levels of protein c and s implicated in pathogenesis of ischemic tissue necrosis lesions and in addition to warfarin might predispose to formation of lesions – May be a risk factor but clear causation not proven Calciphylaxis Precipitated by UV Light in a Pt with ESRD Secondary to SLE James, et al AJKD 1998 • 39 F, ESRD due to SLE, on CAPD, p/w 3wk hx bilat thigh pain • Dx in ‘84 w/SLE and APLA after recurrent DVT and PE, on chronic prednisone, azathioprine, coumadin • Developed generalized pruritis refractory to topical agents, including steroid based creams. Dermatologist rx: phototherapy • Developed erythematous, macular rash on left thigh 2d after 2nd UV rx Skin Lesion Progression • Similar rash developed on rt thigh 2d later, w/assoc burning and hyperesthesia of both thighs • Serum calcium 8.4, albumin 3.6 • Po4 5.5, iPTH 119, INR 2.0 QuickTime™ and a decompressor are needed to see this picture. QuickTime™ and a decompressor are needed to see this picture. UV light induced CUA • CUA developed 2d after exposure to UV photoradiation • Pt had been taking warfarin for 7 years prior to skin lesions, therefore not suspected to be coumadin necrosis • Cannot r/o role of steroids and cytotoxic drugs as inciting agents for CUA • APLA induced ischemic cutaneous necrosis from recurrent arterial/venous thromboses show thrombi in small arteries/veins without medial calcification or intimal thickening did not support APLA syndrome as the cause Sodium Thiosulfate Treatment for CUA in Children and Young Adults Araya, et al JASN 2006 • IV Sodium Thiosulfate (STS) – Antioxidant and chelator of cations (e.g. Ca), initially used as antidote for Cn and cisplatin toxicity – AOX properties restore endothelial cell function and promotes VD – Enhanced aqueous solubility of Ca thiosulfate allows for successful mobilization and clearance of vascular and ST calcium deposits Methods • CUA dx histologically and confirmed w/nuclear medicine bone scan • STS 25% solution after each HD session tiwk • HD performed with high flux dialyzer Pt’s • 1: 21 white M, esrd at age of 5 mths due to bilat multicystic dysplastic kidney dz, now s/p one living-related and 2 deceased donor kidney tx. Refractory hyperPTH led to PTX • 2: 12 y/o white boy, in-utero posterior urethral valves, progressed to esrd, received tx at age 3, CVC left femoral DVT on coumadin, developed 2 hyperparathyroidism with levels 129 to 974 • 3: 21 white F with CF bilat lung tx at age 18, developed calcineurin nephrotoxicity and CRF. HD at age 20, developed SVC thrombus QuickTime™ and a decompressor are needed to see this picture. QuickTime™ and a decompressor are needed to see this picture. STS • Leads to enhanced solubility of calcium deposits in aqueous solution • Admin of STS in CUA could facilitate the mobilization of calcium from affected vessels • Animal data, demonstrate that STS distributes rapidly throughout the EC space • In RF VOD doubles and the metabolic clearance rate decreases drastically • Believed to be eliminated via biliary secretion in ESRD pt’s STS • First described benefits by Yatzidis in 1985 w/respect to rx 34 pt’s with recurrent urolithiasis and decreased rate of new stone development • In CUA, assoc with reduced pain/ inflammation, improved healing • Most dramatic reported benefit is in pain relief, usu noted within first days after initiation of Rx. It is hypothesized due to AOX properties of STS, by restoring endothelial function can enhance NO production, promoting VD and reducing pain. Long-Term IV STS in Treatment of a Pt with Calciphylaxis Brucculeri, et al 2005 Seminar In Dialysis • ESRD pt w/severe CUA • Treated for 34 months • Found measurable qty of drug more than 50 hrs after Rx, in addition to a markedly elevated t1/2 of 478 minutes MOA • Suggested: the physical properties of its more aqueous soluble calcium salt allow it to dissolve away other relatively insoluble calcium salts from supersaturated tissues • When compared to other calcium salts (sulfate, citrate, phosphate, oxalate), Ca thiosulfate is 250-100,000 times more soluble in aqueous solution. Yatzidis, 1984 • Plausible that STS admin may in essence chelate calcium from the precipitated mineral that comprises the ST deposits. • Additionally, STS appears to have AOX Pharmakokinetics STS