Chapter 40 Environmental Emergencies 40-1
advertisement
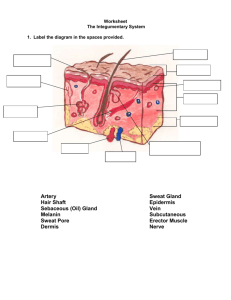
Chapter 40 Environmental Emergencies Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 40-1 Objectives 40-2 Body Temperature • Balance between heat produced and heat lost • Measured in degrees • Core temperature • Peripheral (surface) temperature 40-3 Temperature Regulation • Skin – Sensors detect changes in temperature • Hypothalamus – Located in the brain – Functions as the body’s thermostat 40-4 Temperature Regulation • When high temperatures are sensed: – Blood vessels in the skin widen (dilate) 40-5 Temperature Regulation • When low temperatures are sensed: – Blood vessels in the skin narrow (constrict) – Sweating stops – Major body muscles shiver to increase heat 40-6 Heat Production • Heat is mainly produced by: – Converting food to energy (metabolism) – Increasing skeletal muscle activity 40-7 Heat Loss 40-8 Radiation • Transfer of heat from one object to another without contact between the two objects • Example: – Heat from the sun 40-9 Convection • Transfer of heat by the movement of air or water current 40-10 Conduction • Transfer of heat between objects that are in direct contact • Amount of heat lost depends on: – Temperature difference between the body and the object – Amount of time the body and the objects are in contact – Amount (surface area) of the body in contact with the object 40-11 Evaporation • Loss of heat by vaporization of moisture on the body surface – Body heat is lost if the skin temperature is higher than the surrounding temperature – Body heat is gained if the surrounding air temperature is higher than the body temperature 40-12 Respiration • Small amount of heat is lost through the evaporation of moisture within the lungs 40-13 Mechanisms of Heat Loss • Peripheral blood vessels dilate • Blood flow to body surface increases • Heat escapes from the skin surface by radiation and conduction • When air currents pass across the skin, heat is lost by convection • Sweating allows heat loss through evaporation 40-14 Types of Cold Emergencies 40-15 Types of Cold Emergencies • Two main types of cold emergencies: – Generalized cold emergency • Generalized hypothermia – Local cold injury • Damage to a specific area of the body 40-16 Hypothermia • Core body temperature of less than 95°F (35°C) • Three stages: 1. Mild hypothermia (core body temperature 93.2° to 96.8°F, or 34.0° to 37.0°C) 2. Moderate hypothermia (86.0° to 93.1°F, or 30.0° to 33.9°C) 3. Severe hypothermia (less than 86°F, or less than 30.0°C) 40-17 Hypothermia • Can occur even in warm weather • Can occur when the body loses its ability to maintain a normal body temperature 40-18 Factors Contributing to Hypothermia • Ambient temperature, wind speed, moisture • Prolonged exposure to a cool environment • Activity level of victim • Immersion in water • Improper, inadequate, or wet clothing • Low body weight • Poor physical condition • Low blood sugar • Alcohol/drug ingestion • Extremes in age (very young children, older adults) • Impaired judgment due to mental illness or Alzheimer's disease • Preexisting illness or injury • Suicide • Previous cold exposure 40-19 Scene Size-Up • Signs of exposure may be obvious or subtle • Signs of a subtle exposure include: – Alcohol ingestion – Underlying illness – Overdose or poisoning – Major trauma – Outdoor recreation – Decreased room temperature 40-20 Scene Size-Up • Remove the patient from the environment – Use trained rescuers when necessary 40-21 Primary Survey • • • • Form a general impression Move the patient to a warm location Remove any cold or wet clothing Protect the patient from the environment • Cover the patient to preserve body heat • Stabilize the patient’s spine if needed 40-22 Primary Survey • Assess: – Mental status – Airway – Breathing – Circulation 40-23 Vital Signs • Breathing – Initially increased – Then slow and shallow – Finally, absent • Heart rate – Initially increased – Then slow and irregular – Finally, absent • Skin – Initially red – Then pale – Then blue – Finally, gray, hard, and cold to the touch 40-24 Motor and Sensory Functions • • • • • Joint aches Muscle stiffness Lack of coordination Staggering walk Shivering usually present initially – May decrease until it is absent 40-25 Mild Hypothermia • • • • • • • Increased heart rate Increased respiratory rate Cool skin Shivering Difficulty talking, slurred speech Difficulty moving Memory lapse (amnesia), mood changes, combative attitude • Joint aches, muscle stiffness • Altered mental status, confusion, or poor judgment 40-26 Moderate Hypothermia • Shivering that may gradually decrease and become absent • Decreasing heart rate and respiratory rate • Irregular heart rate • Pale, blue (cyanotic), or mottled skin • Progressive loss of responsiveness • Dilated pupils • Blood pressure that is difficult to obtain 40-27 Severe Hypothermia • Irrational attitude that changes to unresponsiveness • Rigid muscles • Cold skin • Blue or mottled skin • Slow or absent breathing • Slowly responding pupils • Slow, irregular, or absent heart rate • A pulse that is hard to feel or absent • Low to absent blood pressure • Cardiopulmonary arrest 40-28 History • Obtain SAMPLE history • Ask the following questions: – How long has the patient been exposed to the cold? – What was the source of the cold (water, snow)? – If exposed to water, approximate water temperature? – What was the patient doing when his symptoms began? 40-29 Emergency Care for Hypothermia • Remove the patient from the cold environment • Protect the patient from the cold and drafts – Use sleeping bag, blankets, newspapers, etc. – Place insulating material between patient and the surface on which he is lying 40-30 Emergency Care for Hypothermia • Avoid rough handling • Do not allow the patient to walk or exert himself • Maintain an open airway • Have suction available • Give oxygen • Begin CPR if needed 40-31 Emergency Care for Hypothermia • Passive rewarming – Placing the patient in a warm environment – Applying warm clothing and blankets – Preventing drafts 40-32 Emergency Care for Hypothermia • Active rewarming – Involves adding heat directly to the surface of the patient’s body – May be used if the patient is alert and responding appropriately – Should not delay definitive care – Important: Consult medical direction 40-33 Emergency Care for Hypothermia • Do not allow the patient to eat or drink stimulants or to drink alcohol • Do not rub or massage the patient’s extremities • During transport, turn the heat up in the patient area of the ambulance 40-34 Local Cold Injury 40-35 Local Cold Injury • Also called frostbite • Involves tissue damage to a specific area of the body • Occurs when a body part is exposed to prolonged or intense cold • Cold causes narrowing of blood vessels in affected part – Reduces blood flow to affected area 40-36 Local Cold Injury Risk Factors • Circulation problems • Use of alcohol, nicotine, and some medications • Burn or previous cold injury • Ambient temperature • Wind-chill factor • Length of exposure • Type and number of clothing layers worn • Whether or not patient is wet • Whether or not patient has had direct contact with cold objects 40-37 Superficial Cold Injury • Involves the uppermost skin layers • Skin of the exposed area first appears red and inflamed – With continued cooling, the area becomes gray or white • Patient may complain of a loss of feeling in the injured area 40-38 Deep Cold Injury • Involves more tissue layers • Whitish skin color is followed by a waxy appearance • Affected area becomes frozen • Swelling may be present • Blisters may be present 40-39 Emergency Care for Local Cold Injury • Scene size-up • Remove patient from the cold environment • Protect the affected area from further injury • Give oxygen if indicated 40-40 Emergency Care for Superficial Cold Injury [Insert figure 40-3] 40-41 Emergency Care for Deep Cold Injury • Do not break blisters • Do not rub or massage the affected area • Do not apply heat to or rewarm the affected area • Do not allow the patient to walk on an affected extremity 40-42 Local Cold Injury Rewarming • Handle affected area gently • Immerse affected area in a warm water bath – Do NOT use hot water 40-43 Local Cold Injury Rewarming • Continue rewarming until the affected part is soft and color and sensation return • Gently dry the area after rewarming • Dress the area with dry, sterile dressings [Insert figure 40-5] 40-44 Exposure to Heat 40-45 Exposure to Heat • Hyperthermia – High core body temperature – Body gains or produces more heat than it loses • Three main types of heat emergencies: – Heat cramps – Heat exhaustion – Heat stroke 40-46 Predisposing Factors • High ambient temperature • High relative humidity • Elderly • Newborns, infants • Medications – Amphetamines – Cocaine – Alcohol – Tricyclic antidepressants – Antihistamines 40-47 Types of Heat-Related Emergencies • Heat Cramps • Heat Exhaustion • Heat Stroke 40-48 Heat Cramps • Results from water and electrolytes lost during sweating – Leads to dehydration • Loss of water and electrolytes causes painful muscle spasms – Arms, abdomen, back of lower legs 40-49 Heat Exhaustion • Cool, pale, moist • Result of excessive skin heat and dehydration • Muscle cramps • Oral body • Heavy sweating temperature normal • Fast heart rate or slightly elevated • Thirst (up to 101° to 102°F • Dizziness or 38.3° to 38.9°C) • Tiredness • Weakness • May progress to heat • Headache stroke if not treated • Nausea, vomiting • Fainting 40-50 Heat Stroke • Medical emergency • Very high body temperature – Higher than 103°F or 39.4°C, orally • Act quickly to lower patient’s body temperature • Altered mental status • Dry, hot, flushed skin • Fast heart rate initially, then a slow heart rate • Headache • Dizziness • Nausea • Vision disturbances • Muscle twitching, seizures • Unresponsiveness 40-51 Emergency Care for Heat-Related Injuries • Remove patient from hot environment • If the patient has moist, pale, skin that is normal to cool in temperature: – Place patient in supine position – Give oxygen if indicated – Remove outer clothing – Consult medical direction 40-52 Emergency Care for Heat-Related Injuries • Remove patient from hot environment • If the patient has hot and dry or moist skin: – Call for ALS personnel right away – Give oxygen if indicated – Remove outer clothing – Cool the patient – Immediate transport [Insert figure 40-7] 40-53 Water-Related Emergencies 40-54 Terms • Drowning • Delayed drowning • Immersion • Submersion 40-55 Drowning Risk Factors • • • • • • • • Age Gender Race Inability to swim Use of drugs, alcohol Underlying illness or injury Child abuse, suicide, or homicide Hypothermia 40-56 Effects of Drowning • • • • • • • • • Panic Hyperventilation Gastric distention Mammalian diving reflex Hypoxia Aspiration Wet drowning Laryngospasm Dry drowning 40-57 Factors That Influence a Drowning Victim’s Chances for Survival • Length of immersion/ submersion • Duration of hypoxia • Ability to swim • Age of victim • Cleanliness of the water • Temperature of the water • Duration and degree of hypothermia • Preexisting medical conditions • Presence of drugs and/or alcohol • Presence of associated injuries • Response to initial resuscitation efforts 40-58 Scene Safety • Study the scene – Determine if approaching the patient is safe – Evaluate the mechanism of injury • Obtain additional help before contact with the patient(s) • Call for specially trained personnel as needed 40-59 Drowning Special Considerations • Suspect neck injury: – When the mechanism of injury is unknown – When signs of facial trauma are present – When signs of drug or alcohol use are present – In incidents involving use of a water slide – Swimming, boating, water-skiing, or diving accidents 40-60 Drowning Signs and Symptoms • Signs and symptoms vary • Nervous system • Respiratory system • Cardiovascular system 40-61 Establish Patient Priorities • Priority patients include: • Patients who give a poor general impression • Patients experiencing difficulty breathing • Patients with signs and symptoms of shock • Unresponsive patients with no gag reflex or cough • Responsive patients who are unable to follow commands 40-62 Secondary Survey • Physical exam – Look for other injuries • SAMPLE history • Vital signs 40-63 Emergency Care for Drowning • Scene safety • Spinal stabilization, if indicated • Give oxygen if indicated • Suction ready • Rescue breathing, CPR / AED as needed • Prompt transport 40-64 Diving Emergencies 40-65 Barotrauma • Diving-related injury caused by pressure • Can occur on ascent or descent – Ascent • Pulmonary overpressurization syndrome (POPS) or "burst lung" – Descent • “Lung squeeze" or "the squeeze" 40-66 Emergency Care for Barotrauma • Establish and maintain an open airway • Give oxygen by nonrebreather mask • Transport promptly 40-67 Air Embolism • May occur when: – Divers ascend too rapidly – Divers hold their breath during ascent • Onset is usually rapid and dramatic • Air bubbles become lodged in small arteries, cutting off circulation 40-68 • • • • • Air Embolism Signs and Symptoms Dizziness • Sudden unresponsiveness Confusion • Pink, frothy sputum Shortness of breath • Respiratory arrest Visual • Cardiac arrest disturbances Weakness or paralysis in extremities 40-69 Emergency Care for Air Embolisms • Establish and maintain an open airway • Give oxygen • Position on left side with head and chest tilted downward – If no contraindications – If approved by medical direction • Maintain body temperature • Consider transport to recompression facility 40-70 Decompression Sickness (Bends) • Results from dissolved nitrogen in blood and tissues • Size and location of nitrogen bubbles determines signs and symptoms 40-71 Decompression Sickness (Bends) • Fatigue • Weakness • Shortness of breath • Skin rash • Itching • Joint soreness • • • • • Dizziness Headache Paralysis Seizures Unresponsiveness 40-72 Emergency Care for Decompression Sickness • Establish and maintain an open airway • Give oxygen • Position on left side with head and chest tilted downward – If no contraindications – If approved by medical direction • Maintain body temperature • Consider transport to recompression facility 40-73 Bites and Stings 40-74 Pit Vipers 40-75 Pit Viper Bites Signs and Symptoms A rattlesnake bite six hours after the injury. Same patient seven weeks after the rattlesnake bite. 40-76 Pit Viper Bites Signs and Symptoms Local Systemic • Fang marks or semicircle of teeth marks • Burning pain • Red and swollen area around the fang or teeth marks • Discoloration and blisters common • • • • Weakness Sweating Nausea and vomiting Shock 40-77 Coral Snakes [Insert figure 40-13] 40-78 Early Coral Snake Bites Signs and Symptoms Late • Scratch marks or tiny puncture marks • Little or no pain at site • Minimal to moderate swelling • Slurred speech • Muscle weakness • Difficulty swallowing • Dilated pupils • • • • • Nausea/vomiting Difficulty breathing Seizures Paralysis Respiratory failure 40-79 Emergency Care for Snakebites • Ensure safety of all rescuers • It is not necessary to capture the snake for identification • Establish and maintain an open airway • Give oxygen if indicated • Keep the patient calm • Limit patient’s physical activity • Remove rings, watches, and tight clothing from the injured area before swelling begins 40-80 Emergency Care for Snakebites • Pressure immobilization technique [Insert figure 40-15] 40-81 Emergency Care for Snakebites • Monitor swelling [Insert figure 40-16] 40-82 Emergency Care for Snakebites • Do not apply heat or cold to the bite site • Do not cut the wound • Do not attempt to suck out the venom • Do not apply a constricting band or tourniquet 40-83 Arthropods • • • • • • Spiders Insects Crustaceans Scorpions Lice Fleas • • • • • • Ticks Bedbugs Horseshoe crabs Centipedes Millipedes Mites 40-84 Black Widow Spider 40-85 Brown Recluse Spider 40-86 Emergency Care for Spider Bites • • • • Maintain an open airway, give oxygen Gently wash the area Remove jewelry from injured area If swelling present, mark outer edge and note the time with a pen or marker. • Observe closely for development of allergic reaction; treat as needed • Transport 40-87 Scorpion Stings 40-88 Emergency Care for Scorpion Stings • • • • • Maintain an open airway Give oxygen Gently wash the area Remove jewelry from injured area If swelling present, mark outer edge and note the time with a pen or marker • Observe closely for development of allergic reaction; treat as needed • Transport 40-89 Hymenoptera Stings (Bees, Wasps, and Ants) 40-90 Emergency Care for Hymenoptera Stings • Maintain an open airway, give oxygen if indicated • Remove stinger by scraping with flat edge • Remove jewelry from injured area • If swelling present, mark outer edge and note the time with a pen or marker. • Observe closely for development of allergic reaction; treat as needed 40-91 • Transport Marine Life Stings [Insert figures 40-27] 40-92 Emergency Care for Venomous Marine Injuries • Maintain an open airway, give oxygen • Stingray injury – Flush wound immediately – Immerse injured part in hot water to patient tolerance (109° to 113°F, or 43° to 45°C) for 30 to 90 minutes – Elevate injured arm or leg – Cover wound with a sterile dressing • Transport 40-93 Dog and Cat Bites [Insert figure 40-28] 40-94 Emergency Care for Dog and Cat Bites • • • • • • Maintain an open airway Give oxygen Control bleeding If no bleeding, gently wash the area Remove jewelry from injured area If swelling present, mark outer edge and note the time with a pen or marker. • Transport 40-95 Human Bites • Usually occur while playing or fighting • Clenched fist injury – Also called a fight bite – Most serious human bite – Infection common 40-96 Emergency Care for Human Bites • • • • • • Maintain an open airway Give oxygen if indicated Control bleeding If no bleeding, gently wash the area Remove jewelry from injured area If swelling present, mark outer edge and note the time with a pen or marker. • Transport 40-97 Questions? 40-98