Vessels
advertisement

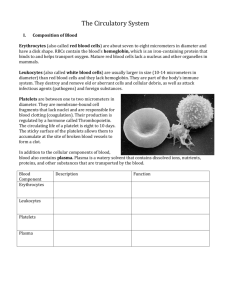
Blood Vessels Chapter 19 Blood Vessels Arteries – carry blood away from the heart • “branch” and “supply” Veins – carry blood toward the heart • “merge” and “drain” Lumen – the hollow space that carries the blood Figure 19.1 Blood Vessels Vessel Histology: • Arteries have a thicker wall and a rounder lumen • Veins have thinner walls and a larger, slit-like lumen • Arteries and veins often run side-by-side Figure 19.1a Blood Vessels Vessel Tunics: -The 3 layers of a vessel wall 1.Tunica Intima – innermost layer with simple squamous endothelium and its underlying connective tissue 2.Tunica Media – middle layer of smooth muscle (thickest in arteries) Vasoconstriction – shrinks lumen Vasodilation – enlarges lumen 3.Tunica Externa – outer layer of connective tissue for support, with nerve fibers and small vessels (thickest in veins) Vasa vasorum – series of small vessels bringing blood to large vessel walls Figure 19.1b Blood Vessels Types of Arteries: Elastic arteries • aorta and its branches • D = 1.0 - 2.5cm • highly elastic, act as pressure reservoirs Muscular arteries • vessels supplying muscles/organs • D = 0.3mm – 1.0cm • thick media to regulate blood flow Arterioles – • smallest arteries • D = 10µm – 0.3mm • # of tunics varies with size • regulate blood supply to capillary beds Figure 19.2 Blood Vessels Types of Veins: Venules – • smallest of the veins • D = 8 – 100 µm • Drain blood from capillary beds • # of tunics varies with size Veins – • D = 0.1mm – 2.5 cm • have all three tunics • act as blood reservoirs, holding 60-65% of blood at any time • pressure is low, need valves Venous Sinuses – large flat veins that are not true vessels, supported by the surrounding tissues, not tunics Figure 19.2 Capillaries Capillaries: • smallest vessels, allow exchange of solutes with tissues • pericytes – muscle-like cells for support • only 1 tunic, intima • D = 8 – 10 µm • Length = 1mm 3 type of Capillaries: 1.Continuous 2.Fenestrated 3.Sinusoid Figure 19.3 Capillaries 3 type of Capillaries: 1. Continuous: • most common type, found in muscle and skin • wall has continuous sheet of endothelial cells • Intercellular clefts – small gaps between endothelial cells allowing some fluid and solute movement Figure 19.3a Capillaries 3 type of Capillaries: 2. Fenestrated: • found in kidneys, small intestine, and endocrine glands • small holes, fenestrations, make these vessels highly permeable • used for filtration and absorption Figure 19.3b Capillaries 3 type of Capillaries: 3. Sinusoid: • found in the liver, bone marrow and lymph tissues • large lumens, large fenestrations, and large intercellular clefts • Highly permeable to fluids, solutes and even cells! Figure 19.3c Capillaries Capillary bed – an interweaving network of 10-100 capillaries from arteriole to venule, performing ‘microcirculation’ • Vascular shunt – allows blood to bypass a bed • True capillaries – the many vessels for gas and nutrient exchange • Precapillary sphincters – regulate blood flow into the true capillaries based on local tissue needs Figure 19.4 Physiology of Circulation Note: Blood moves down its pressure gradient (high to low) • Blood flow – the volume of blood passing through a vessel in a given amount of time, expressed as mL/min • Blood pressure – the force exerted by blood on a vessel wall, measured in mmHg. Typically represents pressure in a large artery. • Resistance – the friction encountered by the blood, reducing flow. Caused by 3 main factors: 1. Blood viscosity – thicker blood, as in polycythemia, experiences more resistance 2. Blood vessel length (total) – additional pounds of adipose adds miles of vessels to the body, increasing resistance 3. Blood vessel diameter – blood in smaller vessels experiences more resistance • Formula : Flow = ∆P/R Blood Pressure Arterial blood pressure – the pulsatile pressure resulting from heart contraction and relaxation • Systolic pressure – the peak pressure caused by heart contractions (av. = 120 mmHg) • Diastolic pressure – the low pressure resulting from heart relaxation (av. = 80 mmHg) • Pulse pressure – the difference between systolic and diastolic pressures, causing a pulse in an artery. This P dissipates at the end of the arterial system Figure 19.5 Blood Pressure Mean arterial pressure – the average pressure in a vessel that drives blood movement. Decreases from aorta to R. atrium Formula: MAP = diastolic P + (pulse P/3) If P = 120/80… MAP = 80mmHg + (40mmHg/3) MAP = 93mmHg MAP in… Arterioles - 80-35 mmHg Capillaries – 35-15 mmHg Veins – 15-0 mmHg Figure 19.5 Blood Pressure in Veins Low venous pressure requires the following adaptations: • Large lumens – decreases resistance • Venous valves – catch blood similar to semilunar valves • Respiratory ‘pump’ – the rising and falling of thoracic pressure squeezes veins and propels blood • Muscular ‘pump’ – skeletal muscle movements squeeze veins and propels blood • Venous smooth muscle – contracts in fight-or-flight responses to propel blood Figure 19.6 Regulating Blood Pressure Blood Pressure Regulation: 1. Short Term – done by the CNS and hormones • Make changes in cardiac output or peripheral resistance, via changes in heart rate, stroke volume, and vessel diameter (increased CO and PR means higher pressure) 2. Long term – done by the kidneys • Done by making changes to blood volume (increased volume means higher pressure) Figure 19.7 Regulating Blood Pressure Neural Regulation: Baroreceptors – stretch receptors in large arteries that measure pressure When pressure rises… 1. Stretch of baroreceptors sends impulse to medulla 2. Medulla slows heart rate and dilates arteries, lowering the pressure When pressure falls… 1. Baroreceptor inactivity sends impulse to medulla 2. Medulla increases heart rate and constricts arteries, raisin the pressure Figure 19.8 Regulating Blood Pressure Hormonal Regulation: 1. Adrenal medulla hormones – norepinephrine and epinephrine are released to aide the fight-or-flight response. These trigger vasoconstriction and increased CO, therefore increasing pressure 2. Atrial natriuretic peptide – hormone from heart’s atria that causes vasodilation and a decrease in blood volume by increasing urine output, thereby decreasing pressure 3. Antidiuretic Hormone – hormone from hypothalamus that increases blood volume by decreasing urine output, therefore increasing pressure 4. Angiotensin II – a kidney hormone that causes vasoconstriction, thereby increasing pressure Regulating Blood Pressure Renal Regulation (Long term): 1. Direct mechanism – does not use hormones • Increased pressure means increased kidney filtration and urine output, lowering blood volume and pressure • Lower pressure means decreased filtration and urine output, raising blood volume and pressure 2. Indirect mechanism – uses hormones to affect blood volume • Called the Renin-Angiotensin mechanism Figure 19.9 Regulating Blood Pressure Renin-Angiotensin mechanism • Decreased pressure causes kidneys to release the hormone Renin, which triggers Angiotensin II production • Angiotensin II causes vasoconstriction and aldosterone release from the adrenal glands • Aldosterone causes sodium retention which causes water retention, increasing blood volume • Increased blood volume increases blood pressure Figure 19.9 Regulating Blood Pressure Figure 19.10 Pulse Pulse – a wave of stretch and recoil of an artery due to the rising and falling of arterial pressure • Pressure/Pulse points – locations where major arteries are superficial and easily felt Figure 19.11 Measuring Blood Pressure Ausculatory method – measures blood pressure by listening to sounds in the vessel. Needs cuff to constrict the vessel, pressure gauge to measure, and stethoscope to listen. 1. Inflate cuff to a pressure greater than systolic to collapse vessel = no flow 2. Slowly release air from cuff until sounds are heard = turbulent flow. The reading on the gauge is now the systolic pressure 3. Continue releasing air until sounds dissipate to nothing = laminar flow. The reading on the gauge is now the diastolic pressure Measuring Blood Pressure Healthy blood pressure = 120/80 mmHg Hypotension • Low blood pressure, systolic P < 100 mmHg • Can be due to good fitness, or malnutrition causing low blood viscosity Hypertension • High blood pressure, 140/90 mmHg or above • Causes include diet, obesity, age, diabetes, heredity, stress, smoking • Can lead to heart failure, renal failure, stroke, enlarged myocardium, etc. Regulating Blood Flow Tissue perfusion – blood flow through tissues for nutrient delivery, gas exchange, absorption, or filtration. Blood distribution – at rest, large volumes of blood are sent to the kidneys and abdominal organs. During exercise, large volumes of blood are sent to skeletal muscles and skin Figure 19.12 Regulating Blood Flow Autoregulation – the automatic adjustment of blood flow through a tissue based on that tissue’s need. Can be regulated metabolically or myogenically. • Metabolic control – decreased O2, increased CO2, and decreased nutrient levels trigger local vasodilation of arterioles, supplying more blood to local capillary beds • Myogenic control – increased stretch of arterioles triggers their vasoconstriction, thereby protecting the fragile capillaries. Decreased stretch of arterioles triggers their vasodilation. Autoregulation in specific organs: • Skeletal muscle – major increase in blood flow during activity, called exercise hyperemia. Largely triggered by low O2 and high waste levels • Skin – besides normal metabolic and myogenic controls, increased body temperature causes vasodilation here. WHY? • Lungs – areas of lung tissue with low O2 levels triggers local vasoconstriction, while lung tissue with high O2 levels triggers local vasodilation. WHY? Capillary Dynamics Capillary Exchange – movement into or out of capillaries occurs 4 different ways 1. Diffusion – direct movement of lipid-soluble molecules through the endothelial cells 2. Intercellular clefts – movement of water-soluble molecules between endothelial cells 3. Fenestrations – movement of water-soluble molecules through endothelial holes 4. Vesicular Transport – movement of large molecules by vesicles Figure 19.15 Capillary Dynamics Bulk flow – the leakage of plasma out of, then back into a capillary, based on the balance of pressures Hydrostatic pressure – the pressure of a fluid on a vessel wall (same as blood pressure) Colloid osmotic pressure – the pressure generated by nondiffusable solutes tendency to draw water towards themselves Figure 19.16 Capillary Dynamics Net Filtration Pressure (NFP) – the pressure generated by the balance between hydrostatic and colloid osmotic pressures • NFP is a positive pressure at the arterial end of a capillary bed, forcing plasma to leak into the surrounding tissue • NFP is a negative value at the venous end of a capillary bed, drawing plasma back into the vessels Figure 19.16