oxide-oxygen inhalation
advertisement
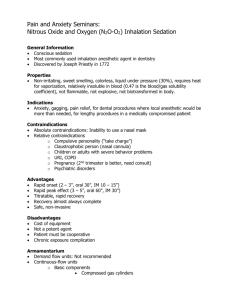
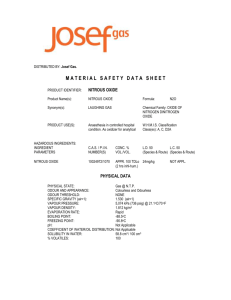
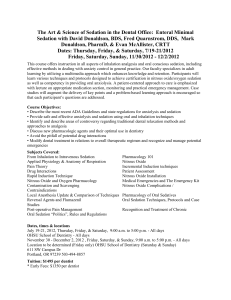
OXIDE -OXYGEN INHALATION Dr.zameer pasha Sedation • The provision of adequate anxiety control is an integral part of the practice of dentistry. • It is of fundamental importance that the level of sedation must be such that the patient remains conscious, and is able to both understand and respond to verbal commands. • Conscious sedation: • A minimally depressed level of consciousness, that retains patient’s ability to maintain an airway independently and respond appropriately to physical stimulation and verbal command • Deep sedation: a controlled state of depressed consciousness, accompanied by partial loss of protective reflex, including inability to respond to verbal commands • General anesthesia : control state of unconsciousness accompanied by complete loss of protective reflexes including inability to maintain air way independently and respond to verbal commands • Goals for sedation to control behavior to allow procedure to be completed successfully. • • Kids under age 5 or 6 (chronologically or developmentally) may require deep sedation Pre- sedation assessment • • • • • • A fully recorded medical history. Blood pressure. Weight, if recorded. ASA status. A dental history. A conscious sedation and general anaesthetic history. • • • • Dental treatment plan. The selected conscious sedation technique. Any individual patient requirements. Provision of pre- and post-operative written instructions provided before treatment. • Written consent for conscious sedation and dental treatment. TYPES / ROUTES OF ADMINISTRATION • Inhalation • Nitrous oxide • Desflurane • Sevofuraine • Oral • Diazepam • Triazolam • Intramuscular • Ketamine • Midazolam • Intravenous • Midazolam • propofol • Conscious Sedation for Children • Nitrous oxide/oxygen is usually the technique of choice for conscious sedation of pediatric dental patients • Nitrous Oxide is a very quick acting inhaled sedation medicine that decreases discomfort and anxiety. • Sometimes called “laughing gas” • Often given at the dentists office • Nitrous Oxide is a sweet-smelling, colorless gas. • It is heavier than air or oxygen History of N2O • 1793 - Joseph Priestly invented N2O • In 1844, Dr. Gardner Colton • Initially used as an anesthetic agent in 1844. by Dr. Horace Wells • Roberts in 1990 and dr. kevin allen demonstrated relative analgesia on child patient Pharmacokinetic properties Onset • • • • • Anywhere from a few seconds up to 3-5 minutes Crosses the blood-brain barrier rapidly Elimination Rapid elimination Unchanged with exhalation from the lungs Do not hold a child close to your face while they are “waking up” No significant metabolism by the liver or kidneys • Not stored in the tissues Fear Reduction & N2O • One group treated with behavior management only; • other group with behavior management and N2O. • Dental treatment of highly fearful children is carried out more successfully with N2O during the first few sessions. • N2O is thus a valuable aid for making highly fearful children treatable quickly. • When highly anxious children are treated with nitrous oxide for a number of consecutive sessions, their anxiety remains significantly lower during a following control period, even without use of nitrous oxide. Four Stages of Anesthesia • Analgesia • patient is conscious • reflexes are intact • Delerium • Surgical Anesthesia • Respiratory Paralysis • In analgesia stage, the patient is conscious, has all vital reflexes intact, can communicate and cooperate with the dentist, and quickly returns to a normal state following a few minutes of oxygenation. N2O Should Be Used To: • Ease fears and anxieties • Aid in the treatment of special patients • Increase tolerance for longer appointments • Raise the pain reaction threshold N2O Should Not Be Used To: • uncontrolled behavior • Control pain by replacing local anesthesia • Replace poor techniques of behavior management Administration of N2O • 5 - 6 liters O2 • Increase N2O gradually; watch for stages of analgesia • Maintenance about 40% -50% • Reduce N2O with long procedures • Record N2O levels in the chart • 3 - 5 minute O2 flush • Rapid induction technique • 1. Open both tanks (O2 and N2O) • 2. Turn the On/Off switch to On • 3. Adjust the green (O2) and blue (N2O) levers to administer a 50/50 mixture of oxygen and Nitrous Never turn on the gases until the mask is sealed on the patients face! … • Begin with a 20/80 mix of N2O and O2 and titrate to achieve desired level of sedation/anxiolysis • Nitrous oxide may be administered to a maximum of 60% Remember the patient is not “asleep” • Patient should appear calm and relaxed Administration of N2O/O2 Titration is an important skill in administering nitrous oxide. Titration is a method of administering a drug in incremental amounts until a desired endpoint is reached. If done properly, the patient does not receive more of the drug than is necessary. . Administration of N2O/O2 Advantages of N2O titration • Only the amount of drug required by the patient is given. • Allows for individual biovariability • Uncovers idiosyncratic reactions early • Minimizes negative experiences with over sedation Potential side effects of nitrous oxide • Detachment / disassociation from environment • Dreaming, hallucinating, or sexual fantasizing • Out-of-body experiences • Floating and/or flying • Physical body movements may become restless, combative, sluggish • Inability to move, communicate, or keep mouth open • Words may be slurred or repeated; incoherent sentences Potential side effects of nitrous oxide • Humming or vibrating sounds that progressively worsen • Fits of uncontrolled laughter • Patient may experience: • Drowsiness • Dizziness / Light headedness / spinning sensations • Diaphoresis • Nausea / vomiting • Fixed eyes • Uncomfortable body warmth • Unconsciousness Contraindications for use of N2O/O2 sedation • N2O rapidly replaces N2 in air filled spaces in the body causing expansion of those spaces; therefore, N2O/O2 should not be used in patients with: • Pneumothorax • Middle ear occlusion/surgery • Recent (within 3 weeks) craniotomy/pneumoencephalography • Increased intracranial pressure • Intraocular injury/surgery (injected gas may last up to 10 weeks) • Maxillofacial injuries • Intestinal obstruction • Cystic fibrosis Contraindications for use of N2O/O2 sedation • • • • • • • • • • Current upper respiratory tract infection Chronic obstructive pulmonary diseases Vitamin B12 deficiency Psychological impairment Phobic individuals Bleomycin therapy Current psychotropic drug use Current or recovering drug use/addiction First trimester of pregnancy Any facial injury which would prevent use of the mask Note: Asthma is not a contraindication Potential biohazards of N2O for health professionals • No direct evidence suggests any causal relationship between chronic low-level exposure to N2O and potential biologic effects. • The following preventive measures to reduce or eliminate trace gas contamination are encouraged: • Operate a delivery system with scavenging capabilities, accurate flow meter, adequate vacuum, and a variety of mask sizes. • Maintain a ventilation system to include vent exhaust to outside and fresh air exchange when possible. • Maintain an adequate suction system – ensure vacuum, use appropriate size mask, discourage patient talking. • Inspect cylinder attachments, lines, hosing, and reservoir bag for leaks. • Calibrate flow meters every 2 years.