Sanglas_TAFITCI_9rr.doc
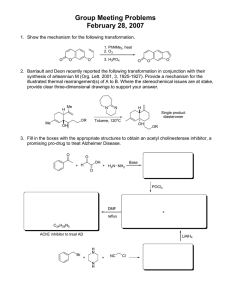
advertisement

0 Structure of activated thrombin-activatable fibrinolysis inhibitor, a molecular link between coagulation and fibrinolysis. Laura Sanglas, 1,4 Zuzana Valnickova, 2,4 Joan L. Arolas, 3 Irantzu Pallarés, 1 Tibisay Guevara, 3 Maria Solà, 3 Torsten Kristensen, 2 Jan J. Enghild, 2 Francesc X. Aviles, 1,* & F. Xavier Gomis-Rüth 3,* 1 Institut de Biotecnologia i de Biomedicina and Departament de Bioquímica i Bio. Mol. (Facultat de Ciències); Universitat Autònoma de Barcelona, E-08193 Bellaterra (Spain) 2 Center for Insoluble Protein Structures at the Department of Molecular Biology; Science Park; University of Århus; Gustav Wieds Vej 10c, DK-8000 Århus C (Denmark) 3 Department of Structural Biology at the Molecular Biology Institute of Barcelona, CSIC; Barcelona Science Park; c/ Balidiri Reixach,10-12 and 15-21; E-08028 (Spain) 4 These authors contributed equally to this study and share first authorship. * Correspondence: <xgrcri@ibmb.csic.es> or <francescxavier.aviles@uab.es>. The authors state they have no competing financial interest. RUNNING TITLE: Active TAFI carboxypeptidase in complex with TCI 1 SUMMARY Thrombin-activatable fibrinolysis inhibitor (TAFI) is a metallocarboxypeptidase (MCP) that links blood coagulation and fibrinolysis. TAFI hampers fibrin-clot lysis and is a pharmacological target for the treatment of thrombotic conditions. TAFI is transformed through removal of its prodomain by thrombin-thrombomodulin into TAFIa, which is intrinsically unstable and has a short half-life in vivo. Here we show that purified bovine TAFI activated in the presence of a proteinaceous inhibitor renders a stable enzyme-inhibitor complex. Its crystal structure reveals that TAFIa conforms to the /-hydrolase fold of MCPs and displays two unique flexible loops on the molecular surface, accounting for structural instability and susceptibility to proteolysis. In addition, point mutations reported to enhance protein stability in vivo are mainly located in the first loop and in another surface region, which is a potential heparin-binding site. The protein inhibitor contacts both the TAFIa active site and an exosite, thus contributing to high inhibitory efficiency. 2 INTRODUCTION After blood-vessel injury, hemostasis induces fibrin clot formation to prevent blood loss and trigger vessel repair (Mann et al., 1988). This clot must be removed after tissue repair to restore blood flow. These processes are tightly regulated by the coagulation and fibrinolytic cascades because imbalance may lead to thrombosis, heart attack and stroke, or to bleeding as in hemophilia (Boffa et al., 2001). Hemostasis is modulated by thrombin-activatable fibrinolysis inhibitor (TAFI), also known as procarboxypeptidase (PCP) B from plasma, procarboxypeptidase B2, U and R. It attenuates fibrinolysis by removing surface-exposed C-terminal lysine residues from the fibrin clot (Arolas et al., 2007; Bajzar et al., 1995; Boffa et al., 2001; Bouma and Mosnier, 2003; Eaton et al., 1991; Hendriks et al., 1989; Willemse and Hendriks, 2007). TAFI is the zymogen of a B-type zincdependent metallocarboxypeptidase (MCP), which is produced and secreted by the liver, and apart from carboxypeptidase N, it is the only known MCP found in human plasma. TAFI is similar in sequence to human pancreatic PCPs (see Fig. 1 and (Arolas et al., 2007), (Pereira et al., 2002)). However, it differs from these proenzymes in that the pro-domain is highly glycosylated at four sites, the glycosylation accounting for ~20% of the total molecular mass (Valnickova et al., 2006). During coagulation, TAFI is processed by thrombin/thrombomodulin to TAFIa through removal of its 92residue pro-domain. In contrast to pancreatic MCPs, both TAFI and TAFIa uniquely display carboxypeptidase activity against larger substrates. However, while TAFIa has a half-life of less than ten minutes, in contrast to its robust pancreatic counterparts, TAFI is stable in circulation (Boffa et al., 1998; Valnickova et al., 2007). Protein inhibitors account for a control mechanism of proteolytic activity. Latexin, alias ECI, is the only known endogenous A/B-type MCP protein inhibitor found in mammals (Pallarès et al., 2005). Its role as a TAFIa inhibitor in fibrinolysis is questionable, however, as it is not found in blood. In contrast, TCI is a physiologically relevant inhibitor that has been found in the hematophagous ixodid tick, Rhipicephalus bursa, which only feeds on ruminants. Such parasites need to inactivate host inflammation and defense mechanisms and prevent coagulation in the gut 3 during feeding through protein inhibitors. TCI displays the highest affinity for TAFIa (equilibrium dissociation constants of 1.3 and 1.2 nM for bovine and human TAFIa, respectively) and strongly accelerates fibrinolysis similarly to the A/B-type MCP inhibitors from potato (PCI) and leech (LCI), which also target TAFIa. These protein inhibitors have proven potential as therapeutic adjuvants and they are now under clinical trials in various cardiovascular conditions (Arolas et al., 2007). In addition, stimulation of the TAFI pathway is being examined as an approach to the treatment of hemophilia (Mosnier and Bouma, 2006; Walsh et al., 1971). Such research attests to the importance of TAFI as a pharmacological target for cardiovascular disease treatment (Do et al., 2005; Hsu et al., 2007; Klement et al., 1999; Refino et al., 2000). Recent data show that the TAFI plasma concentration in humans varies strongly and that high concentrations are a risk factor for thrombosis and coronary artery disease (Silveira et al., 2000; van Tilburg et al., 2000), while low levels have been correlated with chronic liver disease (Van Thiel et al., 2001). Accordingly, TAFI has been proposed as a molecular marker for vascular diseases (Boffa and Koschinsky, 2007; Boffa et al., 2001; Mann et al., 1988; Wang et al., 2007). In addition to its involvement in fibrinolysis, TAFI has been implicated in wound healing, blood-pressure regulation, tissue remodeling and inflammation by inactivating plasminogen activation, bradykinin and inflammatory mediators (for a review, see (Arolas et al., 2007)), as well as in sepsis (Taylor and Bajzar, 2005), endometriosis (Bedaiwy and Casper, 2006), and pulmonary fibrosis (Gabazza et al., 2006). TAFI is also expressed in the neuronal endoplasmic reticulum of hippocampal neurons, potentially playing a role in the processing of native -amyloid precursor protein in the brain (Matsumoto et al., 2000; Matsumoto et al., 2001). Here, latexin (alias ECI), which has been detected in rodent and human brain (Arimatsu, 1994; Normant et al., 1995), could play a role as an endogenous TAFI inhibitor. Given the importance and key role of the TAFI/TAFIa axis in thrombotic conditions, the detailed structure analysis of TAFIa should contribute to an explanation for its intrinsic instability and provide a mold for the design of small-molecule inhibitors, thus contributing to alternative therapeutic approaches. 4 RESULTS AND DISCUSSION TAFI purification, complex formation with TCI and heparin-binding assay – Glycaninduced heterogeneity, the minute amounts retrievable from single-patient samples, the impossibility of establishing efficient recombinant over-expression systems, and the instability of human TAFIa have hampered structural studies on this protein since its discovery in 1988. We sought to overcome these problems by choosing a highly homologous orthologue from a non-human mammalian species, for which large amounts of blood could be obtained from one individual. We purified TAFI from a single cow to homogeneity, essentially in three large-scale liquid chromatography steps, and showed it to be active against a chromogenic substrate (see materials and Methods). The kinetic properties of bovine TAFI and human TAFI were compared in parallel experiments and the data suggested that the two proteins are very similar in terms of activity (Table 1), in agreement with their 78% sequence identity (see Fig. 1). Freshly purified TAFI was subsequently incubated in vitro with the physiological processor thrombin in the presence of its modulator thrombomodulin and TCI. The TAFIa/TCI complex was stable for several days/weeks and suitable for structural studies. In addition, our experiments with heparin-sepharose showed that both human and bovine TAFI binds heparin, since most of the protein eluted only in the presence of 200-500mM NaCl (data not shown). This suggests that glycosaminoglycans may modulate TAFI as described for antithrombin III and thrombin (Bjork and Lindahl, 1982). Overall structure of TAFIa, active-site cleft and potential heparin-binding sites - TAFIa has a compact globular shape and shows the classic /-hydrolase fold of A/B- and N/E-type MCPs (Arolas et al., 2007; Vendrell et al., 2000). It has a central eight-stranded -sheet (strands 1-8) of strand connectivity +1,+2,-1x,-2x,-2,+1x,-2, which vertically spans the molecule top to bottom accumulating a vertical twist of ~130º (Figs. 1 and 2a). This gives rise to a concave face, which accommodates helices 4 and 6, and the active-site cleft. At the rear, the convex side of the sheet harbors 1-3, 5 and 7 and the surface N- and C-termini of the molecule. The access to the active site is like a funnel, whose rim is shaped by a series of irregular loop segments required for 5 interactions of the protease moiety with the pro-domain and with cognate protein inhibitors in A/Btype MCPs (Pallarès et al., 2005). These segments include the loop connecting strand 8 with helix 7 (L87), L32, L56, L65, as well as the first part of the 53-residue segment connecting 3 and 4 (L34). This long segment is stabilized by two disulfide bonds (Cys138-Cys161 and Cys152-Cys166; for numbering conventions, see Fig. 1) and closes the front and the bottom of the active site and the specificity pocket, thus contributing to the characteristic cul-de-sac of these exopeptidases (Fig. 2c). The catalytic zinc ion resides at the bottom of the funnel-like cleft and is coordinated by His69 N1 (2.09Å apart) and by Glu72, in an asymmetric bidentate manner, through its O2 (2.01Å) and O2 (2.76Å) atoms (Fig. 2c). These two residues are imbedded in a consensus sequence, HXXE (amino-acid one-letter code; X for any residue), characteristic of A/B- and N/E-type MCPs (Hooper, 1994). The third TAFIa zinc ligand is His196 N1 (2.08Å). An acetate ion is found next to the zinc, partially occupying the specificity pocket and hydrogen-bonded through one of its carboxylate oxygen atoms to Arg127 N2 (3.02Å), Arg145 N2 (2.89Å), and Tyr248 O (2.58Å). The latter is in the “down” orientation usually found in MCPs with occupied pockets (Reverter et al., 2000). The other acetate carboxylate oxygen atom is bound to Asn144 N2 (2.90Å) and Arg145 N1 (2.80Å). As shown for other MCPs, the protein residues engaged in substrate binding and catalysis in A/Btype MCPs (Auld, 2004; Vendrell et al., 2000) are Arg127 and Glu270 forming S1; Arg71, Ser197, Tyr198, and Ser199 delimiting S2; and Phe279 contributing to S3. Typical B-type MCP specificity towards basic side chains in substrates is due to an S1’ pocket that is hydrophobic at its entrance and acidic at its bottom. The pocket is formed by the side chains of Asn144, Arg145, Val203, Gly243, Leu247, Ala250, Thr268, Tyr248, and Asp255. The terminal carboxylate group of a substrate, when it is trapped for scission, is fixed by Asn144, Arg145, and Tyr248, while the scissile carbonyl group is near Glu270, Arg127, and the catalytic zinc (Fig. 2c). Heparin has been shown to stabilize TAFIa against spontaneous inactivation (Mao et al., 1999). In the absence of structural data of a complex with heparin, surface anions may point to 6 potential binding sites. In the present complex, two pairs of sulfate ions found in the structure may represent two potential independent binding sites for heparin sulfate groups. In one case, the two sulfate ions are 10Å apart, one is bound by Ser158 N and O, and Arg52I N1 and N2 from the TCI moiety, and the other is bound by Ser160 N and O, and Ala137 N. The distance between sulfate ions is similar to that found in the thrombin/heparin complex structure, in which two sets of sulfate groups from sulfoiduronate or disulfoglucosamine moieties are separated by two (11Å apart) and three (10Å apart) monosaccharides, respectively (Protein Data Bank (PDB) access code 1XMN; (Carter et al., 2005)). The sulfur atoms of the second potential TAFIa site are 20Å apart, which is compatible with the spacing of three or four monosaccharides within a heparin chain (Carter et al., 2005). Here, the sulfate groups are bound by His1501 N2, Ser209 O, and Ser211 O and by His216 N2, Arg224 N2 and N, and Ser 220 O, respectively, and they affect segment 5-L57-7 on top of the molecule (Fig. 2a). It is interesting to note that this region contains a high number of residues whose substitution by random mutagenesis has been shown to influence TAFIa stability ((Knecht et al., 2006; Schneider et al., 2002); see Fig. 1 and below). Therefore, heparin binding at this site could thus become a regulatory mechanism affecting the half-life of TAFIa. For the last six years, the structure of human pancreatic PCPB1, solved by two of our groups, has been a model for TAFI (Marx et al., 2000; Pereira et al., 2002). Sequence and structure comparison of the homology model obtained from the former with bovine TAFIa (Fig. 1 and 2b) enables to assess that the gross of the model proposed was valid. In particular, TAFI very likely possesses an equivalent pro-domain to PCPB1 with a globular part folded as an open sandwich. This globular part would be linked to the mature enzyme moiety through a connecting segment, which would include an -helix. The pro-domain would be likewise placed on top of the active site, which would be preformed in the TAFI zymogen. With respect to the mature enzyme moiety, the overall structure is also very similar and this similarity comprises the identity and arrangement of the active-site residues (see also below). There are two major points that were anticipated by the PCPB1based model: (i) An essential salt bridge made up between Asp41 of the pro-domain and by an 7 active-site residue, Arg145, is not present in TAFI as inferred from TAFIa. This interaction is thought to account for the lack of activity of B-type MCP zymogens and therefore it was postulated that TAFI might show intrinsic activity, at least against small substrates (Pereira et al., 2002). This hypothesis was recently proven right for experiments in vitro (Valnickova et al., 2007). (ii) Our model further anticipated that L24 could be a hot spot accounting for instability as it showed highly-positive values of pseudo-potential energy (Pereira et al., 2002). This is confirmed by the present study (see below). Structural determinants of TAFIa inhibition through TCI – The proteinaceous inhibitor TCI consists of tandem structurally-similar small modules, an N-terminal (NTD; Asn1I-Leu37I) and a Cterminal domain (CTD; Cys40I-Leu74I) linked by two residues, Thr38I and Gly39I (Fig. 2a). Each domain is compacted by three internal disulfide bonds and consists of a short -helical fragment and a subsequent antiparallel triple-stranded -sheet. This fold resembles -defensin, as previously reported (Arolas et al., 2005b). The structural similarity of the NTD and the CTD suggests that this inhibitor may have arisen by gene duplication. The two TCI domains do not interact with each other suggesting they are flexible in solution. This feature means that the two domains could bind simultaneously to separate sites of a target protease, which would provide for more potent and selective inhibition. The way in which TCI inhibits TAFIa resembles its inhibition of human CPB1 (PDB 1ZLI; (Arolas et al., 2005b)). Both complexes display an rmsd of 0.76Å for 368 common C atoms deviating by less than 3Å. TCI mainly inhibits TAFIa through its CTD (Fig. 2c), with an interaction surface between the enzyme and the inhibitor spanning 666Å2. This domain lies on top of the funnellike rim surrounding the active-site cleft and establishes 32 contacts (<4Å) with the TAFIa protein moiety. As observed in other MCP/inhibitor complexes, such as those made by PCI (Rees and Lipscomb, 1982) and LCI (Reverter et al., 2000), the C-terminal residue, here His75I, is cleaved and the new C-terminus, Leu74I, approaches and contacts the TAFIa catalytic zinc ion through its carboxylate oxygen atoms (2.12 and 2.52 Å apart). This means that the metal ion is coordinated by a total of six ligands in a basically tetrahedral arrangement (two oxygen and two nitrogen atoms 2.01- 8 2.12Å apart), with another two oxygen ligands at 2.52 and 2.76Å (Fig. 2c). In addition to this contact, CTD interacts with TAFIa through 15 hydrogen bonds and five hydrophobic contacts (see Table 2). The NTD of TCI contacts TAFIa over a surface of 413Å2 and mainly interacts with TAFIa region Trp120-Met125 at the beginning of the long L34 segment. This interaction includes 21 contacts (<4Å), among them six hydrophobic contacts and seven hydrogen bonds and polar interactions (see Table 2). Accordingly, the interaction mediated by NTD is weaker than that performed by CTD, but it identifies Trp120-Met125 as an exosite contributing to complex stability, which could be targeted by inhibitors in addition to the active-site to enhance specificity and potency (Fig. 2d). This exosite is actually specific for the dual binding mode of the inhibitor as it was also found in the complex of TCI with human CPB (Arolas et al., 2005b). Interestingly, although the composite complex interaction surface provided by NTD and CTD (1,080Å2) is smaller than typical protease-inhibitor interfaces (1,250-1,750Å2, (Janin and Chothia, 1990), the number and type of contacts in the TCI/TAFIa complex renders it as stable as that formed by human CPA4 and latexin, which displays a much larger contact surface (1170Å2) but fewer intermolecular contacts and no direct interaction with the active-site cleft (Pallarès et al., 2005). Structural determinants of TAFIa instability, conformational rearrangement and proteolytic inactivation in vivo –The short half-life of TAFIa has been correlated with a temperature-dependent conformational instability, which renders the molecule dysfunctional and eventually increases its susceptibility to proteolysis (Arolas et al., 2007; Boffa et al., 2000; Boffa et al., 1998). Several TAFIa variants have lower thermal sensitivity and thus longer half-lives and a greater antifibrinolytic potential (Ceresa et al., 2007; Ceresa et al., 2006; Marx et al., 2004). These variants include point mutants (Fig. 1), as well as two chimeric constructs between human TAFI and CPB1 containing segments 201-240 and 201-308 from the latter, respectively. Inspection of the respective regions in the TAFIa structure shows that these mutations map onto structure elements L23, L34, 6, L65, 5, L57, 7 and 6. The beneficial mutations accumulate at segment 5-L57-7, which lies on top of the molecule between Arg210 and Ser242 (Figs. 1 and 2a). In addition, residues in this segment, Arg210, Lys235 and Arg237, have been identified as hot spots for proteolytic 9 inactivation of TAFIa through thrombin and plasmin (Boffa et al., 2000; Boffa et al., 2001). This segment is fully defined and rigid in the TAFIa structure and it is topologically equivalent in the stable A/B-type MCPs such as human CPB1. However, its co-localization with a putative heparinbinding site (see above), together with the experimental evidence that human TAFI may bind heparin, suggests a role for segment 5-L57-7 in the regulation of TAFIa half-life. The present TAFIa structure provides evidence for another hypothesis for the mechanism of destabilization, which is supported by stronger evidence: Two vicinal segments contained in L23 and L24 are flexible in the TAFIa structure and five residues are untraceable within each loop (Figs. 1 and 2b). Intrinsically flexible regions on the molecular surface of a protein structure can be directly correlated with instability, conformational changes/lability and proteolytic susceptibility, and, thus, degradation (Zappacosta et al., 1996), especially if we consider a protease-rich medium like blood. The equivalent regions of all other A/B-type MCPs thus far structurally analyzed are well ordered and rigid, inter alia in active and zymogenic human pancreatic CPB1 (except for some isolated side chains; see Fig. 2b and (Arolas et al., 2005b; Pereira et al., 2002)). Flexibility may be favored in TAFIa by a one-residue insertion after position 56, which is absent in all pancreatic MCPs (see Fig. 1 and (Pereira et al., 2002)). In addition, a unique lysine potentially targetable by thrombin and plasmin is found at position 55 within L23 both in bovine, human, mouse and rat TAFIa, but it is absent in pancreatic counterparts (Fig. 1). In contrast to the preceding lysine at position 54, Lys55 should protrude from the TAFI molecular surface and be accessible to the action of proteases. Mutation of Lys55 to asparagine has actually been found in human TAFIa variants that have 2.6times (a double point mutant) and 22-times (a fourfold mutant) longer half-lives than the wild-type enzyme (Knecht et al., 2006). Furthermore, mouse, rat and bovine TAFIa undergo cleavage within L23 as part of their inactivation processes. These findings back comparative studies of human and rodent orthologues, which revealed similar but not identical biochemical characteristics, thus suggesting a similar role during fibrinolysis in vivo ((Hillmayer et al., 2006) and our unpublished results). According to the preceding considerations, the two-loop flexible region here described could be conceived as hot spots to trigger destabilization and inactivation of the entire molecule. 10 In summary, the 3D crystal structure of TAFIa shows unique flexible features, which account for the instability of the molecule as compared to the robust pancreatic counterparts. In the absence of an endogenous inhibitor in the blood stream, it must be assumed that structural instability is the principal modulator of TAFI/TAFIa activity, as was revealed by fluorescence studies (Boffa et al., 2000; Ceresa et al., 2007). Major structural rearrangement leads to a loss of enzymatic activity, which in turn causes sites susceptible to proteolysis to become available for degradation (Boffa et al., 2000; Marx et al., 2000). In addition, the structural determinants of inhibition through a protein inhibitor revealed by the present study may pave the way for the design of TAFIa inhibitors to be used in thrombolytic therapies. The discovery of an exosite provides additional elements to be considered for drug design. Initial steps in this direction have already been undertaken: TCI markedly accelerates lysis of human plasma clots and its usage as an adjuvant is a promising approach (Arolas et al., 2005b; Arolas et al., 2007). 11 MATERIALS AND METHODS Preparation of human and bovine TAFI – Human TAFI was purified as described (Eaton et al., 1991; Wiman, 1980) and its functionality was tested as previously reported (Valnickova et al., 2007). Bovine TAFI was purified from 10L of bovine blood collected at the local slaughterhouse from a single cow using 10mM EDTA as anticoagulant. At this concentration, the chelating agent has no influence on the activity, i.e. the zinc ion is not removed. Plasma was recovered by centrifugation and polyethylene glycol (PEG) 8000 was then added to a final concentration of 6% (w/v). After 1h, the precipitate was collected by centrifugation and discarded. The supernatant was applied to a 1L ECH-lysine-sepharose column (GE Healthcare), equilibrated in binding buffer (50mM NaH2PO4, 100mM NaCl, pH7.5). The plasminogen-depleted flow-through was applied to a 500mL-plasminogen-sepharose column equilibrated with binding buffer. The column was washed and bovine TAFI was eluted using 50mM -amino-caproic acid in binding buffer. After a buffer exchange to 20mM Tris·HCl, pH7.5 (buffer B), bovine TAFI was separated from contaminating proteins by using a GE Healthcare 5mL-HiTrap Q-HP anionic-exchange chromatography column connected to an ÄKTAprime plus system (GE Healthcare). The column was developed with a linear gradient from 20mM Tris·HCl, pH7.5 (buffer A) to 20mM Tris·HCl, 1M NaCl, pH7.5 (buffer B) at a flow-rate of 3mL/min and a 0.5% B increase/min. Determination of activity – Human and bovine TAFI activity was essentially determined as described previously (Buelens et al., 2008). Briefly, 1µg of the zymogen was incubated with increasing concentrations of the Hippuryl-Arg substrate (0-30mM), in duplicates, for 60min at 37C in a final volume of 60µl. The reactions were terminated by the addition of 20µl 1M HCl followed by 20µl of 1M NaOH and 25µl of 1M NaH2PO4, pH 7.4. Upon addition of 60µl 6% cyanuric chloride dissolved in 1,4-dioxane, the samples were vortexed vigorously and centrifuged at 16000g for 5min. The supernatant was subsequently transferred to 96-well microtiter plate and the absorbance measured at 405nm in a FLUOStar Omega plate reader (BMG Labtech) using the endpoint mode. 12 Heparin binding assay of human TAFI – Human TAFI (15g) in 500L of buffer A, was incubated with 100L of heparin-sepharose for 1h at 22ºC. The supernatant was removed and TAFIbound heparin-sepharose was washed in 5x1mL buffer A. Elution of TAFI proceeded in five steps of 100L buffer A containing increasing amounts of NaCl. TAFIa/TCI complex formation and purification – Recombinant TCI inhibitor was expressed and purified as previously published (Arolas et al., 2005a). Bovine TAFI was activated by incubating 1mg-batches of zymogen (0.1mg/mL in 20mM Tris-HCl, 200mM NaCl, pH7.5) with 10µg of rabbit thrombomodulin (American Diagnostica), 5µg of human thrombin (Sigma) and 0.4mg of TCI for 2h at 25ºC. The resulting TAFIa/TCI complex was immediately purified by hydrophobic interaction chromatography on a Resource Phenyl column (GE Healthcare) eluting with a decreasing linear gradient from 1M (NH4)2SO4 to 0 in buffer B (50mM Tris·HCl, 150mM NaCl, pH7.5). Purified complex obtained from several batches was pooled and injected to a HiLoad Superdex 200 26/60 column (GE Healthcare) equilibrated with buffer B. The complex was concentrated and bufferexchanged to 10mM Tris·HCl, 50mM NaCl, pH7.5 using an Amicon Ultra-4 concentrator (5kDacutoff, Millipore) and subsequently an Amicon Centricon concentrator (10kDa-cutoff, Millipore) to a final concentration of 8.5mg/mL. The purity and integrity of the complex were assessed by SDSPAGE and mass spectrometry (data not shown). Crystallization of the complex - Crystallization assays were performed following the sittingdrop vapor diffusion method. Reservoir solutions were prepared by a Tecan robot and 200-nL crystallization drops were dispensed on 96x3-well CrystalQuick plates (Greiner) by a Cartesian nanodrop robot (Genomic Solutions) at the joint IBMB-CSIC/IRB/Barcelona Science Park HighThroughput Crystallography Platform (PAC). Best crystals appeared after 3-4 days in a Bruker steady-temperature crystal farm at 20°C with 0.2M (NH4)2SO4, 0.1M NaAcO, 10% PEG 4000, pH4.6 as reservoir solution. These conditions were efficiently scaled up to the microliter range with Cryschem crystallization dishes (Hampton Research). A complete diffraction dataset was collected at 100K from a single N2 flash-cryo-cooled (Oxford Cryosystems) crystal on a marCCD detector at beam line ID23-2 of the European Synchrotron Radiation Facility (ESRF, Grenoble, France) within 13 the Block Allocation Group "BAG Barcelona". Crystals were trigonal and harbored one complex per asymmetric unit. Diffraction data were integrated, scaled, merged, and reduced with programs MOSFLM and SCALA within the CCP4 suite (CCP4, 1994) (see Table 3). Structure solution and refinement - The structure was solved by Patterson-search methods with program AMoRe (Navaza, 1994) using all diffraction data between 15 and 4Å resolution. The coordinates of the complex between human CPB1 and TCI (PDB 1ZLI) were used as a searching model. A single solution was found at 55.9, 47.1, 288.0 (,, in Eulerian angles) and 0.339, 0.319, 0.337 (x,y,z, as fractional unit-cell coordinates) after rigid-body refinement. This solution gave a correlation coefficient in structure factor amplitudes of 51.1% and a crystallographic Rfactor of 42.9% (for definitions, see Table 3 and (Navaza, 1994)). Subsequently, manual model building on a SiliconGraphics workstation using program TURBO-Frodo alternated with crystallographic refinement with REFMAC5 within the CCP4 suite until completion of the model (see Table 3). This model contained the protein residues of the mature protease moiety (molecule A) from Ser7 to Val308 (see Fig. 1 for the numbering convention) and the catalytic zinc ion. Two segments, Lys55-Ala58 and Glu93-Thr97 were undefined and thus not included in the final model. The TCI model (molecule B; suffix I) was fully defined in the complex for its 74 residues (Asn1I-Leu74I, after cleavage of the C-terminal His75I residue). Miscellaneous – Figure 2 was prepared with program MOLMOL (Koradi et al., 1996). The final coordinates of the TAFIa/TCI complex have been deposited with the PDB at www.pdb.org (access code 3D4U). 14 REFERENCES Arimatsu, Y. (1994). Latexin : a molecular marker for regional specification in the neocortex. Neurosci Res 20, 131-135. Arolas, J. L., Lorenzo, J., Rovira, A., Castella, J., Aviles, F. X., and Sommerhoff, C. P. (2005a). A carboxypeptidase inhibitor from the tick Rhipicephalus bursa: isolation, cDNA cloning, recombinant expression, and characterization. J Biol Chem 280, 3441-3448. Arolas, J. L., Popowicz, G. M., Lorenzo, J., Sommerhoff, C. P., Huber, R., Avilés, F. X., and Holak, T. A. (2005b). The three-dimensional structures of tick carboxypeptidase inhibitor in complex with A/B carboxypeptidases reveal a novel double-headed binding mode. J Mol Biol 350, 489498. Arolas, J. L., Vendrell, J., Avilés, F. X., and Fricker, L. D. (2007). Metallocarboxypeptidases: emerging drug targets in biomedicine. Curr Pharm Des 13, 349-366. Auld, D. S. (2004). 240. Carboxypeptidase A. In Handbook of proteolytic enzymes., A. J. Barrett, N. D. Rawlings, and J. F. Woessner Jr., eds. (London: Elsevier Academic Press), pp. 812-821. Bajzar, L., Manuel, R., and Nesheim, M. E. (1995). Purification and characterization of TAFI, a thrombin-activable fibrinolysis inhibitor. J Biol Chem 270, 14477-14484. Bedaiwy, M., and Casper, R. (2006). Diagnosis and treatment of endometriosis. In World Intellectual Property Organization (International Bureau, Mount Sinai Hospital, Toronto (CA)), November 9, 2006, Patent-No. WO 2006/116873A1. Bjork, I., and Lindahl, U. (1982). Mechanism of the anticoagulant action of heparin. Mol Cell Biochem 48, 161-182. Boffa, M. B., Bell, R., Stevens, W. K., and Nesheim, M. E. (2000). Roles of thermal instability and proteolytic cleavage in regulation of activated thrombin-activable fibrinolysis inhibitor. J Biol Chem 275, 12868-12878. Boffa, M. B., and Koschinsky, M. L. (2007). Curiouser and curiouser: recent advances in measurement of thrombin-activatable fibrinolysis inhibitor (TAFI) and in understanding its molecular genetics, gene regulation, and biological roles. Clin Biochem 40, 431-442. Boffa, M. B., Nesheim, M. E., and Koschinsky, M. L. (2001). Thrombin activable fibrinolysis inhibitor (TAFI): molecular genetics of an emerging potential risk factor for thrombotic disorders. Curr Drug Targets Cardiovasc Haematol Disord 1, 59-74. Boffa, M. B., Wang, W., Bajzar, L., and Nesheim, M. E. (1998). Plasma and recombinant thrombinactivable fibrinolysis inhibitor (TAFI) and activated TAFI compared with respect to glycosylation, thrombin/thrombomodulin-dependent activation, thermal stability, and enzymatic properties. J Biol Chem 273, 2127-2135. Bouma, B. N., and Mosnier, L. O. (2003). Thrombin activatable fibrinolysis inhibitor (TAFI) at the interface between coagulation and fibrinolysis. Pathophysiol Haemost Thromb 33, 375-381. Buelens, K., Hillmayer, K., Compernolle, G., Declerck, P. J., and Gils, A. (2008). Biochemical importance of glycosylation in thrombin activatable fibrinolysis inhibitor. Circ Res 102, 295301. Carter, W. J., Cama, E., and Huntington, J. A. (2005). Crystal structure of thrombin bound to heparin. J Biol Chem 280, 2745-2749. CCP4 (1994). The CCP4 suite : programs for protein crystallography. Acta Crystallogr sect D 50, 760-763. Ceresa, E., De Maeyer, M., Jonckheer, A., Peeters, M., Engelborghs, Y., Declerck, P. J., and Gils, A. (2007). Comparative evaluation of stable TAFIa variants importance of alpha-helix 9 and betasheet 11 for TAFIa (in)stability. J Thromb Haemost 5, 2105-2112. Ceresa, E., Van de Borne, K., Peeters, M., Lijnen, H. R., Declerck, P. J., and Gils, A. (2006). Generation of a stable activated thrombin activable fibrinolysis inhibitor variant. J Biol Chem 281, 15878-15883. Coll, M., Guasch, A., Aviles, F. X., and Huber, R. (1991). Three-dimensional structure of porcine procarboxypeptidase B: a structural basis of its inactivity. EMBO J 10, 1-9. 15 Do, Y. H., Gifford-Moore, D. S., Beight, D. W., Rathnachalam, R., Klimkowski, V. J., Warshawsky, A. M., and Lu, D. (2005). Inhibition of thrombin activatable fibrinolysis inhibitor by cysteine derivatives. Thromb Res 116, 265-271. Eaton, D. L., Malloy, B. E., Tsai, S. P., Henzel, W., and Drayna, D. (1991). Isolation, molecular cloning, and partial characterization of a novel carboxypeptidase B from human plasma. J Biol Chem 266, 21833-21838. Gabazza, E. C., Taguchi, O., Fujimoto, H., and Nagashima, M. (2006). TAFI inhibitors and their use to treat pulmonary fibrosis. In World Intellectual Property Organization (International Bureau, Schering AG, Berlin (DE), Mie University Graduate School of Medecine, Mie (JP), and Michael John Morser, San Francisco (CA; US)), April 20, 2006, Patent-No. WO 2006/041808 A2. Hendriks, D., Scharpé, S., van Sande, M., and Lommaert, M. P. (1989). Characterisation of a carboxypeptidase in human serum distinct from carboxypeptidase N. J Clin Chem Clin Biochem 27, 277-285. Hillmayer, K., Macovei, A., Pauwels, D., Compernolle, G., Declerck, P. J., and Gils, A. (2006). Characterization of rat thrombin-activatable fibrinolysis inhibitor (TAFI)--a comparative study assessing the biological equivalence of rat, murine and human TAFI. J Thromb Haemost 4, 2470-2477. Hooper, N. M. (1994). Families of zinc metalloproteases. FEBS Lett 354, 1-6. Hsu, M.-Y., Matsueda, G. R., and Tamura, J. K. (2007). Baboon TAFI polypeptides. In United States Patent 7189829 (United States, Bristol-Myers Squibb Company), Patent-No. Janin, J., and Chothia, C. (1990). The structure of protein-protein recognition sites. J Biol Chem 265, 16027-16030. Klement, P., Liao, P., and Bajzar, L. (1999). A novel approach to arterial thrombolysis. Blood 94, 2735-2743. Knecht, W., Willemse, J., Stenhamre, H., Andersson, M., Berntsson, P., Furebring, C., Harrysson, A., Hager, A. C., Wissing, B. M., Hendriks, D., and Cronet, P. (2006). Limited mutagenesis increases the stability of human carboxypeptidase U (TAFIa) and demonstrates the importance of CPU stability over proCPU concentration in down-regulating fibrinolysis. FEBS J 273, 778792. Koradi, R., Billeter, M., and Wüthrich, K. (1996). MOLMOL: A program for display and analysis of macromolecular structures. J Mol Graphics 14, 51-55. Mann, K. G., Jenny, R. J., and Krishnaswamy, S. (1988). Cofactor proteins in the assembly and expression of blood clotting enzyme complexes. Annu Rev Biochem 57, 915-956. Mao, S. S., Cooper, C. M., Wood, T., Shafer, J. A., and Gardell, S. J. (1999). Characterization of plasmin-mediated activation of plasma procarboxypeptidase B. Modulation by glycosaminoglycans. J Biol Chem 274, 35046-35052. Marx, P. F., Hackeng, T. M., Dawson, P. E., Griffin, J. H., Meijers, J. C., and Bouma, B. N. (2000). Inactivation of active thrombin-activable fibrinolysis inhibitor takes place by a process that involves conformational instability rather than proteolytic cleavage. J Biol Chem 275, 1241012415. Marx, P. F., Havik, S. R., Marquart, J. A., Bouma, B. N., and Meijers, J. C. (2004). Generation and characterization of a highly stable form of activated thrombin-activable fibrinolysis inhibitor. J Biol Chem 279, 6620-6628. Matsumoto, A., Itoh, K., and Matsumoto, R. (2000). A novel carboxypeptidase B that processes native -amyloid precursor protein is present in human hippocampus. Eur J Neurosci 12, 227238. Matsumoto, A., Itoh, K., Seki, T., Motozaki, K., and Matsuyama, S. (2001). Human brain carboxypeptidase B, which cleaves -amyloid peptides in vitro, is expressed in the endoplasmic reticulum of neurons. Eur J Neurosci 13, 1653-1657. Mosnier, L. O., and Bouma, B. N. (2006). Regulation of fibrinolysis by thrombin activatable fibrinolysis inhibitor, an unstable carboxypeptidase B that unites the pathways of coagulation and fibrinolysis. Arterioscler Thromb Vasc Biol 26, 2445-2453. 16 Navaza, J. (1994). AMoRe : an automated package for molecular replacement. Acta Crystallogr sect A 50, 157-163. Normant, E., Martres, M. P., Schwartz, J. C., and Gros, C. (1995). Purification, cDNA cloning, functional expression, and characterization of a 26-kDa endogenous mammalian carboxypeptidase inhibitor. Proc Natl Acad Sci USA 92, 12225-12229. Pallarès, I., Bonet, R., García-Castellanos, R., Ventura, S., Avilés, F. X., Vendrell, J., and GomisRüth, F. X. (2005). Structure of human carboxypeptidase A4 with its endogenous protein inhibitor, latexin. Proc Natl Acad Sci USA 102, 3978-3983. Pereira, P. J. B., Segura-Martín, S., Oliva, B., Ferrer-Orta, C., Avilés, F. X., Coll, M., Gomis-Rüth, F. X., and Vendrell, J. (2002). Human procarboxypeptidase B : three-dimensional structure and implications for thrombin-activatable fibrinolysis inhibitor (TAFI). J Mol Biol 321, 537-547. Rees, D. C., and Lipscomb, W. N. (1982). Refined crystal structure of the potato inhibitor complex of carboxypeptidase A at 2.5 Å resolution. J Mol Biol 160, 475-498. Refino, C. J., de Guzman, L., Schmitt, D., Smyth, R., Jeet, S., Lipari, M. T., Eaton, D., and Bunting, S. (2000). Consequences of inhibition of plasma carboxypeptidase B on in vivo thrombolysis, thrombosis and hemostasis. Fibrinol Proteol 14, 305-314. Reverter, D., Fernandez-Catalan, C., Baumgartner, R., Pfander, R., Huber, R., Bode, W., Vendrell, J., Holak, T. A., and Aviles, F. X. (2000). Structure of a novel leech carboxypeptidase inhibitor determined free in solution and in complex with human carboxypeptidase A2. Nat Struct Biol 7, 322-328. Schneider, M., Boffa, M., Stewart, R., Rahman, M., Koschinsky, M., and Nesheim, M. (2002). Two naturally occurring variants of TAFI (Thr-325 and Ile-325) differ substantially with respect to thermal stability and antifibrinolytic activity of the enzyme. J Biol Chem 277, 1021-1030. Silveira, A., Schatteman, K., Goossens, F., Moor, E., Scharpe, S., Stromqvist, M., Hendriks, D., and Hamsten, A. (2000). Plasma procarboxypeptidase U in men with symptomatic coronary artery disease. Thromb Haemost 84, 364-368. Taylor, F. B., and Bajzar, L. (2005). Treatment of sepsis with TAFI. In United States Patent (USA, Oklahoma Medical Research Foundation, Oklahoma City (OK; US), and McMaster University, Hamilton (CA)), January 4, 2005, Patent-No. US6,838,432B2. Valnickova, Z., Christensen, T., Skottrup, P., Thogersen, I. B., Hojrup, P., and Enghild, J. J. (2006). Post-translational modifications of human thrombin-activatable fibrinolysis inhibitor (TAFI): evidence for a large shift in the isoelectric point and reduced solubility upon activation. Biochemistry 45, 1525-1535. Valnickova, Z., Thogersen, I. B., Potempa, J., and Enghild, J. J. (2007). Thrombin-activable fibrinolysis inhibitor (TAFI) zymogen is an active carboxypeptidase. J Biol Chem 282, 30663076. Van Thiel, D. H., George, M., and Fareed, J. (2001). Low levels of thrombin activatable fibrinolysis inhibitor (TAFI) in patients with chronic liver disease. Thromb Haemost 85, 667-670. van Tilburg, N. H., Rosendaal, F. R., and Bertina, R. M. (2000). Thrombin activatable fibrinolysis inhibitor and the risk for deep vein thrombosis. Blood 95, 2855-2859. Vendrell, J., Querol, E., and Avilés, F. X. (2000). Metallocarboxypeptidases and their protein inhibitors. Structure, function and biomedical properties. Biochim Biophys Acta 1477, 284-298. Walsh, P. N., Rizza, C. R., Matthews, J. M., Eipe, J., Kernoff, P. B., Coles, M. D., Bloom, A. L., Kaufman, B. M., Beck, P., Hanan, C. M., and Biggs, R. (1971). -Aminocaproic acid therapy for dental extractions in haemophilia and Christmas disease: a double blind controlled trial. Br J Haematol 20, 463-475. Wang, X., Smith, P. L., Hsu, M. Y., Tamasi, J. A., Bird, E., and Schumacher, W. A. (2007). Deficiency in thrombin-activatable fibrinolysis inhibitor (TAFI) protected mice from ferric chloride-induced vena cava thrombosis. J Thromb Thrombolysis 23, 41-49. Willemse, J. L., and Hendriks, D. F. (2007). A role for procarboxypepidase U (TAFI) in thrombosis. Front Biosci 12, 1973-1987. Wiman, B. (1980). Affinity-chromatographic purification of human 2-antiplasmin. Biochem J 191, 229-232. 17 Zappacosta, F., Pessi, A., Bianchi, E., Venturini, S., Sollazzo, M., Tramontano, A., Marino, G., and Pucci, P. (1996). Probing the tertiary structure of proteins by limited proteolysis and mass spectrometry: the case of Minibody. Prot Sci 5, 802-813. 18 ACKNOWLEDGMENTS This study was supported by the following grants: BIO2007-68046, BIO2006-02668, BFU2006-09593, PSE-010000-2007-1, and the CONSOLIDER-INGENIO 2010 Project “La Factoría de Cristalización” (CSD2006-00015) from Spanish ministries; and 2005SGR00280 and 2005SGR01027 from the Generalitat de Catalunya. Additional funding was obtained by J.J.E. from the Danish National Science Research Council. L.S. and I.P. enjoyed Ph.D.-fellowships from the Spanish Ministry of Education and Science. M.S. and J.L.A. are, respectively, beneficiaries of the “Ramón y Cajal” and “Juan de la Cierva” Programs of the Spanish Ministry of Education and Science. We acknowledge the help provided by EMBL and ESRF synchrotron local contacts. Funding was provided by ESRF for data collection. Robin Rycroft and, specially, Josep Vendrell are thanked for helpful suggestions to the manuscript. 19 FIGURE LEGENDS Figure 1. Alignment of B-type MCPs. Sequence alignment of bovine, human, rat and mouse TAFI, human PCPB1 and porcine PCPB. The corresponding UniProt sequence database access codes and the percentage of sequence identity with human TAFI within overlapping residues are shown preceding the second and third blocks of sequences, respectively. Signal peptides are shown over yellow background. The TAFI activation cleavage site is indicated by red scissors. The traditional sequential numbering and the structure-based numbering of TAFI employed throughout the text are shown above and below each alignment block, respectively. The latter numbering was established for porcine PCPB to fit that of archetypal bovine CPA1 (Coll et al., 1991). This entails that the pro-domain is numbered separately (1A-95A) from the active enzyme moiety (4-308) and that there is a one-residue insertion after position 188 in B-type MCPs, here named 1889. TAFI starts with Phe7A and has three extra unique one-residue insertions after positions 56, 150 and 235 of the mature enzyme moiety with respect to porcine PCPB, which are numbered 567, 1501 and 2356, respectively. In addition, TAFI displays three extra residues at the end of the pro-domain, so that cleavage occurs at bond Arg98A-Ala4. Regular secondary structure elements for bovine TAFIa (helices as green cringles, 1-7; -strands as red arrows, 1-8; T1 and T2 for 1,4-turns of type I and II) are depicted above each sequence block. Identical residues in bovine and human TAFI are shown over blue background and those identical in all four sequences over magenta background. Positions reported to produce human TAFI or TAFIa variants with longer half-lives (Ceresa et al., 2007; Ceresa et al., 2006; Knecht et al., 2006; Schneider et al., 2002) are shown in green. Segments disordered in TAFIa are shown in red. Figure 2. Structure of TAFIa in its complex with TCI. (A) Richardson plot of the complex showing TAFIa in standard orientation with yellow -strands (1-8), green -helices (1-7) and the catalytic zinc ion as a red sphere. Segment 5-L57-7 is shown in orange and the TAFI exosite in magenta. The region of the proposed fibrinolysis switch is shown over gray background. TCI is shown for its NTD (light blue), linker (red) and CTD (navy blue). The disulfide bonds of TCI 20 are also shown. The N- and C-termini of both molecules are labeled. (B) Close-up view of (A) after a vertical rotation of ~90º showing the proposed fibrinolysis switch region of TAFIa (yellow) superimposed with the equivalent region of human CPB1 (green). TAFIa regular secondary structure elements are labeled. (C) Close-up view of (A) showing the TAFIa active site and the residues participating in the interaction with TCI CTD. (D) Close-up view of (A) centered on the interaction area of TAFIa with TCI NTD and the participating residues. 21 Table 1. Comparison of the activity of human and bovine TAFI. human TAFI Equation bovine TAFI Vmax Km Vmax Km (µM/min) (mM) (µM/min) (mM) Hanes 44.84 2.36 47.40 3.58 Eadie-Hofstee 44.65 2.35 44.33 3.14 Eisenthal-CornishBowden 44.96 2.44 44.61 3.16 44.99±1.19 2.35±0.20 47.84±3.67 3.88±0.85 44.86 2.38 46.05 3.44 Hyperbolic Regression Average values Kcat (min-1) Kcat/Km (min-1/mM) 160.21 164.46 67.32 47.81 The values for Km and Vmax were determined using the direct fit of the Michaelis-Menten equation employing 4 graphical methods. The data represent the enzyme-catalyzed reaction for 0.28µM TAFI. 22 Table 2. Interactions between TCI NTD and CTD with bovine TAFIa. CTD TAFIa Dist.(Å) Hydrogen bonds and polar interactions NTD TAFIa Dist.(Å) Hydrogen bonds and polar interactions Gly44I O Arg71 N1 3.40 Asn1I N2 Trp120 O 2.94 Glu46I O1 Glu163 N 2.77 Cys10I S Lys121 O 3.17 Gln53I N2 Ser244 O 3.34 Cys10I O Arg124 N 2.76 Gln53I O1 Leu249 N 2.87 Ser28I N Lys121 O 2.78 Lys55I N Ser246 O 3.28 Pro12I N Lys122 O 3.36 Lys55I N Leu247 O 3.04 Gly26I O Lys121 N 3.12 Trp73I O Arg71 N2 2.98 Thr29I O Lys122 O 2.77 Trp73I O Arg127 N1 3.29 Residues making van-der-Waals interactions Leu74I O His69 N1 3.10 Val4I Trp73 Leu74I O Glu72 O2 2.92 Val4I Trp120 Leu74I O Arg127 N1 2.83 Pro12I Asp123 Leu74I OT His196 N1 3.30 Ser28I Lys122 Leu74I OT Glu270 O2 2.59 Leu34I Leu280 Leu74I OT Ser197 O 3.26 Leu34I Met125 Leu74I N Tyr248 O 2.88 Residues making van-der-Waals interactions Gly44I Met125 Leu74I Leu247 Val72I Phe279 Trp73I Ile164 Trp73I Tyr248 23 Table 3. Crystallographic data. ____________________________________________________________________________ Space group / cell constants (a and c, in Å) P3221 / 84.20, 128.90 Wavelength (Å) 0.8726 No. of measurements / unique reflections Resolution range (Å) (outermost shell)a 874,530 / 57,962 48.1 – 1.70 (1.79 – 1.70) Completeness (%) Rr.i.m. (= Rmeas) b / Rp.i.m. 93.3 (95.5) b 0.099 (0.611) / 0.025 (0.190) Average intensity (<[<I> / (<I>)]>) 20.6 (4.0) B-Factor (Wilson) (Å2) / Average multiplicity 18.6 / 15.1 (9.2) Resolution range used for refinement (Å) 48.1 – 1.70 No. of reflections used (test set) 57,265 (695) Crystallographic Rfactor (free Rfactor) c 0.156 (0.171) d No. of protein atoms / solvent molecules / ions 2,991 / 358 / 1 (Zn2+), 2 acetates, 5 sulfates Rmsd from target values bonds (Å) / angles (°) bonded B-factors (main chain / side chain) (Å2) Average B-factors for protein atoms (Å2) 0.015 / 1.35 0.96 / 2.30 19.6 Main-chain conformational angle analysis Residues in favored regions / outliers / all residues 351 / 1 / 362 _____________________________________________________________________________ a Values in parentheses refer to the outermost resolution shell. Rr.i.m.= hkl(nhkl /[nhkl-1] 1/2)i |Ii(hkl) - <I(hkl)>| / hkli Ii(hkl) and Rp.i.m.= hkl(1/[nhkl-1]1/2)i |Ii(hkl) - <I(hkl)>| / hkli Ii(hkl). b c Crystallographic Rfactor = hkl ||Fobs| - k |Fcalc|| / hkl |Fobs|; free Rfactor, same for a test set of reflections not used during refinement. d Including atoms in alternate conformation.