Hydatid Disease of the Liver.ppt
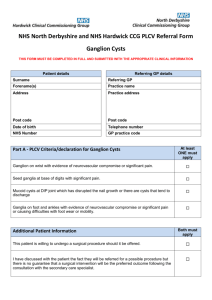
advertisement

Hydatid Cysts Disease of the Liver Treatment Options Surgical Vs. Percutaneous Drainage Presented By: Dr.Doaa Al-Qaidy Hose officer Contents: • Case presentation. • Introduction. • Basic Information. • Hydatid disease in human: Liver Hydatid disease: Clinical presentation, management options and complication. • Conclusion. Case • A twenty-five year old female presented with intermitted upper abdominal pain for two years. She is a villager and there was history of weight loss and off/on history of fever. There was no previous hospitalization and surgical interventions. There was history of keeping sheep at home. On clinical examination patient was a fibrile vital were stable, systematic review was normal. • Abdominal Examination: 4X4 cm mass firm in consistency in Epigastric area moves with respiration slight tenderness in epigastric area. There were no visible pulsation or penstaltic movements on it. US abdomen&CTAbdomen were both in favor of Hydatid cyst involving left lobe of Liver completely. According to clinical history and image finding Hydatid cyst was suspected. Introduction: • Hydatid disease is a worldwide zoonosis produced by the larval stage of the Echinococcus tapeworm . • The two main types of hydatid disease are caused by E granulosus and E multilocularis. • E granulosus is commonly seen in the great grazing regions of the world—particularly the Mediterranean region, Africa, South America, the Middle East, Australia, and New Zealand— and is the most frequently encountered type of hydatid disease in humans. Life Cycle of E granulosus Hydatid Cyst Structure • The hydatid cyst has three layers: (a) the outer pericyst, composed of modified host cells that form a dense and fibrous protective zone; (b) the middle laminated membrane, which is acellular and allows the passage of nutrients; (c) the inner germinal layer, where the scolices (the larval stage of the parasite) and the laminated membrane are produced. • Daughter vesicles (brood capsules) are small spheres that contain the protoscolices and are formed from rests of the germinal layer. Before becoming daughter cysts, these daughter vesicles are attached by a pedicle to the germinal layer of the mother cyst. At gross examination, the vesicles resemble a bunch of grapes. Hydatid Disease in Humans Hydatid disease involves the liver in approximately 75% of cases, the lung in 15%, and other anatomic locations in 10% Clinical presentation : The clinical features are highly variable. The spectrum of symptoms depends on the following: • Involved organs • Size of cysts and their sites within the affected organ or organs • Interaction between the expanding cysts and adjacent organ structures, particularly bile ducts and the vascular system of the liver • Symptoms due to pressure usually take a long time to manifest, except when they occur in the brain . • Most symptomatic cysts are larger than 5 cm in diameter. • Bacterial infection of cysts and spread of protoscolices and larval material into bile ducts or blood vessels • Immunologic reactions such as asthma, anaphylaxis, or membranous nephropathy secondary to release of antigenic material Hepatic Disease • The right lobe is the most frequently involved portion of the liver. • Once in the human liver, cysts grow to 1 cm during the first 6 months and 2–3 cm annually thereafter, depending on host tissue resistance. Clinical presentation of liver disease: Work Up • Generally, routine laboratory tests do not show specific results. • In patients with rupture of the cyst in the biliary tree, marked and transient elevation of cholestatic enzyme levels occurs, often in association with hyperamylasemia and eosinophilia (as many as 60%). • Indirect hemagglutination test and enzyme-linked immunosorbent assay are the most widely used methods for detection of anti-Echinococcus antibodies (immunoglobulin G [IgG]).These tests give false positive results in cases of schistosomiasis and nematode infestations that is why they are not specific for diagnosing hydatidosis. Imaging Studies: • • • • Plain radiography Ultrasound examination CT scaning MRI Management Options • Medical . • Surgery. • PAIR. Medical therapy: • • Indications: Chemotherapy is indicated in patients with primary liver or lung cysts that are inoperable (because of location or medical condition), patients with cysts in 2 or more organs, and peritoneal cysts. Chemotherapeutic agents: Two benzimidazoles are used, albendazole and mebendazole. Albendazole is administered in several 1-month oral doses (10-15 mg/kg/d) separated by 14-day intervals. The optimal period of treatment ranges from 3-6 months, with no further increase in the incidence of adverse effects if this period is prolonged. Mebendazole is also administered for 3-6 months orally in dosages of 40-50 mg/kg/d. • Contraindications: Early pregnancy, bone marrow suppression, chronic hepatic disease, large cysts with the risk of rupture, and inactive or calcified cysts are contraindications. A relative contraindication is bone cysts because of the significantly decreased response. • Outcome : Response rates in 1000 treated patients were that 30% had cyst disappearance (cure), 30-50% had a decrease in the size of the cyst (improvement), and 20-40% had no changes. Also, younger adults responded better than older adults. PAIR • This technique, performed using either ultrasound or CT guidance, involves aspiration of the contents via a special cannula, followed by injection of a scolicidal agent for at least 15 minutes, and then reaspiration of the cystic contents. The cyst is then filled with isotonic sodium chloride solution. Perioperative treatment with a benzimidazole is mandatory (4 d prior to the procedure and 1-3 mo after). • The cysts should be larger than 5 cm in diameter and type I or II according to the Gharbi ultrasound classification of liver cysts • Indications: Inoperable patients; patients refusing surgery; multiple cysts in segment I, II, and III of the liver; and relapse after surgery or chemotherapy are indications for the PAIR technique. • Contraindications: Early pregnancy, lung cysts, inaccessible cysts, superficially located cysts (risk of spillage), type II honeycomb cysts, type IV cysts, and cysts communicating with the biliary tree (risk of sclerosing cholangitis from the scolecoidal agent). • Outcome: The reduced cost and shorter hospital stay associated with PAIR compared to surgery make it desirable. The risk of spillage and anaphylaxis is considerable, especially in superficially located cysts, and transhepatic puncture is recommended. Sclerosing cholangitis (chemical) and biliary fistulas are other risks. Experience is still limited. Surgical Management • Indications: 1-Large liver cysts with multiple daughter cysts; superficially located single liver cysts that may rupture (traumatically or spontaneously). 2-liver cysts with biliary tree communication or pressure effects on vital organs or structures. 3-infected cysts . 4-cysts in lungs, brain, kidneys, eyes, bones . Choice of surgical technique: • 1-Radical surgery (total pericystectomy or partial resection, if possible), • 2-Conservative surgery (open cystectomy), or simple tube drainage for infected and communicating cysts are choices for surgical technique. The more radical the procedure, the lower the risk of relapses but the higher the risk of complications. • Concomitant treatment with benzimidazoles (albendazole or mebendazole) has been reported to reduce the risk of secondary echinococcosis. Treatment is started 4 days preoperatively and lasts for 1 month. • Contraindications: General contraindications to surgical procedures (eg, extremes of age, pregnancy, severe preexisting medical conditions); multiple cysts in multiple organs; cysts that are difficult to access; dead cysts; calcified cysts; and very small cysts are contraindications. Complications: 1-All the usual complications related to the surgical procedure and anesthesia 2-Related to the parasite Recurrence • Metastasis • Infection • Spillage and seeding (secondary echinococcosis) Allergic reaction or anaphylactic shock 3-Related to the medical treatment Hepatotoxicity • Anemia • Thrombocytopenia • Alopecia • Embryotoxicity • Teratogenicity. Complications , cont. 4-Related to PAIR • Hemorrhage • Mechanical damage to other tissue • Infections • Allergic reaction or anaphylactic shock • Persistence of daughter cysts • Sudden intracystic decompression leading to biliary fistulas 5-Related to scolicidal agents - Chemical sclerosing cholangitis Conclusion: • Many hydatid cysts remain asymptomatic, even into advanced age. Parasite load, the site, and the size of the cysts determine the degree of symptoms. • The liver is the most common organ involved, followed by the lungs. These 2 organs account for 90% of cases of echinococcosis. • Surgery remains the main Treatment of the hydatied liver disease , PAIR technique still promising. • Patient education about the prevention of this zoonotic infection . References: Articles: • Hydatid Disease: Radiologic and Pathologic Features and Complications , by Iván Pedrosa, MD,Radiographics,2004. • Surgical treatment of liver hydatid disease,by ali azer, department of general surgery , Baskent university, Turky 2006. • Surgical treatment of hydatid cysts of the liver,drainage versus omentoplasty,annuls of hepatology , 2005. • Percutaneous Treatment of hydatid liver diseases , 2009. Web sites: http://emedicine.medscape.com/articl e/178648-followup#a2651 .