Internal Transport Chapter 43
advertisement

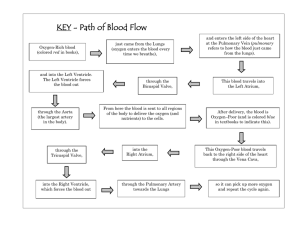
Internal Transport Chapter 43 KEY CONCEPTS • A circulatory system typically consists of blood, a heart, and a system of blood vessels or spaces through which blood circulates Learning Objective 1 • Compare and contrast internal transport in animals with no circulatory system, those with an open circulatory system, and those with a closed circulatory system Internal Transport • Diffusion • • in small, simple invertebrates (sponges, cnidarians, flatworms) Specialized circulatory systems • • in larger animals blood, heart, blood vessels or spaces No Circulatory System Fig. 43-1a, p. 920 Gastrovascular cavity Pharynx Mouth (b) Fig. 43-1b, p. 920 Interstitial Fluid • Tissue fluid between cells • • in all animals Brings oxygen, nutrients in contact with cells Open Circulatory System • Found in arthropods, most mollusks • Blood flows into a hemocoel • bathing tissues directly Open Circulatory Systems Stomach Ventricle Atrium Gills Fig. 43-2a, p. 921 Artery Ostia Tubular heart Fig. 43-2b, p. 921 Closed Circulatory System • Found in all vertebrates • • and some invertebrates Blood flows through a continuous circuit of blood vessels Closed Circulatory System Dorsal vessel Ventral vessel Contractile blood vessels Lateral vessels Fig. 43-3, p. 921 KEY CONCEPTS • Arthropods and most mollusks have an open circulatory system in which blood bathes the tissues directly • Some invertebrates and all vertebrates have a closed circulatory system in which blood flows through a continuous circuit of blood vessels Vertebrate Circulatory System 1 • Muscular heart • • pumps blood into arteries, capillaries, veins Transports • nutrients, oxygen, wastes, hormones Vertebrate Circulatory System 2 • Helps maintain • • fluid balance, pH, body temperature Defends body against disease Learn more about open and closed circulatory systems by clicking on the figures in ThomsonNOW. KEY CONCEPTS • The vertebrate circulatory system transports nutrients, oxygen, wastes, and hormones; helps maintain fluid balance, appropriate pH, and body temperature; and defends the body against disease Learning Objective 2 • Compare the structure and function of plasma, red blood cells, white blood cells, and platelets Plasma • Water and salts • Substances in transport • Plasma proteins • • • albumins globulins fibrinogen Red Blood Cells (Erythrocytes) • Transport oxygen and carbon dioxide • Produce hemoglobin • red pigment that binds with oxygen White Blood Cells (Leukocytes) • Defend body against disease organisms • Lymphocytes and monocytes • • agranular white blood cells Neutrophils, eosinophils, basophils • granular white blood cells Platelets • Patch damaged blood vessels • Release substances essential for blood clotting Vertebrate Blood Whole blood Plasma Cell components Plasma proteins Lipoproteins Albumins Globulins White blood cells (leukocytes) Fibrinogen Clotting proteins Water Salts Dissolved gases Hormones Glucose Wastes 7 µm Granular leukocytes Agranular leukocytes 1 to 2 µm Red blood cells Platelets (erythrocytes) Fig. 43-4a, p. 923 Learn more about the composition of vertebrate blood by clicking on the figures in ThomsonNOW. Learning Objective 3 • What is the sequence of events involved in blood clotting? Blood Clotting • Damaged cells and platelets • • Prothrombin is converted to thrombin • • release substances that activate clotting factors converts fibrinogen to insoluble protein (fibrin) Fibrin forms long threads • make up webbing of clot Blood Clotting 1 Injury to blood vessel Blood flow 2 Wall of vessel contracts Blood flow decreases 3 Platelets adhere 4 More permanent to collagen fibers clot forms of damaged vessel wall Platelet Blood flow plug Blood flow decreases ceases Fig. 43-5a, p. 924 1. Injury to blood vessel Blood flow 2. Wall of vessel contracts Blood flow decreases 3. Platelets adhere to collagen fibers of damaged vessel wall Blood flow decreases 4. More permanent clot forms Blood flow Platelet ceases plug Stepped Art Fig. 43-5a, p. 924 Prothrombin Damaged cells and platelets release substances that activate clotting factors Prothrombin activator Ca2+ Thrombin Fibrinogen Ca2+ Fibrin threads (clot) Fig. 43-5b, p. 924 Learning Objective 4 • Compare the structure and function of different types of blood vessels, including arteries, arterioles, capillaries, and veins Blood Vessels 1 • Arteries • • carry blood away from the heart Veins • return blood to the heart Blood Vessels 2 • Arterioles • • • constrict (vasoconstriction) dilate (vasodilation) Arterioles regulate blood pressure and distribution of blood to tissues Blood Vessels 3 • Capillaries • • thin-walled exchange vessels allow materials to transfer between blood and tissues Blood and Lymphatic Vessels Vein Lymphatic Artery Venule Arteriole Lymph node Capillary bed Capillaries (a) Movement of interstitial fluid Lymph capillaries Fig. 43-6a, p. 926 Outer coat (connective tissue) VEIN Smooth muscle Endothelium ARTERY Outer coat (connective tissue) Endothelium CAPILLARY (b) Fig. 43-6b, p. 926 Fig. 43-6c, p. 926 A Capillary Network Precapillary sphincter Metarteriole True capillaries Arteriole (a) Sphincters closed Venule Fig. 43-7a, p. 927 Precapillary sphincter Metarteriole True capillaries Arteriole (b) Sphincters open Venule Fig. 43-7b, p. 927 Learning Objective 5 • Trace the evolution of the vertebrate cardiovascular system from fish to mammal The Vertebrate Heart • One or two atria • • receive blood One or two ventricles • pump blood into arteries The Vertebrate Heart The Fish Heart • One atrium and ventricle • single circuit of blood flow Atrium Sinus venosus Veins from the body Valve Ventricle Valve Aorta (a) Fishes Fig. 43-8a, p. 928 Terrestrial Vertebrates • Circulatory systems separate oxygen-rich from oxygen-poor blood • Allows higher metabolic rate • supports active terrestrial lifestyle Amphibian Heart • Two atria and one ventricle • Blood flows through a double circuit • oxygen-rich blood partly separated from oxygen-poor blood Sinus venosus Pulmonary vein Veins from the body Pulmonary artery Aorta Partition separating atria Valves Ventricle Conus Atria (b) Amphibians Fig. 43-8b, p. 928 Reptile Heart • Most have a wall that partly divides the ventricles • minimizing mixing of oxygen-rich and oxygenpoor blood Pulmonary vein Aorta Sinus venosus Veins from the body Pulmonary artery Right atrium Ventricle Left atrium Semilunar valves Conus Incomplete partition of the ventricle (c) Reptiles Fig. 43-8c, p. 928 Bird and Mammal Hearts • Four-chambered hearts • Separate oxygen-rich blood from oxygenpoor blood Left atrium AV valve Veins from the body Pulmonary artery Right atrium Aorta Ventricles Semilunar valves (d) Birds and mammals Fig. 43-8d, p. 928 KEY CONCEPTS • During the evolution of terrestrial vertebrates, adaptations in circulatory system structures separated oxygen-rich from oxygen-poor blood • The four-chambered hearts and double circuits of endothermic birds and mammals completely separate oxygenrich blood from oxygen-poor blood Learning Objective 6 • Describe the structure and function of the human heart • Include the heart’s conduction system in your answer The Human Heart 1 • Pericardium encloses heart • Valves prevent backflow of blood • • • right atrioventricular (AV) valve (tricuspid valve) between right atrium and ventricle mitral valve between left atrium and ventricle semilunar valves guard exits from heart The Human Heart 2 • Intercalated discs • • Sinoatrial (SA) node (pacemaker) • • join cardiac muscle fibers initiates each heartbeat Specialized electrical conduction system • coordinates heartbeats The Human Heart Superior vena cava Right pulmonary arteries Pulmonary valve Right atrium Pulmonary veins Tricuspid valve Aorta Left pulmonary arteries Pulmonary artery Pulmonary veins Left atrium Mitral valve Aortic valve Chordae tendineae (“heartstrings”) Papillary muscles Right ventricle Left ventricle Inferior vena cava Interventricular septum Aorta Fig. 43-9, p. 929 Insert “The human heart” anatomy_heart_v2.swf Learn more about heart anatomy by clicking on the figure in ThomsonNOW. Heart Conduction System SA node or pacemaker Left atrium Right atrium AV node Purkinje fibers Right ventricle AV bundle Left ventricle Right and left branches of AV bundle Fig. 43-10a, p. 930 Nucleus 25 µm Intercalated discs Fig. 43-10b, p. 930 Intercalated discs Z-line Mitochondria 1 µm Fig. 43-10c, p. 930 Insert “Cardiac conduction” cardiac_conduction.dcr See cardiac conduction by clicking on the figure in ThomsonNOW. Learning Objective 7 • Trace the events of the cardiac cycle • Relate normal heart sounds to these events Cardiac Cycle • One complete heartbeat • Contraction occurs during systole • Period of relaxation is diastole Heart Sounds • Closing of AV valves • • • at beginning of ventricular systole makes low-pitched “lub” sound Closing of semilunar valves • • at beginning of ventricular diastole makes short, loud “dup” sound Cardiac Cycle Superior vena cava Aorta Right atrium Tricuspid valve Inferior vena cava Pulmonary artery Semilunar valves Pulmonary vein Left atrium Mitral valve 1 Atrial systole. Atria 5 Period of falling pressure. Blood flows from veins into relaxed atria. Right Left ventricle ventricle contract, pushing blood through open tricuspid and mitral valves into ventricles. Semilunar valves are closed. 2 Beginning of Heart sounds ventricular systole. Ventricles contract; pressure within ventricles increases and closes tricuspid and mitral valves, causing first heart sound. 4 Beginning of ventricular diastole. Pressure in relaxing ventricles drops below that in arteries. Semilunar valves snap shut, causing second heart sound. 3 Period of rising pressure. Semilunar valves open when pressure in ventricle exceeds that in arteries. Blood spurts into aorta and pulmonary artery. Fig. 43-11, p. 931 Watch the cardiac cycle by clicking on the figure in ThomsonNOW. Learning Objective 8 • Define cardiac output • Describe how it is regulated • Identify factors that affect it Cardiac Output (CO) • Equals stroke volume times heart rate • Stroke volume depends on • • venous return neural messages and hormones (especially epinephrine and norepinephrine) Starling’s Law of the Heart • The more blood delivered to the heart by the veins, the more blood the heart pumps Heart Rate • Regulated mainly by the nervous system • Influenced by hormones and body temperature Factors in Cardiac Output Stressors and other stimuli Increases Decreases Hypothalamus Cardiac centers in the medulla Brain Increased venous return Adrenal Sympathetic Parasympathetic Increase glands nerves nerves in body (accelerator nerves) (vagus) temperature Ephinephrine Norepinephrine and Norepinephrine Acetylcholine X STROKE VOLUME = HEART RATE CARDIAC OUTPUT Fig. 43-12, p. 932 Learning Objective 9 • What factors determine and regulate blood pressure? • Compare blood pressure in different types of blood vessels Blood Pressure 1 • The force blood exerts against inner walls of the blood vessel • Is greatest in the arteries • Decreases as blood flows through the capillaries Blood Pressure 2 • Depends on • • • • cardiac output blood volume resistance to blood flow Peripheral resistance to blood flow • caused by blood viscosity, friction between blood and blood vessel wall Blood Pressure Blood pressure Blood volume Blood viscosity Blood flow Peripheral resistance Cardiac output Vasoconstriction Blood pressure depends on blood flow and resistance to that flow. Fig. 43-14a, p. 936 Fig. 43-14b, p. 936 Area Velocity Blood pressure varies in different types of blood vessels Pulse pressure Total cross-sectional area (cm2) of the vascular bed Vena cavae Diastolic pressure Veins Venules Capillaries Arterioles Arteries Aorta Blood pressure (mm Hg) Systolic pressure Fig. 43-14b, p. 936 Nervous Control 1 • Baroreceptors • • sense increase in blood pressure send messages to cardiac and vasomotor centers in medulla of brain Nervous Control 2 • Cardiac center • • Vasomotor center • • stimulates parasympathetic nerves that slow heart rate inhibits sympathetic nerves that constrict blood vessels Blood pressure is reduced Sympathetic and Parasympathetic Actions Parasympathetic neuron 1 Acetylcholine 2 Acetylcholine receptor Plasma membrane 5 K+ K + channel G-protein 3 4 K+ Cardiac muscle Fig. 43-13a, p. 933 Sympathetic neuron 1 Norepinephrine 2 -adrenergic receptor 6 G protein Ca2+ Plasma membrane Adenylyl cyclase 4 3 Ca2+ ATP cAMP Cardiac muscle Gate open 5 Protein Kinase Fig. 43-13b, p. 933 Hormonal Control • Angiotensin II • • raises blood pressure Aldosterone • • helps regulate salt excretion affects blood volume and blood pressure Insert “Measuring blood pressure” blood_pressure.dcr Learn more about determining blood pressure by clicking on the figures in ThomsonNOW. Learning Objective 10 • Trace a drop of blood through the pulmonary and systemic circulations • Name in sequence each structure through which it passes Blood Circulation • Pulmonary circulation • • connects heart and lungs Systemic circulation • connects heart and tissues Systemic and Pulmonary Circulation Systemic circulation Capillary network Superior vena cava Brain Pulmonary artery Carotid artery Pulmonary artery Pulmonary circulation Left lung Right lung Aorta LA RA RV Pulmonary vein Inferior vena cava LV Pulmonary vein To lower parts of the body Capillary network Fig. 43-16, p. 937 Pulmonary Circulation • From right ventricle to pulmonary arteries to lungs • Through pulmonary capillaries in the lung • Return by pulmonary vein to left atrium Systemic Circulation 1 • Left ventricle to the aorta • Aorta branches into arteries • • leading to body organs Through capillary networks within organs Systemic Circulation 2 • From capillaries into veins • From veins to the superior vena cava or inferior vena cava • Returns to right atrium Principle Arteries and Veins Carotid arteries Jugular veins Right subclavian artery Left subclavian vein Aortic arch Left pulmonary vein Left pulmonary artery Superior vena cava Axillary artery Left ventricle Right ventricle Right lung Liver Renal vein Inferior vena cava Common iliac vein Femoral vein Renal artery Kidney Abdominal aorta Inferior mesenteric artery Common iliac artery External iliac artery Femoral artery Fig. 43-17, p. 938 Venous Blood Flow (a) Resting condition. (b) Muscles contract. (c) Muscles relax. Fig. 43-15, p. 936 Special Circulations • Coronary arteries • • supply heart muscle with blood Hepatic portal system • circulates nutrient-rich blood through the liver Cardiovascular Disease 500 µm (a) Normal coronary artery. 500 µm (b) This artery is almost completely blocked with atherosclerotic plaque. p. 934 Learn more about systemic and pulmonary circulation by clicking on the figures in ThomsonNOW. Learning Objective 11 • Describe the structure and functions of the lymphatic system The Lymphatic System • Collects interstitial fluid, returns it to blood • important in homeostasis of fluids • Defends body against disease • Absorbs lipids from digestive tract Lymphatic System Structures 1 • Lymphatic vessels conduct lymph • Lymph • clear fluid formed from interstitial fluid Lymphatic System Structures 2 • Thoracic duct and right lymphatic duct • • • in shoulder region return lymph to blood circulatory system Lymph nodes • • small masses of tissue filter bacteria, harmful materials out of lymph Lymphatic System Right lymphatic duct Right subclavian vein Tonsil Cervical lymph nodes Left subclavian vein Thymus Thoracic duct Axillary lymph nodes Spleen Lymphatics of breasts Superficial lymphatics of upper limb Superficial lymphatics of lower limb Fig. 43-18, p. 939 Lymph Capillaries Arteriole Venule Red blood cells Valve Plasma Connective tissue fibers Capillary bed Lymph Plasma Fig. 43-19, p. 939 Blood and Interstitial Fluid Arterial end of capillary Venous end of capillary Blood pressure (+40) Osmotic pressure of plasma (-28) Osmotic pressure of interstitial fluid (+3) (40 + 3) - 28 = +15 Net filtration Blood pressure (+15) Osmotic pressure of plasma (-28) Osmotic pressure of interstitial fluid (+3) (15 + 3) - 28 = -10 Net absorption Fig. 43-20, p. 940 Learn more about the human lymphatic system by clicking on the figure in ThomsonNOW. KEY CONCEPTS • The lymphatic system helps maintain fluid homeostasis by returning interstitial fluid to the blood