Document 15355975
advertisement

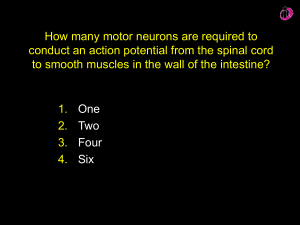
AUTONOMIC NERVOUS SYSTEM Terminologies for ANS • Anatomically: – Thoracolumber outflow(T1-L2) – Craniosacral outflow(III, VII, IX, X, S1-S3) • Physiologically: – Sympathetic – Para sympathetic • Pharmacologically: – Adrenergic – Cholinergic Somatic Vs ANS Organization of ANS • Central component: 1. Brainstem 2. Hypothalamus 3. Spinal cord • Peripheral component: 1. Nerves 1. 2. Sympathetic Parasympathetic • Ganglia: 1. Vertebral 2. Paravertebral 3. Terminal Role of ANS Maitain homeostasis by maintaining a dynamic antagonism b/w sympathetic & parasympathetic divisions of ANS • Parasympathetic (D) – Digestion – Defecation – Diuresis • Sympathetic (E) – – – – Exercise Excitement Emergency Embarrassment • Sympathetic system: – Short preganglionic fiber – Long postganglionic fiber • Parasympathetic system: – Long preganglionic fiber – Short post ganglionic fiber Autonomic neurotransmitters • Acetylcholine (Cholinergic fibers) – All preganglionic fibers – All parasympathetic postganglionic fibers • Adrenaline (Adrenergic fibers) – Most sympathetic postganglionic fibers Receptors • Acetylcholine: – Muscarinic • Membranes of effecter cell – Nicotinic • Synapse of pre & post ganglionic autonomic nerves • Adrenaline: – Alpha • Smooth muscles(contraction) – Beta • Smooth muscle(relaxation) Sympathetic nerve fibers in skelatal nerves • Some of the sympathetic postganglionic fibers pass back from sympathetic chain • These are C type fibers • Control – Blood vessels – Sweat glands – Piloerector muscle 8% of fibers in skeletal nerves are sympathetic Sympathetic nerve fibers in adrenal medulla • Preganglionic symp. Fibers pass without synapse in adrenal medulla. • Reach the specialized secretory cells which secrete epinephrine & nor epinephrine. Thank you Functions of ANS Sympathetic nervous system Catabolic Parasympathetic nervous system Anabolic Preserve energy in the body (i.e. save Increases energy expenditure of the body. energy in the heart and offer it in the intestine). Prepares the body for activity, increasing Predominates during sleep where there the capacity to perform sever muscular are continuous digestion, slow heart rate effort (fight and flight) in response to and constricted pupil. stress (emergency situations). Delay onset of fatigue of contracting Allow for repair and muscles contracting muscles. Sympathetic mass stimulation is useful recovery of Parasympathetic mass stimulation is fatal. Eyes • Pupillary opening – Sympathetic system: • Contracts meridional fibers--- pupillary dilatation – Parasympathetic system: • Contracts the circular muscles---- pupillary constriction • Focus of lense: – Parasympathetic: • Contracts ciliary muscles---- release of tension in lense ligament---- convex---- accomodation Glands • Nasal, lacrimal, salivary & gastrointestinal glands • Parasympathetic---- increased secretion • Sympathetic ---- concentrated secretions(enzymes & mucous) • Sweat glands: cholinergic sympathetic fibers---- increased secretion – Stimulated by centers in hypothalamus • Apocrine glands – Supplied by sympathetic fibers – Stimulation secretes thick, odriferous & lubricant secretion GIT • Parasympathetic: – Increases motility – Sphincters relax – Increased secretion of glands • Sympathetic: – Strong stimulation • Inhibits peristalsis • Increased sphincters tone (1) GIT • (Stomach, small intestine and proximal part of large intestine) • Relaxation of their walls and contraction of their sphincters leading to inhibition of digestion and delayed evacuation of their contents. (2) Liver: • Stimulation of glycogenolysis leading to increased blood glucose. • Stimulation of fibrinogen synthesis. (3) Gall bladder: • contraction of wall and relaxation of sphincter of Oddi, helping its evacuation. (4) Spleen: • Contraction of smooth muscles in splenic capsule and trabeculae leading to pouring of about 250 ml of stored blood into the general circulation. (5) Pancreas: • Sympathetic stimulation usually inhibits pancreatic secretion (both endocrine and exocrine components). (6) Blood vessels • Mixed supply (vasoconstriction and vasodilatation). (7) Kidneys: • Stimulation of juxta glomerular cells leading to increased renin secretion. • Decrease renal blood flow. • Decrease urine output. Sympathetic origin LHCs of T6-12 segments of spinal cord (splanchni c nerves). Relay Collateral ganglia (celiac, superior mesenteric, aortico-renal) and terminal ganglia (1) GIT • (Stomach, small intestine and proximal part of large intestine) • contraction of their walls and relaxation of their sphincters enhancing both digestion and evacuation of GIT contents i.e. help deglutition, gastric motility, and peristaltic movement of GIT. (2) Liver: • increased hepatic bile flow. (3) Gall bladder: • Relaxation of its wall and contraction of sphincter of oddi leading to retention of bile and delayed emptying of gall bladder. (4) Pancreas: • Parasympathetic stimulation usually stimulates pancreatic secretion (both endocrine and exocrine components). (5) Blood vessels • Vasodilatation. (6) Glands: • Stimulation of gastric juice secretion (rich in HCl). • Stimulation of alkaline mucus secretion from Bruner's glands in the duodenum. Parasympatheti c origin Dorsal motor nucleus of the vagus Relay Terminal ganglia in the wall of abdominal organs Action of sympathetic on Suprarenal medulla Origin: LHCs of T10,11 segments of spinal cord. * SRM has special character being supplied by sympathetic preganglionic nerve fibers (with no postganglionic nerve fibers) which relay there on special neurosecretory cells (chromaffin cells). * Stimulation of sympathetic nerves to SRM releases large quantities of adrenaline (80%) and noradrenaline (20%) into the circulating blood, being carried to all body tissues. These hormones has prolonged action due to their slow clearance from the circulation. - Adrenaline acts more on metabolic actions of the body while noradrenaline acts more on blood vessels. - In stress conditions, SRM acts together with sympathetic nervous system (sympatho-adrenal system). Heart (CVS) Sympathetic • Increased HR • Increased FOC • Increased resistance • Vasoconstriction in abdomin & skin Parasympathetic • Decreased HR • Decreased FOC • Decreased resistance • Little effect on vessels Sympathetic Parasympathetic Origin LHCs of upper 4 or 5 thoracic segments Dorsal Motor nucleus of the vagus of spinal cord Relay Cervical ganglia (superior, middle and Terminal ganglia in the wall of the heart inferior) and upper 4 thoracic ganglia and lung a) Sympathetic stimulation increases the Parasympathetic stimulation decreases effectiveness of the heart as a pump i.e. the effectiveness of the heart as a pump increasing the rate, force of heart i.e. decreasing the rate, force of heart contraction, Action on the heart conduction velocity, contraction, conduction velocity, excitability, cardiac metabolism and O2 excitability, cardiac metabolism and O2 consumption. consumption. b) Coronary vessels: Direct effect is Coronary vessels : Direct effect is vasoconstriction. Indirectly the coronary vasodilatation. Vagal stimulation inhibits vessels dilate as a result of accumulation cardiac work with less production of of metabolites of the stimulated heart. metabolites. Thus the coronary vessels indirectly constrict (vasoconstriction). N.B.: Parasympathetic does not supply the ventricles. SYMPETHETIC PARASYMPETHETIC a) inhibition of the smooth a) Motor to the smooth muscles of the bronchial muscles of the bronchial tree tree Action of the lungs resulting bronchodilatation in resulting in bronchoconstriction. b) inhibition of the mucus b) secretion of air passages. c) vasoconstriction of the pulmonary blood vessels. secretion of the air passages. c) Stimulate the Vasodilatation mucus of pulmonary blood vessels. the Actions on Pelvis Sympathetic Parasympathetic Origin LHCs of L1, L2, L3 segments of spinal cord. Sacral segments 2, 3, 4 (preganglionic forms pelvic nerve) Relay Collateral ganglia (inferior mesenteric or hypogastric ganglia) and terminal ganglia Action on Urinary bladder Contraction of its wall and relaxation of relaxation of its wall and contraction of internal urethral sphincter leading to internal urethral sphincter leading to micturition. urine retention. Terminal ganglia in the wall of the pelvic organs relaxation of its wall and contraction of Contraction of its wall and relaxation of anal sphincter leading to internal anal sphincter leading to retention. defecation. Action of internal the rectum Action of male sex organs Action of a) Contraction of smooth muscles in a) Vasodilatation of the blood vessels of the walls of seminal vesicle, the pelvic viscera including that of sex epididymis, vas deferens and organs leading to erection of the penis, ejaculatory duct leading to ejaculation clitoris, etc. and congestion of the of semen. labia. So, the pelvic nerve is named as b) Vasoconstriction of blood vessels of the nervus erigenus. pelvic viscera including those of b) Secretory to the seminal vesicles, external sex organs leading to prostate and other accessory glands. shrinkage of penis. a) Vasoconstriction of blood vessels of Sympathetic (I) Antagonistic functions: 1- Pupil: Mydriasis. 2- Air passages. bronchodilatation. 3- Heart rate Parasympathetic Miosis. bronchoconstriction. rate contraction coronary blood flow contraction coronary blood flow 4- GIT: - Wall - Sphincter - Blood vessels 5- Rectum relaxation contraction vasoconstriction retention of faeces contraction relaxation vasodilatation defecation 6- Urinary bladder 7- blood vessels retention of urine Vasoconstriction Micturition vasodilatation (II) Synergistic function: (During salivary secretion) Trophic salivary secretion (little, viscid, rich in enzymes) True salivary secretion (large in volume, watery, rich in electrolytes) N.B.: Augmented secretion Stimulation of sympathetic to salivary glands after parasympathetic stimulation leads to augmented secretion due to active squeeze of acini as a result of sympathetic stimulation of myoepithelial cells surrounding acini (which are filled with secretions by parasympathetic stimulation). (III) Cooperative functions: (During sexual intercourse) * Contraction of vas deference, seminal vesicle, * Secretory to seminal vesicle and prostate. ejaculatory duct; producing ejaculation of semen. * Erection of penis and clitoris due to * Shrinkage of penis and clitoris due to vasodilatation. vasoconstriction