Protozoa
advertisement

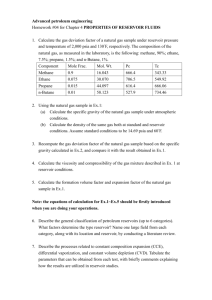
MEDICAL PARASITOLOGY Protozoa and Helminths INFORMATION EMPHASIS • Agent ID and general importance • Epidemiology (transmission, distribution, etc) • Agent damage capability • Diagnostics • Control BASIC TERMINOLOGY AND PRINCIPLES • Symbiosis: Living together • Commensalism: One symbiont benefits, other unaffected • Mutualism: Both symbionts benefit • Parasitism: One symbiont benefits, other is damaged COMMON TERMS • • • • • • • • Obligate/Facultative Parasites Endo/Ecto Parasites Pseudo/Spurious Parasites Zoonotic Parasites Host-specific/Non-specific Parasites Definitive/Intermediate Hosts Paratenic/Transfer Hosts Vector Hosts SURVIVAL FACTS AND FUNCTIONS • Parasites adapt to every niche in a host • Best adapted are least pathogenic • Parasite-host relationship is typically longterm/chronic/ “intimate” CONDITIONS REQUIRED FOR ENDEMIC PARASITISM • Reservoir of Infection • Means of Transmission to Susceptible Hosts • Ability to Invade and Establish in New Hosts • Ability to Reproduce PROTOZOAN TERMINOLOGY • Trophozoite: Active, vegetative LC stage • Cysts: Protective LC stage -Common cyst -Oocyst, sporocyst, sarcocyst, pseudocyst, etc • Cilia: Ciliate motility organelles • Flagella: Flagellate motility organelles • Pseudopod: Amoeba motility organelles • Macronucleus: Ciliate body function control • Axostyle: Flagellate “skeletal” rod • Peristome: Funnel leading to cytostome/mouth CILIATE PARASITE Balantidium coli Trophozoite Cytostome Macronucleus Cilia Cyst Macronucleus Ciliate parasite, continued • Balantidium coli Cyst transmission (fecal oral) Pathogenic in humans, mucosal erosion Frank blood in feces, sloughed mucosa Reservoir hosts swine, probably other Potential for serious damage high Prevalence overall, low Diagnosis: fecal analysis for cysts, trophs, proctoscopy for lesions/biopsy Treatment: oxytet; metronidazole; natural, spontaneous clearance occasionally Balantidium coli Life Cycle FLAGELLATE PARASITES AND COMMENSALS Trichomonads and Dientamoeba fragilis Trophozoites only Flagella Nucleus/nuclei Body shape & size Flagellates, continued Trichomonas tenax Trophozoite transmission-direct oral Mouth inhabitant, oral hygiene factor Nonpathogenic, thrives in bad conditions Reservoir unknown, probably wide Considered classically commensalistic Prevalence data spotty Diagnosis by culture, microscopic exam of oral fluids/scrapings Eliminated by good oral hygiene Pentatrichomonas hominis, Dientamoeba fragilis Transmission direct-oral, no cysts (you tell me) Colon/caecum inhabitants Non-pathogenic Reservoir unknown, probably wide Considered commensalistic (D. fragilis ???) Prevalence unknown Diagnosis usually incidental-fecal smear-stain, wet mounts + microscopy Treatment: incidental elimination-Flagyl, et.al. Dientamoeba fragilis Life Cycle Flagellate, continued Trichomonas vaginalis Transmitted by sexual intercourse Induces vaginal pH change, erosion of normal mucosa in women Vaginal itching, burning, yellow discharge in women, occasional urethritis, prostate swelling in men Human reservoir, zoonotic potential ?? Prevalence varies with population & culture Diagnosis by visual features, microscopy Treatment usually Flagyl Trichomonas vaginalis Life Cycle Flagellate Parasites and Commensals Chilomastix mesnili Enteromonas hominis, Retortamonas intestinalis, Giardia lamblia, et.al. Trophozoites Cysts Nuclei Nuclei Flagella Size & shape Size & shape Flagellates, continued Chilomastix mesnili, Enteromonas sp., Retortamonas sp.,, others Caecum/colon inhabitants Transmission by cyst or trophozoite Nonpathogenic, commensalistic Thrive in most diarrheic conditions Reservoir pool (probably) wide, unknown Widespread, sanitation dependent Diagnosis: microscopic fecal exam Treatment: unnecessary in most cases, Flagyl will work Flagellates, continued Giardia lamblia, etc Cyst transmission Pathogenic potential individually inconsistent Clinical signs variable Diarrhea/dysentery, periodic or steady Gas production Borborygmus Anorexia Skin rash Fibromyalgia Spontaneous lactose intolerance Fatigue, mild/severe Other Flagellates, continued Giardia, continued Reservoir hosts: almost any mammal Damage potential: individual factors Immunocompetence of host Natural, undefined host tolerance level Other (fuzzy factors) Worldwide distribution, sanitation dependent Diagnosis: fecal ELISA, direct microscopic exam for cysts/trophs Treatment: Atabrine, Flagyl, other Giardia Life Cycle Flagellates, continued HAEMOFLAGELLATES Trypanosomes/ trypomastigote forms Leishmanias/ amastigote forms Haemoflagellates, continued Trypanosoma brucei complex, T.b. gambiense, T.b. rhodesiense, others Vector transmission, Tse tse flies Pathogenic, terminal ‘sleeping sickness’, East African SS less acute than West African SS Signs: swollen cervical lymph nodes, fever, rashes, headache, malaise, nausea, eventually coma Various wild/domestic animal reservoirs West African much more acute and severe than East African SS. Haemoflagellates, continued Trypanosoma brucei complex, continued T.b. gambiense in West Africa, overlaps with endemic East African T.b. rhodesiense in center of continent Microscopy of concentrated or cultured blood or fluid aspirates, RES biopsy normal diagnostic methods Treatment: melarsoprol complex, suramin Trypanosoma brucei complex, LC Haemoflagellates, continued Trypanosoma cruzi American trypanosomiasis, Chaga’s disease Vector/direct contact transmission; triatomids, several species Highly pathogenic late-term/chronic Symptoms vary: fever; edema; swelling of thyroid, spleen, liver, various lymph nodes; CNS re mental impairment, coma; tachycardia, weakness, chest pain, anemia, megacolon, megaesophagus, other, depending on organism strain, length of infection, condition of host, etc. Haemoflagellates, continue T. cruzi, continued Reservoir large, many carnivore, omnivore & herbivore species Damage severe, early (fulminating) or late (chronic), depends on various factors Prevalence < 3% to > 50% in endemic areas from southcentral USA to southern SA Diagnosis: cell/fluid culture, xenodiagnosis, direct microscopy Treatment: no reliable/curative; nifurtimox, primaquine & related drugs reduce but do not eliminate blood stage, nothing effective X cellular stage T.cruzi, continued Triatomid Vector Trypomastigote/ Trypanosome Haemoflagellates, continued T. Cruzi life cycle Haemoflagellates, continued Leishmania topica complex, L.t. mexicana complex, L.t. braziliense complex, et.al. Vector trans. by sand flies Superficial to extensive, shallow to deep Cutaneous lesions, vary by strain/species Oriental sore: limited, wet ulcer Chiclero ulcer: ear ‘notches’ Diffuse cutaneous: dry, diffuse Mucocutaneous: cartilage erosion Reservoir: large; many native carnivore, omnivore, herbivore vertebrates Haemolagellates, continued Leishmania tropica complex, continued Lesion severity varies with species/strain, simple limited wet/dry to severe erosion Widespread in tropical, subtropical & warm temperate regions worldwide Lesion appearance is diagnostic, agents can be cultured or viewed microscopically Pentavalent antimony compound treatment, with/without amphotericin B Haemoflagellates, continued Leishmania donovoni complex Vector transmission, sandflies Visceral, reticulo-endothelial system inhabitation, often lethal Fevers (variable), anemia, hepatomegaly splenomegaly, ascites, Kala-azar (blackening of facial skin), et.al. Reservoir: domestic & wild vetebrates Damage potential varies with species/strains Distributed widely, tropics, subtropics, warm temperate and cool temperate regions Diagnosis by serology, culture of blood or biopsy Antimony, amphotericin-B, allopurinol treatments Leishmania sp. life cycle Sarcodina AMOEBIC PARASITES AND COMMENSALS Entamoeba gingivalis Trophozoite only, inhabits oral cavity Transmitted directly (no cyst) Commensalistic, considered nonpathogenic Host reservoir: dogs, cats, monkeys, other? Patho potential considered 0/low Distribution undefined, prevalence 70-90% of “unhealthy”, 7-35% of “healthy” mouths surveyed Diagnosis: microscopy of tissue/scraping/fluid Treatment: improve oral hygiene; probably Flagyl Sarcodines, continued Amebic parasites and commensals, continued Entamoeba histolytica Trophozoite in caecum/colon, if invasive may inhabit liver, lungs, other tissues; Cysts (infective stage) form in normal stools Pathology variable: noninvasive; if invasive, ulcerates colonic mucosa, spreads to liver, lung, et.al., produces abcesses; path potential indicated by colony site Reservoir includes monkeys, dogs, pigs, et.al. Distribution worldwide: tropical, subtropical, warm temperate areas; sanitation dependent Sarcondines, continued E. histolytica, continued Prevalence rated second to Giardia worldly Diagnosis by microscopic ID of trophs, cysts in feces, trophs in tissue-based abcesses Treated with Flagyl (metronidazol), various Emetine formulations, Diiodohydroxyquin, et.al. Entamoeba histolytica Cyst Trophozoite Amoeba sp. life cycle Sarcodines, continued Entamoeba coli, E. hartmanni, E. dispar, E. sp.(unnamed), Endolimax nana, Iodamoeba butschlii, a few others Caecum/colon inhabitants, transmitted by cysts, All commensals (with rare exceptions) Diarrhea enhances production of trophs Reservoir: various vertebrate animals Damage potential 0/low (some exceptions?) Prevalence high, world-wide warm areas Diagnosis: microscopic ID in feces Treatment considered unnecessary Entamoeba coli Cyst Trophozoite Sporozoa/apicomplexa SPOROZOA/APICOMPLEXA TERMINOLOGY Sporogony: basic life cycle stage; sporozoite generation Schizogony/merogony: basic life cycle stage; (asexual repro) merozoite generation Gametogony/gamogony: basic life cycle stage; (sexual repro) gametocyte generation Oocyst: cyst produced in sporogony Sporocyst: cyst within oocyst, produced in sporogony Sporozoite: basic infective unit in oocysts/sporocysts Sporozoa, continued Sporozoan terminology, continued Trophozoite: transitional zoite, between sporozoite and schizont/merozoite Merozoite: basic zoite product of schizogony Tachyzoite: rapidly replicating merozoite Bradyzoite: slowly replicating merozoite Sarcocyst: end-stage schizont in intermediate host with Sarcocystis sp. infection Pseudocyst: end-stage schizont in intermediate host with Toxoplasma gondii infection Sporozoa, continued Sporozoa, continued Basic Life Cycle Stages Sporogony: formation of sporocysts and sporozoites Schizogony/merogony: formation of merozoites/tachyzoites/bradyzoites Gamogony/gametogony: formation of gametocytes and gametes Sporozoa, continued Isospora belli Transmission direct, fecal oral, via oocysts Pathogenic potential low, non-bloody diarrhea common in immunodeficient hosts, uncommon in others Clinical signs absent, except in rare cases Reservoir limited to humans, other anthropoids, strongly host-specific Damage low, destroys superficial mucosal cells Prevalence world-wide, sanitation dependent Diagnosis by microscopic ID of oocysts in fecal flotation Treatment usually unnecessary, pyrimethamine + a sulfa, trimethoprim, when needed Isospora sp. life cycle Sporozoa, continued Cyclospora cayetanensis Transmission direct fecal-oral, via oocysts Pathogenic potential low/moderate, non-bloody diarrhea in sporadic cases, most severe in immunodeficient individuals Diarrhea ~3 weeks in “healthy” hosts, longer/much longer in immonodeficient; can be cyclic, recurrent; long-term may + anorexia, fatigue, weight loss, fever Reservoir hosts: reptiles, rodents, insectivores, probably other domestic & wild animals; species ID is incomplete in host animals Sporzoa, continued C. cayetanensis, continued Damage: jujunal villous atrophy, crypt hyperplasia, inflammation Prevalence spotty, outbreaks in New Guinea, Nepal, Peru, Chicago, Canada, other Diagnosis: microscopic ID of oocysts from fresh feces, acid-fast-stained smears, fluorescent Ab-stain preps Treatment: trimethoprim + sulfamethoxazole Cyclospora sp. life cycle Sporozoa, continued Cryptosporidium parvum Transmission direct, fecal-oral, via oocysts Pathogenic potential variable: low in “healthy”, moderate/high in “deficient” hosts, depending on immunocompetence level Clinical signs: non-bloody diarrhea/dysentery, mild/short-term (~2 weeks) to severe/longterm (steady or recurrent) Reservoir: complete spectrum unknown, but many domestic animals are known Damage potential and mechanisms vary with hosts & species, poorly understood Sporozoa, continued C. parvum, continued Prevalence world-wide, sanitation dependent, Diagnosis: microscopic ID of oocysts in feces by flotation, acid-fast or immunofluorescent staining; histologic or immunohistologic exam of biopsy of intestinal mucosa Treatment: paramomycin may be suppressive in specific cases, not curative (no curative medication known) Cryptosporidium sp. life cycle Sporozoa, continued Sarcocystis bovihominis, S. suihominis, probably others Transmission: ingestion of beef or pork (or other), uncooked/undercooked, containing sarcocysts in muscle fibers Pathogenic potential low in human DH Clinical signs absent except in rare cases Reservoir limited to human DH (+ possibly other anthropoids), and bovine/porcine IHs Damage low in human DH, inconsequential erosion of intestinal mucosa Sporozoa, continued S. bovihominis, S. suihominis, etc. continued Prevalence world-wide, determined by cultural food prep and consumption factors Diagnosis: microscopic ID of oocysts and/or sporocysts in feces No treatment identified: trimethoprim + sulfamethoxazol probably suppressive Sporozoa, continued Sarcocystis lindemanni Transmission by ingestion of sporocysts from unknown DHs in fecal contamination Pathogenic potential unknown Clinical signs unknown Reservoir unknown Damage potential unknown Prevalence unknown, probably sanitation dependent Diagnosis: histologic examination of muscle Treatment unknown Sarcocystis species Life Cycle Sporozoa, continued Toxoplasma gondii Transmission direct via oocysts (fecal-oral), ingestion of infected meat, transplacental, nursing, organ transplantation, et.al. Pathogenicity moderate to high, depending on strain, host “health” factors Clinical signs: Acute infection; range from unnoticeable to severe flu-like (chills, fever, headache, fatigue, lymphoid pain & swelling) Transplacental; death & abortion, various encephalomyelitis, megacephaly, microcephaly, blindness, deafness Sporozoa, continued T. gondii, continued Reservoir enormous: nearly all warm-blooded vertebrates including birds, suitability varied Damage potential dependent on strain, host susceptibility, host “health” condition Prevalence variable, depending on association with feline DHs, and food (meat) preference & preparation Diagnosis: Indirect; fluorescent Ab, latex aggl., serum ELISA, other serotests. Direct; culture of body fluids & tissue samples, immunohistochemistry, histopathology Treatment: Pyrimethamine + a pyrimidine Toxoplasma gondii life cycle Sporozoa, continued Plasmodium vivax Transmission: female Anopheles mosquito vector, blood transfusion Pathogenicity high, especially in 1st infections, moderate/high in subsequent infections and relapses, depending on host condition Symptomatics: ~12-20 day prepatency (no signs); prodroma (influenza-like; headache, nausea, vomiting, anorexia, muscle aches); sudden,severe shock-like chill (paroxysm), fever cycle quickly stabilizing at ~48 hr, continuous for 3-10 weeks; recrudescences/relapses for 5-8 years Reservoir: humans, monkeys, apes, Anopheles vector Sporozoa,continued P. vivax, continued Damage: extensive hemolysis, production of toxic parasite metabolites Prevalence: world-wide tropical and sub-tropical less common in warm temperate regions Diagnosis: microscopic ID/differentiation of species by microscopic exam of stained smears of blood properly collected and prepared Treatment: Quinine & related alkaloids, at least 15 additional, used or in trial, singly or in combination, efficacy variable Plasmodium sp. life cycle Sporozoa, continued Plasmodium ovale All factors involving this species are nearly identical to those listed for P. vivax, except for severity of damage, symptoms, prevalence and duration of infection. Damage potential: low/moderate, primary erythrocytic cycle ~2-3 weeks, total duration of infection ~1-2 years Symptoms: similar to P. vivax but less severe, same fever cycle periodicity Prevalence: widespread tropical & subtropical Treatment: same as for P. vivax, et.al. Sporozoa, continued Plasmodium malariae Transmission as described for P. vivax Pathogenic potential high re: hemolysis and CNS involvement late in infection Symptoms similar to P. vivax & P ovale, with longer fever cycle periodicity (72 hr), 3-24 weeks primary duration, 20-50 years duration of untreated infection with probability of recrudescence Reservoir as described for P. vivax, P. ovale Damage high; anemia, CNS & kidney syndrome Sporozoa, continued P. malariae, continued Prevalence more common in subtropical and warm temperate regions than tropical, but endemic where other species occur Diagnosis as described for P. vivax & P. ovale Treatment as described for P. vivax & P. ovale Sporozoa, continued Plasmodium falciparum Transmission as described for P. vivax, et.al. Pathogenic potential highest of all Plasmodium species, most likely of all to kill IH (human) Clinical signs similar to those described: shorter (8-11 days) incubation period, prodroma similar but mild, cycle periodicity ~ 48hr, initial paroxysm severe & long (16-36hr), 2-3 week duration of primary attack, 6-17 months duration of untreated infection Reservoir: humans, monkeys, apes, Anopheles mosquito vector Sporozoa, continued P. falciparum, continued Damage as described: hemolysis, etc., but also causes cytoadherence to endothelium of damaged and intact parasitized cells and cellular debris; all organs (brain, kidneys, liver, etc.) are affected Prevalence world-wide, but confined to tropics and subtropics Treatment as described for other species Spoorozoa, continued Babesia spp. (B. microti, B. divergens, B. gibsoni) Transmission by vector ixodid tick DHs Pathogenic potential high in splenectomized and other immunocompromised humans, may be mild or serious in intact hosts, species/strain differences are known Clinical signs: malaise, headache, fever, chills, swetting, fatigue, weakness, anemia, jaundice, renal failure Reservoir: rodents, livestock, other “natural” hosts, humans appear to be accidentals Damage high in immunodeficient, moderate in most others; much depends on species/strain of agent involved Sporozoa,continued Babesia spp., continued Prevalence widespread in “natural” reservoir hosts, spotty in humans: Europe, NE USA, Texas, Mexico, NC USA, et.al. Diagnosis: microscopic ID and differentiation from malarial (Plasmodium sp.) agents Treatment: oral quinine + IV clindamycin, a few others, less efficacious Babesia sp. life cycle