oral microbiology - viral diseases
advertisement
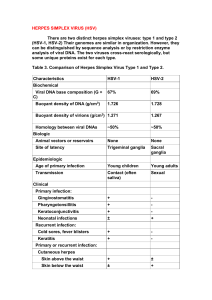
OROFACIAL VIRAL INFECTIONS Dr. Saleem Shaikh Introduction Viruses are some of the smallest microrganisms (100-300 nm). Consist of a core [genome] containing either a DNA or a RNA surrounded by a protein shell [caspid] Many viruses have the property of latency and may reside in the tissue asymptomatically for the entire life Approximately 90% of the adults harbour viruses that have been acquired as a result of infection during earlier life. Oral tissues are a frequent site for viral lesions Viral replication is a complex process comprising of a number of steps – adsorption/penetration, uncoating, transcription, synthesis of viral components, assembly and finally release of new virons. Anti viral agents Relatively few antiviral drugs have been developed compared to the number of antibacterial drugs, this is due to the intracellular nature of the infection and the ability of the viruses to establish a latent form. Acyclovir was the first antiviral drug to be discovered It enters into the viral infected cell and bibds to the viral DNA preventing its further replication. Hence it should be given preferably within 48 hours of onset of acute symptoms. Valaciclovir, penciclovir, famciclovir. Docosanol is an agent which alters the cell membrane to prevent the viral entry and this is available as topical application for herpes simplex infection. Laboratory diagnosis Electron microscopy can be used to provide identification of virus based on morphological appearance but this has low specificity and requires additional tests. Light microscopy in conjuction with immunofluorescence and monoclonal antibodies can be used to give rapid and accurate results. Viruses can be grown in tissue culture, the swab of the lesion should be carefully transported with addition of antibiotics and antifungals to prevent the overgrowth of bacteria and fungus. Diagnosis can be confirmed retrospectively by detection of high rise in antibody titre. HUMAN HERPES VIRUS [HHV] HHV1 – Herpes simplex virus 1 HHV 2 - Herpes simplex virus 2 HHV 3 – Varicella zoster virus HHV 4 – Epstein barr virus HHV 5 – Cytomegalo virus HHV 6 HHV 7 HHV 8 – Kaposi sarcoma virus Herpes Simplex Virus It is a DNA virus, two types are seen - Type 1 & 2 HSV 1 is spread predominantly through the saliva or active perioral lesions Seen more commonly on lips, eyes and skin above the waist HSV 2 is seen more in genital areas and is transmitted predominantly through sexual contact. Clinical lesions produced by both types are identical The initial exposure to an individual is called as primary infection, this is seen at a very young age and is often asymptomatic. The virus travels along the sensory nerves and reaches the associated ganglion and becomes inactive [trigeminal ganglion in oral HSV infection] Secondary [recurrent, recrudescent ] infection occurs by reactivation of the virus. Numerous conditions like old age, pregnancy, emotional stress, trauma, allergy, systemic disease etc can cause reactivation of this virus Herpes Simplex Virus Acute gingivostomatitis is the most common manifestation of symptomatic primary HSV. symptoms like fever, nausea, chills etc are seen Most of the acute herpetic gingivostomatitis arise between the ages of 6 months to 5 years. Initially the affected mucosa develops small vesicles which enlarge slightly and develop into ulcers. When primary infection is seen in adults it usually results in pharyngotonsillitis. Secondary or recurrent infections are seen either at the site of primary inoculation or adjacent sites which are supplied by the involved ganglion. The most common site of recurrence is the vermillion border of lips known as – Herpes labialias . Lesions on the oral mucosa are seen limited to the keratinized mucosa. Herpetic whitlow Herpes Gladiatorum. Histological features Epithelial cells show achantholysis, nuclear clearing and nuclear enlargement [Balooning degeneration] Tzank cells Intra nuclear inclusions – Lipshutz bodies Lab diagnosis Treatment – Acyclovir is the drug of choice, valacyclovir, famicyclovir topical anesthetic corticosteroids should not be prescribed to the patients. Varicella Infection Varicella zoster virus – VZV ; HHV 3 It also has a primary and secondary infection like HSV Primary infection – Chicken pox Secondary infection – Herpes Zoster Chicken pox – this virus spreads by air droplets or direct contact Incubation period – 10 – 21 days Prodormal - Malaise, pharyngitis & rhinitis Rash begins on the face & spreads to the extremities. Each lesion progresses through the stages of Erythema – vesicle – pustule – crust “Dewdrop on rose petal” is the classical presentation seen due to presence of a vesicle with erythema. Oral lesion are seen on the palate and buccal mucosa frequently, oral lesions look like HSV lesion but the most important distinguishing feature is that the lesions of chicken pox are painless. Complications- reye’s syndrome, encephalitis, pneumonia etc Histologic features – Same as HSV Treatment – Warm baths with soap Acyclovir, valacyclovir, famicyclovir Herpes Zoster After initial infection, the virus becomes inactive and is present in the nerve ganglion. Reactivation of the virus can occur due to various reasons, but unlike HSV multiple recurrences are seen in herpes zoster infection. Clinical features: the infection has three phases – Prodrome, acute and chronic Severe neuralgia is the most common prodromal symptom, the pain is severe – burning or stabbing type. Fever, malaise and headache may also be seen. The acute phase is characterized by appearance of vesicles on an etythematous base, in 3-4 days the vesicles become pustular, ulcerate and crust. The lesions tend to occur along the course of the nerve and terminate at the midline. Oral lesions are also seen along with the skin involvement. If pain persists for mare than 3 months after the initial presentation it is chronic phase and is called as ‘postherpetic neuralgia’ Herpes Zoster James Ramsay Hunt syndrome: facial nerve paralysis, deafness, vertigo, and pain. Due to infection of the geniculate ganglion. Zoster sine herpete – some patients may develop the neuralgic pain but the lesions are not seen. This condition is very difficult to diagnose and maybe misdiagnosed as dental problem, migraine, myocardial infarction or appendicitis depending on the involved dermatome. Infectious Mononucleosis Caused by Epstein-barr virus –HHV 4 This is known to spread through intimate contact. Infection in children is asymptomatic. In adults fever, lympadenopathy, tonsillitis, pharyngitis. The fever may reach 1040 F Oral lesions include petichae on the hard and soft palate. Necrotizing ulcerative gingivitis may also be seen. Oropharyngeal tonsillar enlargement is seen, parotid gland enlargement with facial nerve palsy is also reported. Classic serological test for infectious mononucleosis is the “Paul-bunnell test” Cytomegalovirus –HHV 5 Primary infection followed by secondary infection due to reactivation Establishes latency in salivary gland cells, endothelium, macrophages & lymphocytes Almost 90% of cases are asymptomatic Adult clinical infection resembles infectious mononucleosis Oral lesions are seen in AIDS (mucosal ulcers) Neonatal – hypoplasia, attrition, yellow coloration of dentin Histologic features: infected cells are enlarged and have prominent nucleoli - “owl eye” alteration. Coxsakie Virus Belongs to group of enterovirus Herpangina – A1-6,8,10,22 Hand foot & mouth – A16 Acute lymphonodular pharyngitis – A10 Measles (Rubeola) Paramyxovirus Incubation period of 10 days, patient becomes infectious 2 days before becoming symptomatic and untill 4 days after appearance of rash Prodormal symptoms are followed by a rash – face is involved first Complications like otitis, pneumonia, diarrhea Oral manifestations – “Koplik’s spots” are the most distinctive oral manifestation. Areas of erythema with small bluish white macules Enamel hypoplasia of the pitted type is also seen Enlargement of lingual and pharyngeal tonsils Histologic features: large number of neutrophils and lymphocytes. Large multinucleated Warthin – Finkeldey giant cells are seen. Mumps Paramyxovirus infection that primarily affects salivary gland Incubation period of 16 -18 days Spreads through saliva, respiratory droplets Contagious from 1 day before appearance to 14 days after clinical resolution of the infection Low grade prodormal symptoms of 1 day followed by salivary gland changes, Parotid gland is most common, discomfort and swelling are seen in the region around the ear. Enlargement peaks within 2-3 days and is most painful during this period. Enlargement of the glands usually begins on one side and is followed by contralateral gland enlargement. The second most common finding is epididymoorchitis – testicle exhibits rapid swelling with pain and tenderness. Oophoritis & mastitis are also seen Redness and enlargement of stensons and whartons duct MMR vaccine Treatment of mumps is pallative in nature Acquired Immunodeficiency Syndrome [AIDS] Caused by human immunodeficiency virus – HIV The primary target of HIV is CD4+ helper T cells HIV infection is may be asymptomatic or an acute viral response may be seen . The acute viral response develops within 1-6 weeks after the exposure, the symptoms resemble infectious mononucleosis, oral changes include mucosal erythema and focal ulcerations. This acute phase clears within a few weeks, followed by a variable asymptomatic period. Some patients develop a phase of chronic fever, weight loss, diarrhea, oral candidiasis, herpes zoster, oral hairy leukoplakiathis has been termed as AIDS related complex [ARC] This is followed by development of overt AIDS, the presentation is highly variable. The signs and symptoms of ARC are all seen along with increasing number of opportunistic infections and neoplastic processes. Oral manifestations of AIDS Group 1 – (Strongly associated) Candidiasis Hairy leukoplakia Kaposi’s sarcoma Non hodgkins lymphoma Periodontal disease Linear gingival erythema NUG NUP Oral manifestations of AIDS Group 2 – (commonly associated) Bacterial infections Tuberculosis Melanotic hyperpigmentation Necrotizing stomatitis Group 3 – (seen) Apthous ulcerations Verruca vulgaris; squamous papollioma Histoplasmosis Thrombocytopenia



![Info. Speech Packet [v6.0].cwk (DR)](http://s3.studylib.net/store/data/008110988_1-db39bdd1f22b58bf46d9a39ab146e2e3-300x300.png)