week 2-3
advertisement

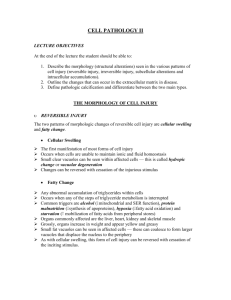
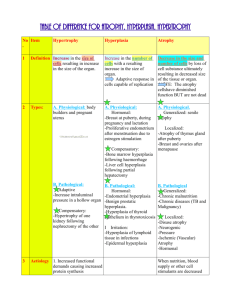
CELL INJURY & CELL ADAPTATIONS DR. SALEEM SHAIKH Introduction Cell injury is defined as a variety of stresses a cell encounters as a result of changes in its internal & external environment. The cells of the body have inbuilt mechanism to to resist the changes. The response of a cell to changes depends upon The type of cell involved The type of injury / stress The etiology of cell injury may be broadly classified into Genetic causes Acquired causes Acquired causes Hypoxia & ischemia – deficiency of oxygen; due to lack of blood supply. (may be other causes of hypoxia) 2. Physical agents – mechanical, thermal, electrical etc 3. Chemical agents – medications, smoke, drugs etc 4. Microbial agents – bacterial, viral fungi etc 5. Immunologic agents – ‘double edged sword’ hypersensitivity reactions, anaphylactic shock 6. Nutritional derangements – both reduced and in excess 7. Ageing – decreased ability for cell repair 8. Psychogenic causes 9. Iatrogenic factors 10. Idiopathic diseases 1. Morphology of cell injury Morphology of reversible cell injury – also called as retrogressive changes Types of changes Hydropic change (cloudy swelling) Hyaline change Mucoid change Hydropic change This is due to accumulation of water within the cytoplasm of the cell. The most commonest and early form of cell injury resulting from acute cell injury from bacterial toxins, chemicals, burns etc Pathogenesis – defective regulation of sodium and potassium at the cell membrane, which results in rapid flow of water into the cell. Microscopically the cell appears to be swollen, small clear vacuoles are seen hence called as vacuolar degeneration. nucleus appears pale. Hyaline change hyaline - glass. This refers to the non specific homogenous pink material which is seen in H&E stained sections. It may be intracellular or extracellular. Russels bodies in plasma cell, hyalinised old scar, hyaline deposits in blood vessels in hypertension and diabetes. Mucoid change Mucus is produced mainly by epithelium and by some cells in connective tissue. Mucin is the main constituent. Excess mucin accumulation in connective tissue is known as myxoid and is seen in tumors of odontogenic and salivary gland origin. Morphology of Irreversible Cell Injury Irreversible cell injury leads to cell death. Types of cell death Necrosis Apoptosis Changes that follow cell death Gangrene Calcification Finally results in end of life Necrosis Necrosis is defined as a localised area of death of tissue followed by degradation of tissue by hydrolytic enzymes, it is always accompanied by inflammatory reaction. Can be caused by various agents like hypoxia, physical, chemical etc Two important changes seen are Cell digestion by lytic enzymes – seen as homogeneous and eosinophilic cytoplasm Protein denaturation – seen as changes in the nucleus (condensation – pyknosis; dissolution – karyolysis; fragmentation- karyohexsis) Types of necrosis Coagulative necrosis – most common, caused by ischemia. The cell outlines are retained but the cytoplasmic and nuclear details are lost. Liquefactive necrosis – Also commonly seen, this occurs due to degradation of tissues by hydrolytic enzymes Fat necrosis – seen in pancreas and breasts Fibrinoid necrosis – deposition of fibrin like material, seen in immunologic tissue injury Caseous necrosis – Found as center foci in tuberculosis infections. Combines features of both coagulative and liquefactive necrosis Apoptosis Apoptosis is a form of ‘coordinated and internally programmed cell death’ This form of cell death is controlled and regulated and is also referred as cell suicide Apoptosis is seen in both physiologic and pathologic conditions Presence of apoptotic bodies Physiologic process Organized shape modification in development of embryo Physiologic involution of tissues Involution of thymus Pathologic process Cell death by cytotoxic T cells Degenerative diseases of CNS – Alzheimer’s Some types of viral infections Difference chart Gangrene Gangrene is a advanced stage of necrosis which also shows putrefaction (production of foul odor). Two main forms of gangrene Dry - this is seen in the distal part of the limb due to ishemia, usually in toes and feet of old patients with atherosclerosis. The blood supply to the part is very less. A line of seperation is seen between the normal part and the gangrene part Wet – (gas gangrene) – seen in moist tissues such as mouth, bowel, lung etc. Diabetic foot and bed sores are also common examples. This is seen due to blockage of venous blood flow. No line of demarcation is seen. Gas gangrene is a variant of wet gangrene formed due to gas producing bacteria (clostridia). Seen in open and contaminated wounds. Pathologic Calcifications Deposition of calcium in tissues other than teeth or bone is called pathologic calcification. Two types Dystrophic – deposition in dead and degenerated tissues, with normal calcium metabolism and calcium levels. Ex- infarcts, thrombi, old scars Metastatic – deposition in normal tissues with deranged calcium metabolism and hypercalcaemia. Ex – kidney stones, lung, blood vessels etc. CELLULAR ADAPTATIONS When a cell is exposed to stress, the cells make adjustments in order to survive. This adaptation could be to physiologic or pathologic adaptation. In general the adaptive responses are reversible on withdrawal of stimulus. The cells may change by Increase or decrease in number Change in appearance and structure Atrophy Reduction in number and size of parenchymal cells of an organ or its parts which was once normal. Hypoplasia – developmentally small Causes – Physiologic Atrophy of thymus Atrophy of gonads after menopause Atrophy of brain after aging Pathologic Ischaemic atrophy Disuse atrophy Endocrine atrophy Pressure atrophy Hypertrophy Increase in the size of parenchymal cells without any change in number of the cells Physiologic enlarged size of uterus during pregnancy Muscular hypertrophy in athletes Pathologic – Hypertrophy of cardiac muscle Compensatory hypertrophy Hypertrophy of smooth muscle Hyperplasia Hyperplasia is an increase in the number of parenchymal cells. Very often hyperplasia and hypertrophy occur together Hyperplasia persists only till the stimulus is present (different from neoplasia) Physiologic hyperplasia – Hormonal hyperplasia – puberty Pathologic hyperplasia – excessive stimulation of hormones Excess granulation tissue during wound healing Formation of skin warts Metaplasia It is the change of one type of adult cell to another type of adult cell, usually as a response to stimulus and reverts back to normal after removal of stimulus Types Epithelial Mesenchymal Epithelial is the more common type, usually the cell becomes less specialized bronchus of smokers- pseudo stratified ciliated columnar to squamous. sialometaplasia – mucous salivary gland acini to squamous Bronchitis – pseudo stratified ciliated to coulmnar Mesenchymal metaplasia – Osseous metaplasia – myositis ossificans; riders bone Cartilaginous metaplasia - healing of fractures Dysplasia Disordered cellular growth (bad growth) It is characterized by Increased layer of epithelial cells Disordered arrangement of cells Loss of basal polarity Cellular and nuclear pleomorphism Increased nucleocytoplasmic ratio Nuclear hyperchromatism Increased and abnormal mitotic activity Very common in oral cavity Classified as mild moderate and severe CARCINOMA IN SITU 1 2 3 4