Health Program Evaluation: An Economic Perspective
advertisement

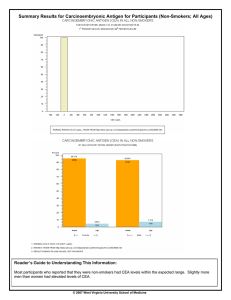
Program Evaluation from an Economic Perspective Phaedra Corso, Ph.D. Associate Professor College of Public Health University of Georgia Why Care About Economics in the Context of Prevention? Maximizing outcomes is important. Minimizing costs is important too. Resources are limited, so hard (resource allocation) decisions must be made. Demonstrates the value provided from the resources expended (return on investment). The PH Model for Prevention – Economics? Risk and Protective Factor Identification Problem Identification Economic Impact - COI Program and Policy Evaluation Program and Policy Development Economic Evaluation Implementation and Dissemination EE Methods Partial evaluation – costs only Cost of illness (COI) analysis Cost analysis (program costs) Full evaluation – costs and outcomes Cost-benefit analysis (CBA) Cost-utility analysis (CUA) Cost-effectiveness analysis (CEA) COI Analysis Estimates total costs incurred because of a disease or condition (i.e., medical costs, non-medical costs, productivity losses) Generally reported as annual total cost average per person lifetime cost Used to show potential benefits of prevention efforts Costs of Violence in the United States Corso et al., AJPM 2007 Cost Parameters Direct costs Medical care ED visits Hospitalizations Ambulance/paramedic MD visits Dental Physical Therapy Prescription Drugs Mental health care Productivity losses Work losses Household productivity losses Incidence ~2.2. million medically-treated injuries associated with violence occurred in 2000 ~17,000 homicides, ~30,000 suicides People aged 15 to 44 years comprise 44 percent of the population, but account for nearly 75 percent of violent injuries Costs The total cost associated with nonfatal injuries and deaths due to violence in 2000 was more than $70 billion. $37 billion for interpersonal violence $33 billion for self-inflicted violence The average cost per homicide was $1.3 million in lost productivity and $4,906 in medical costs. The average cost per case for a non-fatal assault resulting in hospitalization was $57,209 in lost productivity and $24,353 in medical costs. The average cost per case of suicide is $1 million lost productivity and $2,596 in medical So What? The incidence and economic burden of injuries in the US is substantial This information can be used to lobby for more prevention resources Implementation of effective interventions could reduce this burden The cost to implement effective interventions less the economic burden prevented – represents the potential returns on investment for Cost Analysis (CA) Estimates total costs of running a program Costs are the value of the resources (people, building, equipment and supplies) used to produce a good or a service Important for realizing costs from varying perspectives e.g., incurred by program, incurred by participant Includes not just financial, but also economic costs. Important for budget justification, decision Cost Analysis of a national replication of a child maltreatment program Corso et al., CDC, OCAN (in progress) Define Cost Categories **Type of Activity (D) Direct: Client-focused, face-to-face activity (I) Indirect: Collateral activities on behalf of client systems (AC) Administrative-Client: Related to client activities (AP) Administrative-Program: Related to programmatic/management activities ***Activity Description a. Advocate b. Assess c. Counseling/support d. Court representation e. Assist/provide f. Plan g. Refer h. Schedule i. Teach j. Transport a. Advocate b. Clinical documentation c. Research d. Preparation for court e. Testify in court f. Consult/Collaborate g. Locate resources h. Team meeting i. Risk management meeting j. Clinical Interdisciplinary team mtng k. I&R referral a. Gives supervision b. Receives supervision c. etc Etc. Preliminary Results at end of Year 1 The average cost per family referral ranged from $2,319 to $8,906. The average cost per family receiving services ranged from $4,238 to $33,742. At the end of the first year of implementation, pre-implementation costs as a percentage of total costs ranged from 23% to 42% of the total costs of the program. So What? Provides information for Agency X who might want to implement the program in the future. Provides the cost component of a full EE. Lessons learned on how to conduct a programmatic CA: Prospective data collection Input from site implementers Technical assistance throughout data collection Revisions of cost collection templates along the way Reference: Applying Cost Analysis to Public Health Programs (at www.phf.org) What is Economic Evaluation (EE)? Applied analytic methods to: Identify, Measure, Value, and Compare the costs and consequences of treatment* and prevention** strategies. * Done a lot ** Done “not so much” Cost-benefit Analysis - CBA A method used to compare costs and benefits of an intervention Provides a list of all costs and benefits over time: • • where all the costs and benefits are standardized or valued in monetary terms. Can have different time lines Can have different amounts at different times Provides a single value: • Net Benefits: NB (Benefits – Costs) When is CBA Used? To decide whether to implement specific programs When choosing among competing options If NB > 0, implement Implement program with highest NB For setting priorities on options given resource constraints Quantify Benefits - CBA Cost-of-Illness (COI) approach Willingness-to-Pay (WTP) or Contingent-valuation surveys • (e.g., how much is society willing to pay to reduce the annual morbidity and mortality risk associated with a disease or injury) Corso Survey (Fall 2007, Georgia) “Based on national 2 out of every 100,000 “Now we haddata, a nationally-sponsored child maltreatment “If thisimagine program were available to your state, would youchildren be willing to prevention thatper wasof available to your state and this annually, or an taxes average 4 to children every day are this killed pay $150 inprogram extra year sponsor this program?” program wasofproven reduce the riskbyofparents a child being killed due as a result child to maltreatment or caretakers.” to child maltreatment by 50%. This means that the number of YES – “Would you willingevery to pay children killed onbeaverage day$225?” in the U.S. by child NOmaltreatment – “Would youisbe willingfrom to pay $75?” reduced 4 per day to 2 per day.” Cost-utility Analysis - CUA A method used to compare costs and benefits of interventions where benefits are expressed as the number of life years saved adjusted to account for loss of quality. Combines • Length of life (survival), and • Quality of life Compares disparate outcomes in terms of utility • Quality-adjusted life years (QALYs) • Disability-adjusted life years (DALYs) Derives a ratio of cost per health outcome • $/QALY or $/DALY When is CUA Used? When quality of life is the important outcome. When the program affects both morbidity and mortality. When the programs being compared have a wide range of different outcomes. When the program is being compared with a program that has already been evaluated using CUA. Quantify Benefits - CUA Utilities are: • A “preference-based” measure of health, that relies on choice and uncertainty to elicit preferences • Typically based on a 0 (death) to 1 (perfect health) scale Example of Tool to Elicit Utilities: Time Trade-Off (TTO) Quality of Life Which life do you prefer? Short and fun Long and dull Length of Life Example: TTO Utility healthy U(healthy) = 1.0 blind both eyes U (blind both eyes) = ? Dead 0 Years 12 20 Combining Quality of Life with Length of Life Utility without prevention with prevention 1.0 0.7 0 30 QALYS (with prevention) QALYS (without prevention) 75 = 1.0*75 = 75 = 0.7*30 = 21 Years Cost-effectiveness Analysis - CEA Estimates costs and outcomes of interventions Expresses outcomes in natural units e.g., cases prevented, lives saved Compares results with other interventions affecting the same outcome Summary measure: cost-effectiveness ratio Cost per some outcome achieved e.g., cost per case prevented, cost per life saved When is CEA Used? Used to identify • most cost-effective strategy from options that produce a common effect • practices that are not “worth” their costs Used for empirical support for under-funded programs Quantify Outcomes – CEA of parenting intervention Intermediate outcomes • • • Increased child self-esteem and mental health status Increased family cohesiveness/coping skills Decreased depression in parents Final outcomes • QOL improvements in parents and children CEA Caveat Outcomes cannot be combined, so one or two of the most important effectiveness measures should be considered (separately) for the CEA. The number of summary measures depends on the number of outcomes chosen. If 2 outcomes, A and B, are considered the most important for evaluation, then Cost/outcome A Cost/outcome B This makes translation for policy makers difficult!! Example: CM Prevention Program Average CE Ratios for depressive symptoms Program Baseline Ending score score 3-mo. 22.7 18.7 Difference Program Avg. CE cost Ratio* 4 $984 $246 9-mo. 8.3 $2,304 $278 21.1 12.8 * Compared to baseline Final Comments Economic evaluation (EE) is valuable to decision making and for setting health policy. For new researchers in PH, this is an important specialization to consider – because the demand for these skills is growing. Coming soon….. Center for Economic Evaluation Institute for Behavioral Research and College of Public Health pcorso@uga.edu