pathophysiology 5
Repair and Regeneration
Tissue Repair and Regeneration
may start early after tissue damage
• 1. Regeneration
– Restoration of original tissue architecture and function
– by parenchymal cells of the same type
• 2. Repair
– Replacement by connective tissue ( scarring )
– There will be alterations in both architecture and function
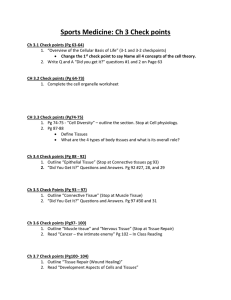
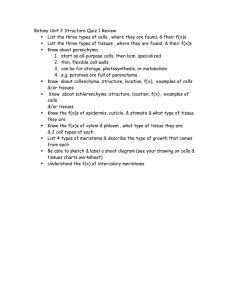
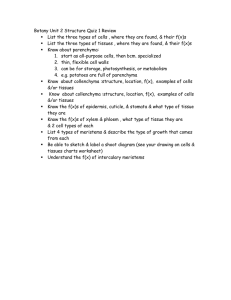
Regeneration: Cell requirements
CELLULAR PROLIFERATION
Tissues of the body are divided into three groups:
• Continuously dividing (labile) tissues
• Stable tissues
• Permanent tissues
Tissue types
1 . permanent
• nonproliferative in postnatal life
• neurons , cardiomyocytes
2 . stable
• regeneration as response to injury
• parenchyma – liver, pancreas, renal tubule
3 . labile
• continuous regeneration from stem cells (self-renewal)
• hematopoietic cells in bone marrow
• surface epithelia – skin, oral cavity, vagina, cervix
• duct epithelia – salivary glands, pancreas, biliary tract
• mucosas – GIT, uterus, fallopian tubes, urinary bladder
CELLULAR PROLIFERATION
Tissues of the body are divided into three groups:
• Continuously dividing (labile) tissues
• cells are continuously proliferating
• can easily regenerate after injury
• contain a pool of stem cells
• examples: bone marrow, skin, GI epithelium
CELLULAR PROLIFERATION
• Stable tissues
• cells have limited ability to proliferate
• limited ability to regenerate (except liver!)
• normally in body, but can proliferate if injured
• examples: liver, kidney, pancreas
CELLULAR PROLIFERATION
• Permanent tissues
• cells can’t proliferate
• can’t regenerate (so injury always leads to scar)
• examples: neurons, cardiac muscle
The Cell Cycle and Different Cell Populations
The parenchyma are the functional parts of an organ in the body.
This is in contrast to the stroma , which refers to the structural tissue of organs, namely, the connective tissues.
Organ brain heart kidney liver lungs pancreas spleen
Parenchyma neurons and glial cells myocyte nephron hepatocyte
Lung parenchyma
Islets of Langerhans and Pancreatic acini white pulp and red pulp
Regeneration: Hindrances
• Destruction of stroma
– disturbed proliferation of parenchymal cells
– Replacement of stroma
• Excessive exudation/infection
• Polymorphonucleocytes(PMNs) secrete numerous proteases.
• Bacteria often have similar enzymes or toxins.
• Excessively large defects
• Permanent cells
Repair
• When the requirements for regeneration are not met, then the gaps produced by lost cells heal by connective tissue replacement
• Repair by
1) fibrous tissue or
2) connective tissue or
3) granulation tissue.
Replacement of necrotic tissue
• resorption by macrophages
• dissolution by enzymes
• replacement by granulation tissue
– The steps are:
1. angiogenesis
2. migration and proliferation of fibroblasts
3. deposition of Extracellular matrix ( ECM)
4. maturation and reorganization
Repair by Connective Tissue
• Conditions for regeneration are not met
• Four components to this process:
1. Formation of new blood vessels (angiogenesis)
2. Migration and proliferation of fibroblasts (fibroblast is a type of cell that synthesizes the extracellular matrix and collagen, the structural framework )
3. Deposition of Extracellular matrix , synthesis of collagen
(scar formation)
4. Maturation, contraction, and organization of fibrous tissue (remodeling of scar)
Pathological aspects of healing
• proud flesh (caro luxurians)
– excessive amount of Granulation tissue(GT)
• keloid
– excessive amount of collagen
• hyaline plaques
– serous membranes (spleen, pleura)
Complications of wound healing
• Deficient scar formation
– Wound dehiscence (premature "bursting" open of a wound along surgical suture)
– Ulceration
• Excessive formation of scar tissue
– Keloid (excessive collagen deposition)
– Desmoid (aggressive fibromatosis, semi-malignant)
• Contracture
Wound dehiscence
Wound ulceration
Keloid
Contracture
Factors that influence wound healing
I. Systemic factors
• Malnutrition
– Protein deficiency
– Vitamin C deficiency (inhibition of collagen synthesis)
• Metabolic status
– e.g Diabetes mellitus
• Consequence of microangiopathy
– Cortison treatment
• inhibits inflammation and collagen synthesis
• Circulatory status
– Inadequate blood supply due to ateriosclerosis
– Varicose veins (retarded venous drainage)
Factors that influence wound healing
II. Local Factors
• Infection (single most important reason for delayed wound healing)
• Foreign bodies
– suture material, bone and wood splinters ….
• Mechanical factors
– Early movement
– Pressure