Overdose PPT
advertisement

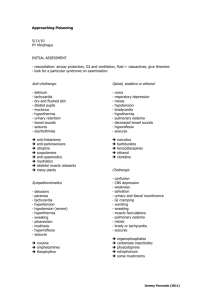
Poisons and Poisoning Dr Ian Wilkinson Clinical Pharmacology Unit Accidental? Deliberate? Suicides in the UK • ~6,300 suicides pa – 20% of deaths in young people • ~140,000 attempted suicides (parasuicides) – Most common 15-19 year old females – Most common method is poisoning • 50% paracetamol General Comments • Try and get as much history as possible including witnesses • People truly wanting to commit suicide often lie • Remember the ABCs: – Airway Clear mouth & throat, gag reflex – Breathing O2 saturation, ABGs – Circulation Venous access, IV fluids if shocked • Assess GCS • Examination History • • • • • • When, what, how much ? Why? Circumstances PMHx, Drug history Psychiatric history Assess mental status and capacity Care with names! • Distalgesic • Anadin Investigations • Always check blood glucose. • Send blood & urine for toxicology screening. • ALWAYS measure paracetamol & salicylate levels – Failure to diagnose & treat is negligent. • U&Es, LFTs, glucose, ABG, clotting, bicarbonate • ECG, CXR • Specific blood levels Management • Supportive – Correct hypoxia, hypotension, dehydration, hypohyperthermia, and acidosis – Control seizures • Monitor – TPR, BP, ECG, Oxygenation, GCS • General – Absorption – Elimination – Specific antidotes Absorption • NEVER Ipecacuanha • Gastric lavage – Only if within 1 hour & life-threatening amount – Never for corrosives – If LOC intubate • Activated charcoal – 50 g single or repeated dose ( elimination) – Doesn’t bind heavy metals, ethanol, acids Elimination • Multiple dose activated charcoal – Quinine, phenobarbitone • Charcoal haemoperfusion – Barbiturates, theophylline • Diuresis • Urinary alkalinization • Dialysis Paracetamol Overdose • • • • Most common drug taken in overdose Few symptoms or early signs As little as 12g can be fatal Hepatic and renal toxin – Centrolobular necrosis • More toxic if liver enzymes induced or reduced ability to conjugate toxin Paracetamol Metabolism Management • General measures including – U&Es, LFTs, glucose, clotting ABG, bicarbonate, paracetamol and salicylate levels – Activated charcoal • <8 hours – Take level after four hours – Start N-aceylcysteine if above treatment line – Patients are usually declared fit for discharge from medical care on completion of its administration. However, check INR, creatinine and ALT before discharge. Patients should be advised to return to hospital if vomiting or abdominal pain develop or recur Management 2 • >8 hours – Urgent action required because the efficacy of NAC declines progressively from 8 hours after the overdose – Therefore, if > 150mg/kg or > 12g (whichever is the smaller) has been ingested, start NAC immediately, without waiting for the result of the plasma paracetamol concentration • >24 hours – Still benefit from starting NAC Treatment Graph N-acetylcysteine • Supplies glutathione • Dosage for NAC infusion - ADULT – (1) 150mg/kg IV infusion in 200ml 5% dextrose over 15 minutes, then – (2) 50mg/kg IV infusion in 500ml 5% dextrose over 4 hours, then – (3) 100mg/kg IV infusion in 1000ml 5% dextrose over 16 hours • Side-effects – Flushing, hypotension, wheezing, anaphylactoid reaction • Alternative is methionine PO (<12 hours) Aspirin Overdose • Early features – hyperventilation, sweating, tremor, tinnitus, nausea / vomiting, or hyperpyrexia • Metabolic features – Hypo- or hyper-glycaemia, hypokalaemia, respiratory alkalosis, metabolic acidosis • Others – renal failure, pulmonary oedema, seizures, coma, death Management • General measures • Bloods – – – – • • • • Salicylate (paracetamol) level >2 hours, and after 2hrs >700 potentially lethal >500 moderate-severe poisoning U&Es, glucose, ABG, bicarbonate Activated charcoal Rehydrate, monitor glucose, correct acidosis and K+ If levels >500mg/L alkalanize urine (HCO3-) Levels > 700 mg/L before rehydration, renal failure or pulmonary oedema consider haemodialysis TCAs -Introduction • Potentially fatal (2.5 to 3.5g of amitriptyline) • Neurological and cardiac problems common – Toxicity due to anticholinergic actions, and direct quinidine-like effect on the myocardium • Serious toxicity results from:– – – – Ventricular dysrhythmias Seizures Hypotension Respiratory depression • Initial symptoms at presentation may be trivial, and most major problems occur within 6hrs TCAs-Features of poisoning • Peripheral – Sinus tachycardia, hot dry skin, dry mouth, urinary retention, hypotension and hypothermia may occur • CNS – Dilated pupils, ataxia, nystagmus, squint, LOC, coma, seizures, respiratory depression, tone, reflexes, plantars • ECG – prolonged PR and QRS interval, QT – ventricular dysrhythmias TCAs -Management • GCS and QRS, best indicators of toxicity • Supportive – do not use flumazenil if benzo taken • Check airway, maintain ventilation, correct hypoxia – Check ABG, if CO2 requires ventilation • • • • • Correct hypotension (crystalloids) Gastric lavage if within 1 hr, and activated charcoal Rx fits and agitation with diazepam Rewarm slowly if hypothermic Close monitoring for 24hrs TCAs- Dysrhythmias • Carful ECG monitoring is required – QRS interval is a guide to cardiac toxicity (>100ms) • Avoid antidysrhythmic drugs. They may make matters worse • Correct hypoxia and acidosis. Aim for a pH of 7.45-7.50 (no higher) – use iv boluses of sodium bicarbonate • Sodium loading may also help • Prolonged CPR may be of use Tricyclic OD – Initial ECG Tricyclic OD – Recovery ECG Benzodiazepine Overdose • Deaths from poisoning with benzodiazepines alone are rare, but may be lethal in combination with other CNS depressants • Treatment is supportive and aimed at maintaining adequate ventilation whilst supporting cardiovascular depression • Flumazenil (specific benzodiazepine antidote) is not licensed (in the UK) for routine use in benzodiazepine overdoses • Flumazenil may induce seizures; particularly dangerous where tricyclic antidepressants have been taken • Flumazenil, may however, be used in the differential diagnosis of unclear cases of multiple overdoses but expert advice is ESSENTIAL. Other agents • • • • • • • Opiates Iron Lead Digoxin Calcium blockers Ethylene glycol Lithium Naloxone Desferrioxamine Sodium EDTA FAB Calcium Ethanol Dialysis