‒ The Renal System Learner Resource 1 Teacher answers
advertisement

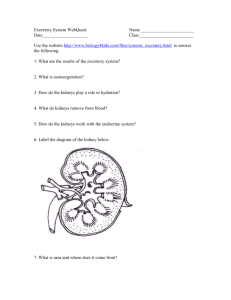
Learner Resource 1 ‒ The Renal System Teacher answers Excretion is the removal of waste products of metabolism. List some waste products that need to be excreted: Carbon dioxide, urea/ammonia/uric acid, bile salts/bilirubin, water How are carbon dioxide and urea produced by the body:Carbon dioxide: Respiration: during decarboxylation of pyruvate to produce acetyl-CoA and by decarboxylation reactions during the Krebs cycle Urea: By enzymatic conversion of the ammonia produced in deamination of amino acids Excess amino acids cannot be stored by the body so are converted into urea. The amino acid is deaminated by removal of its amine group, which is converted to NH3. This in turn is converted to urea in the ornithine cycle and excreted by the kidneys. The rest of the amino acid is converted to a keto acid and can be respired to produce energy or stored. Version 1 Kidney functions and malfunctions 1 © OCR 2016 Where are the following substances excreted from your body:Carbon dioxide: In the lungs Urea : In the kidney Salts: In the kidney and in sweat glands Excess water: In the kidney, some loss also by sweat and from the lungs As well as excreting urea, the kidneys also excrete other substances including excess salts, hormones, and drugs. The kidneys also regulate the salt/water balance of the body by controlling the water and salt concentration of the blood. This process is termed osmoregulation. The waste product produced by the kidneys is urine. This passes down the ureters into the bladder. The kidneys receive blood from the renal artery and once the blood has been filtered by the kidneys, it leaves via the renal vein. Version 1 Kidney functions and malfunctions 2 © OCR 2016 The Structure of the Urinary System Draw and label a diagram showing the structure of the urinary system. Include the following labels: vena cava aorta kidney renal artery renal vein ureter bladder Version 1 Kidney functions and malfunctions 3 © OCR 2016 The structure of the Kidney Draw and label a diagram showing the cross section through a kidney. Include the following structures: cortex capsule medulla pelvis renal artery renal vein Version 1 Kidney functions and malfunctions 4 © OCR 2016 Within the cortex and medulla lie the nephrons or kidney tubules. These are the functional units of the kidneys. They are thin walled tubes, about 2–4 cm long. They produce urine. Each kidney consists of approximately one million nephrons, surrounded by blood capillaries. Each nephron consists of a capsule connected to a long coiled tube. A knotted mass of coiled capillaries, called a glomerulus lies inside each tube. The nephron is the functional unit of the kidney. Each one consists of: a cup-shaped Bowman’s capsule Immediately below the capsule is a twisted region called the proximal convoluted tubule followed by the long hair-pin like loop of Henle, which runs deep into the medulla and then back into the cortex this is followed by another twisted region called the distal convoluted tubule This is joined to the collecting duct which carries urine through the medulla to the pelvis of the kidney Give a brief outline of how the nephrons produce urine. Some of the water and small solutes of the blood are filtered out of the blood into the fluid which will become the urine. Solutes are then selectively reabsorbed into the blood according to the body’s needs. More or less water is reabsorbed into the blood, according to the body’s needs, before the urine finally leaves the kidney to be stored in the bladder. 1. Ultrafiltration High blood pressure is built up in the glomerulus which forces the liquid part of the blood, i.e. plasma into the Bowman’s capsule. This process is called ultrafiltration. The liquid entering the nephron is called the filtrate. What causes high blood pressure in the glomerulus? The large diameter of the lumen of the afferent arteriole, compared with the small diameter of the lumen of the efferent arteriole. List substances that are contained within the filtrate: Water, ions, small molecules including urea, glucose and amino acids. Hormones, alcohol and other drugs or metabolic by-products of drugs. Version 1 Kidney functions and malfunctions 5 © OCR 2016 Which parts of the blood do not enter the filtrate? Why not? Cells, large molecules (including most proteins). They are too big to pass through the fenestrations in the endothelium of the capillary, the mesh of collagen and glycoprotein in the basement membrane and the filtration slits of the epithelium of the Bowman’s capsule. Draw a labelled diagram to show the structure of the filter:- The first layer is the wall or endothelium of the capillary. In the glomerulus this single layer of cells with small holes through which plasma can pass. The basement membrane -its mesh-like structure acts as a filter during ultrafiltration. The second cell layer is the wall of the Bowman’s capsule. The epithelial cells in this wall are called podocytes They have foot-like processes and do not fit tightly together so have gaps between them allowing the filtrate to pass. Version 1 Kidney functions and malfunctions 6 © OCR 2016 2. Selective Reabsorption Up to 70% of water and solutes are removed from the plasma as it passes through the glomerulus. These include some useful substances such as amino acids and glucose, these must be reabsorbed back into the body. This process is called selective reabsorption. All the glucose, amino acids, vitamins and many Na+ and Cl- ions are actively transported out of the proximal tubule and back into the blood. The uptake of these substances means that the blood in the capillaries surrounding the nephron now has a relatively high solute concentration. So large amounts of water passes from the filtrate back to the blood in the proximal tubule by osmosis How are the cells of the proximal convoluted tubule adapted for the process of selective reabsorption? Microvilli increase surface area Co-transporter proteins Na/K pumps Large numbers of mitochondria Version 1 Kidney functions and malfunctions 7 © OCR 2016 The Loop of Henle Its function is to create an area of high solute concentration deep in the medulla. Draw a labelled diagram of the loop of Henle. Include the following labels: descending limb ascending limb interstitial region collecting duct The ascending limb is more permeable to salts and less permeable to water As filtrate moves up Na and Cl ions move out passively and then actively This cause water to move out of the descending limb by osmosis. Thus filtrate become more concentrated as it passes down the descending limb The solute conc. in any part of the loop is always lower in the ascending limb than the descending limb This mechanism is called the counter current multiplier mechanism. As the collecting ducts pass through the medulla to the pelvis they pass through this region of high solute concentration So water is also drawn out of the collecting ducts due to osmosis resulting in far more concentrated urine. Version 1 Kidney functions and malfunctions 8 © OCR 2016 The Distal tubule Reabsorbs Na+ ions through coupled secretion of H+ or K+ ions into the filtrate. By acidifying the urine the distal convoluted tubule plays an important role in acid-base balance. The movement of these ions can be regulated to ensure their correct level is maintained. The distal tubule is normally relatively impermeable to water. However in the presence of antidiuretic hormone (ADH) its permeability to water increases permitting concentration of the urine. secretes ammonium ions and some drugs Release of Wastes The urea, excess ions, excess water and toxins such as alcohol that are not reabsorbed, are not needed by the body. These continue to flow out of the nephron, into the collecting ducts, into the ureter and down to the bladder as urine. Osmoregulation The concentration of the blood must be kept constant. The body achieves this by varying the amount of water lost from the body in urine. When do you produce large quantities of dilute urine? When the concentration of the blood is low / when the blood is dilute / when the water potential of the blood is high When do you produce small quantities of concentrated urine? When the concentration of the blood is high / when the blood is concentrated / when the water potential of the blood is low Version 1 Kidney functions and malfunctions 9 © OCR 2016 The amount of water lost from the body in urine is controlled by the hypothalamus and pituitary gland, situated in the brain. If the blood is too concentrated, meaning its water potential is too hypothalamus , the at the base of the brain, detects this change, and causes the release a hormone called blood low Anti-diuretic . In the kidney it causes more pituitary gland to hormone. This hormone travels to the kidney in the water to be reabsorbed back into the blood. This occurs because the cells lining the nephron become more permeable to water, allowing more water to pass back into the blood. The result is that a smaller volume of more formed and the blood becomes less concentrated urine is concentrated. In your own words, explain what happens if the blood becomes too dilute. Credit correct science and coherent explanation On a separate sheet of paper, draw a flow diagram to explain how the process of osmoregulation controls the water content of blood. Now answer the following questions:How does ADH affect the kidneys on a cellular level? Increasing the permeability of the membranes of the cells in the wall of the collecting duct by causing aquaporins to be inserted in the membrane. Version 1 Kidney functions and malfunctions 10 © OCR 2016 What are aquaporins and how are they inserted and removed from cell membranes of the collecting duct? Membrane-spanning channel proteins that allow water to pass through the membrane. Aquaporins are stored in vesicles within the cell allowing them to be inserted rapidly into the cell surface membrane by fusion of these vesicles. Fusion of vesicles is triggered by a signal transduction cascade involving the second messenger cAMP in response to binding of ADH to cell surface receptors. ADH also has a longer-term effect in increasing the expression of the aquaporin gene, thus increasing the total number of aquaporin proteins in the cell. As well as osmoregulation, the kidneys perform other homeostatic functions:Renin (angiotensinogenase) – released by kidney when blood volume is low. It has four effects: It constricts blood vessels to raise blood pressure. It stimulates the thirst reflex It causes the secretion of ADH so causing an increase in the reabsorption of water in the collecting ducts. It causes aldosterone to be released by the adrenal glands. This causes more sodium to be reabsorbed in the distal tubules (so more water will also be reabsorbed by osmosis), raising blood pressure. Erythropoietin – a hormone produced by the kidneys which causes more red blood cells to be produced by the bone marrow when oxygen levels in the blood are low. OCR Resources: the small print OCR’s resources are provided to support the teaching of OCR specifications, but in no way constitute an endorsed teaching method that is required by the Board, and the decision to use them lies with the individual teacher. Whilst every effort is made to ensure the accuracy of the content, OCR cannot be held responsible for any errors or omissions within these resources. © OCR 2016 - This resource may be freely copied and distributed, as long as the OCR logo and this message remain intact and OCR is acknowledged as the originator of this work. OCR acknowledges the use of the following content: Please get in touch if you want to discuss the accessibility of resources we offer to support delivery of our qualifications: resources.feedback@ocr.org.uk Version 1 Kidney functions and malfunctions 11 © OCR 2016