Eating Disorders' Assessment and MNT.doc
advertisement

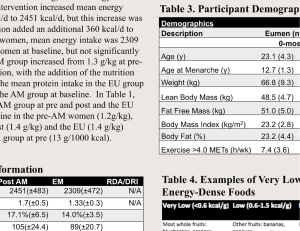
Nutrition in Eating Disorders Nutrition Assessment and Medical Nutrition Therapy Nutrition assessment: Diet history. Biochemical (laboratory) assessment. Metabolic assessment. Anthropometric assessment. Diet history: A) Assessment of energy intake: - It is important to prevent overfeeding or underfeeding at the beginning of their nutritional rehabilitation. - Patients with eating disorders usually Overestimate their food and energy intake, so using food models and asking detailed questions about the serving size are very beneficial methods in determining accurate energy intake. - In Bulimia Nervosa energy intake can unpredictable and challenging because of: 1) The caloric content of a binge can not be predicted and measured easily. (Binge: To consume large amounts of food uncontrollably within a short time period). 2) The degree of caloric absorption after a purge. 3) The extent of caloric restriction between binge episodes. - Many Bulimic patients have a misconception and assume mistakingly that the calories consumed in a binge is completely eliminated after purging, however a study of the caloric content of food ingested and purged in a feeding laboratory revealed that approximately 50% of energy consumed during a binge is retained. B) Assessment of macronutrient consumption: - There is a tendency to avoid fatty foods in the diet. - Many Anorexic patients follow a vegetarian diets affecting both the quality and the quantity of protein consumption. - The majority of Anorexic patients adopt the vegetarian diet during the course of their illness, and thus it is a covert method to limit their food and caloric consumption, particularly fat. - It is important to determine whether the adoption of vegetarianism predated the development of Anorexia Nervosa and whether the family members also follow a vegetarian diet in order to set realistic guidelines for the planning of medical nutritional therapy and to identify the real causes of developing the eating disorder and the actual disease-related eating miss-behaviors. C) Assessment of micronutrient consumption: - Micronutrient intake parallels macronutrient intake: Inadequate caloric intake, limited variety in the diet, and poor food group representation result in inadequate vitamin and mineral consumption in Anorexia Nervosa and Bulimia Nervosa patients. - For example: a) Constantly restricting fat results in a higher risk in developing essential fatty acid and fat-soluble vitamins deficiency. b) Eliminating a food group such as meat causes Fe and vitamin B12 deficiency. D)Assessment of eating behaviors and eating attitudes: 1) Eating attitudes: a) Food aversions. b) Patients categorize their food as safe, risky, forbidden food. c) Magical thinking. d) Binge trigger foods. e) Ideas on appropriate amounts of food. 2) Eating behaviors: a) Ritualistic behaviors. b) Unusual food combinations. c) Atypical seasoning of food. d) Excessive and atypical use of non-caloric sweeteners. e)Atypical use of eating utensils. 3) Eating habits: a) Intake pattern: (1) Number of meals and snacks. (2) Time of day meals and snacks are consumed. (3) Duration of feedings. (4) Eating environment – where and wit whom. (5) How consumed – sitting or standing. b) Avoidance of particular food groups. c) Variety of foods consumed. d) Fluid intake – restricted or excessive. Laboratory Assessment: - The body's compensatory mechanisms are remarkable and thus laboratory abnormalities may not be observed until the illness is far advanced even though Anorexic patients show marked cachexia. - Such adaptive phenomena in chronic starvation results in insignificant alterations in visceral protein at the expense of somatic protein which causes wasting e.g. Serum albumin levels are generally within normal limits but may be masked by dehydration. ( somatic protein status: measure of the protein in the skeletal muscle). ( Visceral protein status: measure of all other proteins in organs, viscera, serum, and blood cells). - Anorexia Nervosa patients initially present with elevated serum cholesterol levels despite the typically low fat diet, however this not warrant the continuation of low fat and cholesterol diet. - If hyperlipidemia predated the development of the disease or if there is a strong family history of hyperlipidemia, the patient should be reassessed After Weight Restoration and a period of Weight Stabilization. - Low blood levels of essential fatty acids may contribute to the physical and mental symptoms of the disorder. - An accurate lipid profile can be obtained only after a period of Dietary Stabilization. - Low serum glucose results from a deficit of precursors needed for gluconeogenesis and glucose production. Metabolic Assessment: Vitamin and Mineral Deficiencies: - Hypercarotenemia is caused by: a) Mobilization of lipid stores. b) Catabolic changes caused by weight loss. c) Metabolic stress. Thus, it is not related to excessive dietary intake o f carotenoids. Normalization of serum carotene occurs during the course of nutrition rehabilitation. - Clinical and biochemical findings of true deficiency diseases are uncommon even though the diet is deficient in many nutrients. The catabolic state in these patients could be the cause of such a phenomenon causing a decreased need for micronutrients. - Iron deficiency anemia is uncommon because: a) Decreased requirement secondary to amenorrhea in women. b) The overall catabolic state. c) The accurate diagnosis could be masked by masked by hemoconcentration that is caused by dehydration in early treatment, so once refeeding is initiated, hemoglobin concenttratin may decrease from baseline values. - Zinc deficiency occurs secondary to inadequate energy intake, avoidance of red meat , and the adoption of vegetarian diet. - Osteoporosis and osteopenia are are common in males and females and caused by: a) low estrogen levels in females and low testosterone levels in males. b) weight loss. c) Ca, Mg, and vitamin D deficiencies. Fluid and Electrolytes Balance: - Vomiting may result in dehydration, hypokalemia, and alkalosis with hypochloremia. - Laxative use may result in hypokalemia. - Diuretic use may result in hypokalemia and dehydration. - Urine concentration is decreased, and urine output is increased in semistarvation. - Edema may occur in response to malnutrition and refeeding. - Depletion of glycogen and lean tissue is accompanied by obligatory water loss that reflects characteristic hydration ratios. Energy Expenditure: - Resting energy Expenditure (REE) is characteristically low. - The hypometabolic state is caused by: a) Weight loss. b) Decreased lean body mass. c) Energy restriction. d) Decreased leptin levels. - Resistance to weight gain is common. It is caused by: a) Excessive increase in REE resulting from refeeding. b) Anxiety level. c) Abdominal pain. d) Hyperactivity. e) Cigarette smoking. - Factors affecting rate of weight gain in Anorexia Nervosa: 1) Fluid balance: a) Polyuria in semistarvation. b) Edema --> (1) Starvation. (2) Refeeding. c) Hydration ratios in tissues. 2) Metabolic rate a) REE. b) Postprandial energy expenditure. 3) Energy cost of tissue gained: More energy is required to gain fat (adipose tissues) versus lean tissues, but weight gain may be a mix of both. 4) Previous obesity. 5) Physical activity. - Patients with Bulimia Nervosa can have unpredictable metabolic rates. Dietary restraints between binge episodes may place bulimic patients in a state of semistarvation. However, binge eating followed by purging can increase the metabolic rate secondary to a preabsorptive release of insulin, which activates the sympathetic nervous system. - Baseline and follow-up assessment of REE is clinically useful throughout the course of nutritional rehabilitation. Anthropometric Assessment: - Anorexia Nervosa patients have protein-energy malnutrition characterized by significantly depleted adipose and somatic protein stores, but a relatively intact visceral protein compartment. - The goal of the assessment of anthropometric measurement is the restoration of fat and fat-free mass. - Body fat measurement: 1) Underwater weighing. 2) DEXA scan (dual-energy x-ray absorptiometry) that is equipped with body composition software. However, these two measurements not generally available in an office or clinic setting. 3) Skin-fold measurement (triceps, biceps, subscapular, and suprailiac crest). 4) BIA (bioelectrical impedance analysis) is more readily available. However, shifts in intracellular and extracurricular fluid compartments in patients with sever eating disorders may affect the accuracy of body fat measurement. To improve the validity of BIA measurement in anorexia Nervosa patients, the measurement should be: a) In the morning before ingestion of food and liquid. b) The use of a reclining chair that is always reclined to the same position to prevent differential pooling of fluids. - Body weight should be assessed and monitored routinely. - In Bulimia Nervosa patients, the short term goal should be weight maintenance. - Rehydration and replenished glycogen stores contribute to weight gain during the first few days of refeeding. Thereafter, weight gain results from increased lean and fat stores. - Although total body fat normalizes after short-term weight restoration, it may not be normally distributed e.g. It was found that body fat disproportionally deposits around waist and abdominal cavity in the weight-restored adult female Anorexia Nervosa patients. - Variables that may affect the type of tissue gained include: 1) Stage of growth and development. 2) Degree of baseline malnutrition. 3) Duration of illness. 4) Duration of weight restoration. 5) Gender. 6) Genetics. 7) Physical activity. 8) The type and rate of refeeding. - If the patient is hospitalized, a daily preprandial, early morning weight should be obtained. - On a n outpatient basis, a gowned weight should be obtained on the same scale, at approximatly the same time of day, at least once a week in early treatment. - Before weigh in, the patient should void (use the bathroom). - Patients may resort to deceptive tactics ( water loading, hiding heavy objects on their person, and withholding urine and bowel movements) to make a mandated weight goal. - Catch-up growth should be calculated for adolescents with stunted heights. - Baseline and follow-up measurement should be routinely monitored during the course of the treatment. Medical Nutrition Therapy: Anorexia Nervosa: Goals: 1) Correction of biologic and psychological indices of malnutrition. 2) Restoration of body fat. 3) Normalization of eating patterns, eating behaviors, and hunger/satiety cues. Guidelines for Medical Nutrition Therapy: 1) Caloric prescription: a) Initial weight gain (1) Start at 30-40 kcal/kg/day ( approximately 1000-1600 kcal/day). (2) Assess risk for refeeding syndrome. b) Controlled weight gain phase (1) Increase prescription in small, progressive increments to promote expected rate of controlled weight gain (e.g. 2-3 lb/wk for inpatients, 0.5-1 lb/wk for outpatients). (2) Late treatment: 70-100 kcal/kg/day Females: 3000-4000 kcal/day Males: 4000-4500 kcal/day (3) If patient requires a higher kcal prescription, evaluate for vomiting, discarding food, increased exercise, increased motor activity, increased REE/ DIT (diet-induced thermogenesis). c) Weight maintenance phase (1) Adults: 40-60 kcal/kg/day (2) Ongoing growth and development in children and adolescents: 40-60 kcal/kg/day. 2) Macronutrients: a) Protein (1) Minimum intake = RDA in g/kg ideal body weight (2) 15-20% kcal (3) High biologic value sources b) Carbohydrate (1) 50-55% kcal (2) Encourage insoluble fiber for treatment of constipation c) Fat (1) 25-30% kcal (2) Encourage small increases in fat intake until goal can be obtained (3) Provide source of essential fatty acids 3) Micronutrients a) 100% RDA multivitamin with minerals supplement b) Note that iron-containing preparations may aggravate constipation Bulimia Nervosa: 1) Caloric prescription for weight maintenance: a) Provide 1500-1600 kcal/day diet if patient is hypometabolic. b) Provide DRI for energy if metabolic rate is normal. c) Monitor body weight and adjust caloric prescription for weight maintenance. d) Avoid weight reduction diets until eating patterns and body weight are stabilized. 2) Macronutrients a) Protein (1) Minimum intake = RDA in g/kg ideal body weight (2) 15-20% kcal (3) High biologic value sources b) Carbohydrate (1) 50-55% kcal (2) Encourage insoluble fiber for treatment of constipation c) Fat (1) 25-30% kcal (2) Encourage small increases in fat intake until goal can be obtained (3) Provide source of essential fatty acids 4) Micronutrients a) 100% RDA multivitamin with minerals supplement b) Note that iron-containing preparations may aggravate constipation