Renal Excretion
advertisement

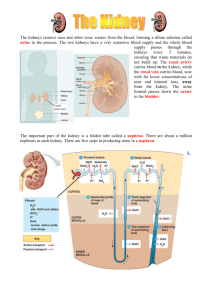
• If you knew there was poison hidden in your house, you would surely do everything possible to find and remove that poison. • If you didn't, you and your family would slowly die. • How would you find and then remove it? • You would probably figure out a system of searching and removing. • That is what the excretory system does!! 1. Filters the blood 2. Removes wastes from the blood 3. Keeps the amount of water and salts in the blood constant 4. Helps to regulate Blood Pressure Humans will die if they lose about 12% of their body water. The threat of desiccation is the most important problem confronting terrestrial life. How do we control our loss of water? 1. Multiple layers of dead, keratinized skin cells 2. Drink and eat moist foods 3. Nervous and hormonal mechanisms control thirst 4. Behaviour: (ie: stay out of intense heat) 5. Kidneys and other excretory organs help conserve water. Water loss can be considerable: a person in a 38oC temperature will lose 1 Litre of H2O/hour. We acquire most of our water in our food and drink, and obtain a smaller amount by dehydration synthesis and as a by-product of cellular respiration. We lose water by urinating, defecating, sweating, and breathing. The Excretory System is made up of the kidneys, liver, lungs, and skin. Each plays a role in excretion. Skin: sweat with water, salts, heat and some urea Lungs: excretes carbon dioxide, water, and heat Liver: gluconeogenesis – makes urea as a byproduct Intestines: excretes certain heavy metals Kidneys: the main excretory organ. Excrete toxins, drugs, wastes (urea…), and water. KIDNEY Kidney: • Bean-shaped • 10 cm long • Lower, dorsal part of the abdomen •Blood enters the kidney via the renal artery, is cleaned, and leaves the kidney in the renal vein The kidneys account for less than 1% of the weight of the human body, but they receive about 20% of the blood pumped with each heartbeat. Renal cortex Renal cortex renal medulla Renal cortex renal medulla renal pelvis Renal cortex renal medulla renal pelvis Renal pyramid Renal cortex renal medulla renal pelvis Renal pyramid Ureter CROSS SECTION OF KIDNEY KIDNEY Ureter: Waste fluid made in the kidney exits through a duct called a ureter. Moves the urine to the bladder via peristalsis URETER KIDNEY Bladder: stores the urine An average bladder can hold a maximum of 1.5 to 2 cups of urine. When full, the BLADDER sphincter muscles control the release of urine from the bladder URETER KIDNEY Urethra: when the sphincter relaxes, the urethra carries the urine outside the body. 20 cm in males URETER 4 cm in females BLADDER Females are more prone to infections of the urinary system. URETHRA The kidneys perform a number of homeostatic functions, as they are the chief regulators of our internal environment: 1. Regulates blood volume and osmotic balance by excreting or conserving water as the situation demands. 2. Regulates the ionic balance of the blood by controlling the excretion of inorganic salts (especially sodium). 3. Regulates Blood pH by excreting excess acids or base 4. Excretes toxic metabolic by-products such as urea, ammonia, uric acid, and creatine (a product of muscle activity). Nitrogen wastes are a by-product of protein metabolism. When proteins are turned into glucose during gluconeogenesis, ammonia is made. Because ammonia is very toxic and must be diluted as it travels around the body, however, terrestrial animals usually need to conserve water. What do we do? The liver converts the ammonia to urea, which is then transported to the kidneys, where it is concentrated and excreted out of the body as urine. This takes a lot of energy. The functional unit of the kidney is the NEPHRON, which consists of a renal tubule and its associated blood vessels. Each kidney contains approximately 1 million nephrons, which represents approximately 80km of tubules. Water, urea, salts, and other small molecules in the blood flow from the capillaries into the renal tubules, where the fluid is now called FILTRATE. The epithelial cells that line the renal tubule adds and removes things from the filtrate to eventually form URINE. From the 1100 to 2000L of blood that flows through the human kidneys each day, the nephron processes about 180L of filtrate, but excretes only ~1.5L of urine. The rest of the filtrate, including ~99% of the water, is reabsorbed into the blood. filtrate blood 1. Bowman’s Capsule: this cup shaped receptacle is the blind end of the renal tubule, which receives filtrate from the blood. It encloses a ball of capillaries called the glomerulus. 2. The proximal convoluted tubule (PCT): most of the important things (nutrients, water, salt…) are reabsorbed from the PCT. 3. The ascending and descending loop of Henle: a lot of salt and water are reabsorbed from Loop of Henle. water water salt salt 4. The distal convoluted tubule (DCT): the blood dumps things it wants to get rid of into the DCT so it can be removed in the urine. acids drugs 5. The collecting duct collects filtrate from many tubules and pass the urine into the renal pelvis. Water and urea are also reabsorbed here. water urea 1. Afferent Arteriole: this arteriole enters the bowman’s capsule from the renal artery . Renal artery Renal vein 2. Glomerulus: the capillaries of the glomerulus are porous and very twisted up. They sit within the Bowman’s capsule. Renal artery Renal vein Bowman’s Capsule 3. Efferent Arteriole: this arteriole leaves the bowman’s capsule. The blood is very hypertonic as most of the plasma has left the blood. The blood carries RBC, WBC, platelets and blood proteins. Renal artery Renal vein 4. Peritubular Capillaires: these are the capillaries that surround the Proximal and Distal convoluted tubules. Renal artery Renal vein 5. Vasa Recta: these are the capillaries that surround the Loop of Henle. Renal artery Renal vein The Nephron has 4 main functions: 1. Pressure Filtration: the blood pressure forces water and solutes through the pores of the glomerulus into the Bowman’s capsule. The holes in the glomerulus are small, so they are permeable to water and small solutes, but not to blood cells or blood proteins. The filtrate contains a mixture of solutes such as salts, nutrients, water and other small molecules. At this point, the concentration of substances in the blood plasma is equal to that of the filtrate. salts, nutrients (glucose, fatty acids, glycerol, nucleotides, amino acids), water, hormones, antibodies, water soluble vitamins, penicillin and other drugs, histamines, nitrogenous wastes (urea, uric acid…) and other small molecules. salts, nutrients (glucose, fatty acids, glycerol, nucleotides, amino acids), water, hormones, antibodies, water soluble vitamins, penicillin and other drugs, histamines, nitrogenous wastes (urea, uric acid…) and other small molecules. Composition of Plasma, and Glomerular Filtrate Urea Glucose Amino acids Water Plasma 0.03 0.10 0.05 52.0 Filtrate 0.03 0.10 0.05 52.0 Salts (ie: Na+, Cl-) 0.9 0.9 Protein RBC, WBC, Platelets 8.0 Lots None None 2. Selective Reabsorption: since filtration is nonselective, the body MUST make sure that the important molecules are returned to the blood plasma as soon as possible. Nearly all of the nutrients (esp. sugar), salts and water are reabsorbed. This happens at the PCT and it is a very selective process. There are a lot of mitochondria in the cells of the PCT. Why? This costs ENERGY!! WHAT IS REABSORBED? : 70% of the water, and 75% of the salts, glucose, amino acids, and other nutrients move back into the blood. The positive sodium ions are actively transported into the interstitial fluid and the negative chlorine ions follow passively, and finally, water follows by osmosis. The glucose, amino acids, and other nutrients are actively transported into the blood. Lots of ATP required!! Recall that osmosis is the movement of water (from [High] to [Low])across a selectively permeable membrane. This movement occurs whenever two solutions separated by a membrane differ in total solute concentration or osmolarity. When two solutions differ: The one with the greater concentration solutes (salt, urea) is HYPEROSMOTIC The one with the more dilute solution is HYPOOSMOTIC Hyperosmotic of Hypo-osmotic (watery) Hyperosmotic Remember: Water always moves towards a hyperosmotic environment. SALT SUCKS!! Changes in the body fluids are controlled by a variety of regulatory mechanisms, usually involving negative feedback. The control of water gain/loss is called OSMOREGULATION. 3. Water Reabsorption: water reabsorption occurs mainly at the loop of henle and in the collecting duct. The nephron pumps out salt and urea in these areas to make the blood and medulla extremely hyperosmotic. Water then moves back in to the blood by osmosis. It is important to note that the blood in the vasa recta moves in the OPPOSITE DIRECTION that the filtrate is moving. This allows the nephron to create a hyperosmotic environment around the descending loop of henle. So we’ll talk about the ascending Loop of Henle 1st. The ASCENDING LOOP OF HENLE: This part of the loop of henle is NOT PERMEABLE to water, but the salt can move. So, the NaCl passively and actively moves out of the tubule and into the blood and the medulla of the kidney. This creates a very HYPERTONIC solution in the blood. As the filtrate moves towards the DCT, most of the salt has left and the filtrate becomes more and more dilute. The DESCENDING LOOP OF HENLE: The loop of henle continues the reabsorption of water as the filtrate moves from the cortex and down into the concentrated medulla. The epithelium of this portion of the renal tubule is permeable to water, but not very permeable to salt and other solutes. Lots of WATER moves into the HYPERTONIC blood (created at the ascending loop) by osmosis as it follows the salt. As a result of this great loss of water, the filtrate becomes more and more concentrated. The COLLECTING DUCT: Water is also reabsorbed here. The epithelium of this duct is permeable to water and urea. As the duct moves down into the VERY HYPERTONIC medulla, the filtrate loses more and more water by osmosis as it moves back into the blood. This loss of water concentrates the urea in the filtrate, and because there is so much UREA in the collecting duct, some of it diffuses down its concentration gradient and back into the blood and medulla. The kidney is made up of two sections: the cortex and the medulla. The medulla is HYPEROSMOTIC as it has high concentrations of the solutes NaCl and urea. renal medulla HYPERTONIC renal cortex 4. Secretion: if the blood still needs to rid itself of other ions and waste products (hydrogen ions, ammonia, potassium ions), it will secrete them into the Distal Convoluted Tubule (DCT). This is a very selective process that involves both active and passive transport. Lots of mitochondria in the DCT too! ATP required!!! REVIEW OF NEPHRON: http://www.youtube.com/watch?v=glu0dzK4dbU Composition of Plasma, Glomerular Filtrate, and Urine (g/100 ml of fluid). Plasma Filtrate Final Urine % Reclaimed Urea Glucose Amino acids Water 0.03 0.10 0.05 52.0 0.03 0.10 0.05 52.0 Salts (ie: Na+, Cl-) 0.9 0.9 Protein RBC, WBC, Platelets 8.0 Lots None None 1.8 None None 1.0 50% 100% 100% 99% < 0.9-3.6 99.5% None None None None If the blood is ACIDIC, 2 things will happen: HCO3H+ 1. The bicarbonate ions are actively transported back into the blood. The HCO3- is an important buffer which will join with H+ to remove it from the solution. 2. The blood will also secrete hydrogen ions into the filtrate so we will pee it out. If you are dehydrated, the kidneys can excrete a small, concentrated volume of urine and reabsorb the majority of water from the filtrate. You will have very little dark yellow urine. If you have consumed an excessive amount of fluid, the kidneys can excrete a large, dilute volume of urine, with very little water being reabsorbed from the filtrate. You will have lots of pale yellow urine. How do we maintain the proper amount of water in our bodies? It is controlled homeostatically with 2 hormones are ADH and Aldosterone. FIRST HORMONE: ANTIDIURETIC HORMONE (ADH) This hormone controls water reabsorption with a negative feedback cycle. The hypothalamus makes ADH and it is stored and released from the posterior pituitary gland. It is released in response to an increase in the osmolarity of the blood (very concentrated blood) when you are dehydrated (inadequate intake of water). When you have low blood volume (high osmolarity), the osmoreceptor cells in the hypothalamus triggers the posterior pituitary to release ADH. ADH increases the permeability of the DCT and collecting ducts to water. This causes more water to be reabsorbed and ultimately increases blood volume (amount of blood). At the same time, the removal of water from the filtrate increases the concentration of the urine. You urinate less and it will be dark yellow. When you have high blood volume and low osmolarity, sensors in the heart signal the hypothalamus to cause a reduction of the amounts of ADH in the blood. This decreases the amount of water that is reabsorbed into the blood, and large quantities of a more dilute urine are produced. This is a negative feedback cycle, because as the osmolarity of the blood is reduced (blood volume increases) less ADH will be secreted. Alcohol can perturb water balance by inhibiting the release of ADH, causing excessive loss of water in the urine and dehydrating the body. This leads to the symptoms of a hangover. Which is why you should always drink a lot of water when drinking alcohol. This keeps you hydrated. Second Hormone: ALDOSTERONE There is tissue surrounding the afferent arteriole called the juxtaglomerular apparatus (JGA) which measures Blood Pressure. • When the BP drops, or if the [Na+ ] in the blood is too low (due to diarrhea, a severe injury…), the JGA releases an enzyme called RENIN. • The liver makes a protein called ANGIOTENSIN which is always circulating around the blood. • RENIN activates angiotensin. The active form of ANGIOTENSIN does two things: 1. It stimulates the adrenal gland to release the hormone ALDOSTERONE. Aldosterone tells the DCT to reabsorb lots of Na+, and water follows the sodium by osmosis. This increases the amount of water in the blood, which increases the BP. 2. It also causes VASOCONTRICTION of the arterioles, which also raises blood pressure. Low blood pressure is bad because there is not enough pressure to filter the blood properly. This makes the kidneys less efficient at ridding the body of drugs and toxins. High blood pressure is bad because the glomerulus can burst and then we would see blood and blood proteins in the urine.